Team Charter for Schedule to Day of Surgery
advertisement
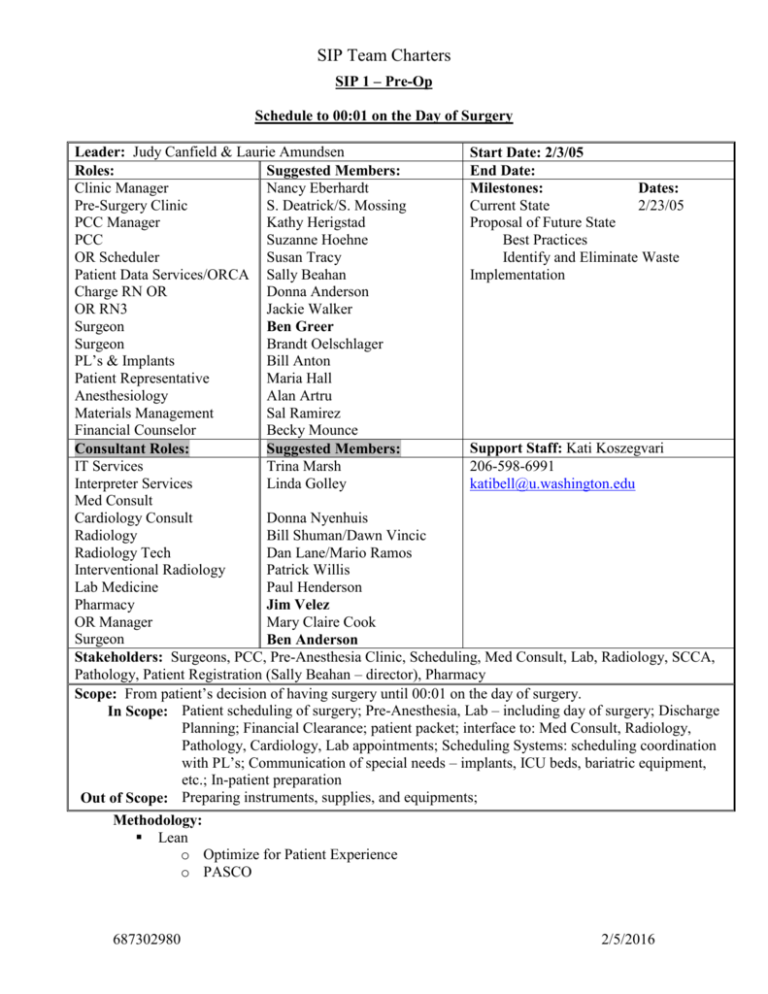
SIP Team Charters SIP 1 – Pre-Op Schedule to 00:01 on the Day of Surgery Leader: Judy Canfield & Laurie Amundsen Start Date: 2/3/05 Roles: Suggested Members: End Date: Clinic Manager Nancy Eberhardt Milestones: Dates: Pre-Surgery Clinic S. Deatrick/S. Mossing Current State 2/23/05 PCC Manager Kathy Herigstad Proposal of Future State PCC Suzanne Hoehne Best Practices OR Scheduler Susan Tracy Identify and Eliminate Waste Patient Data Services/ORCA Sally Beahan Implementation Charge RN OR Donna Anderson OR RN3 Jackie Walker Surgeon Ben Greer Surgeon Brandt Oelschlager PL’s & Implants Bill Anton Patient Representative Maria Hall Anesthesiology Alan Artru Materials Management Sal Ramirez Financial Counselor Becky Mounce Support Staff: Kati Koszegvari Consultant Roles: Suggested Members: IT Services Trina Marsh 206-598-6991 Interpreter Services Linda Golley katibell@u.washington.edu Med Consult Cardiology Consult Donna Nyenhuis Radiology Bill Shuman/Dawn Vincic Radiology Tech Dan Lane/Mario Ramos Interventional Radiology Patrick Willis Lab Medicine Paul Henderson Pharmacy Jim Velez OR Manager Mary Claire Cook Surgeon Ben Anderson Stakeholders: Surgeons, PCC, Pre-Anesthesia Clinic, Scheduling, Med Consult, Lab, Radiology, SCCA, Pathology, Patient Registration (Sally Beahan – director), Pharmacy Scope: From patient’s decision of having surgery until 00:01 on the day of surgery. In Scope: Patient scheduling of surgery; Pre-Anesthesia, Lab – including day of surgery; Discharge Planning; Financial Clearance; patient packet; interface to: Med Consult, Radiology, Pathology, Cardiology, Lab appointments; Scheduling Systems: scheduling coordination with PL’s; Communication of special needs – implants, ICU beds, bariatric equipment, etc.; In-patient preparation Out of Scope: Preparing instruments, supplies, and equipments; Methodology: Lean o Optimize for Patient Experience o PASCO 687302980 2/5/2016 SIP Team Charters Outcome Characteristics 1. Safe and patient-centered care 2. Scientific modeling for case accuracy 3. Collect accurate patient data once, retain and disseminate 4. Universally accessible patient data 5. Staff, equipment, OR, ready for patient on arrival 6. Patient ready on arrival 7. Scheduling by code or code group that delivers time estimate, equipment, special staffing, and essential service resource needs 8. Robust and flexible yet highly efficient Outcome Deliverables 1. Document current state process(es) 2. Document best industry practices 3. Value analysis using LEAN methodology a. Identification of optimal patient flow (patient experience) b. Identification of optimal information flow c. Identification of essential variability 4. Design future state process(es) 5. Develop project plan and timeline a. Identify short and long term projects 6. Develop metrics and key indicators 7. Short and long term project completion 8. Strategy for ongoing Performance Improvement Essential Metrics Patient ready upon arrival All resources ready upon arrival Block time utilization Planned schedule same as actual schedule Project Support Lean Expert; EPIC Expert Resources 687302980 2/5/2016 SIP Team Charters SIP 2 – First Case Day of Surgery: 00:02 to Incision First Case Leader: Kevin Smith Roles: PL’s/Equipment & C-Core Anesthesiology Anesthesiology RN Pavilion Pre-OP RN Main Pre-OP RN OR RN3 Patient Representative Ambulatory Surgery Manager Surgical Tech Instrument Room Hospital Assistant E Surgeon (Ortho) Surgical Resident (Ortho) Consultant Roles: Suggested Members: Jason Jio Karen Domino Karen Souter Susan Grant Dori Nelmark Vicki Sandeen Sonja Borthen Terry Way Renae Burchiel-Battie Mike Amos George Davis Abdul Ramzan Kevin Smith TBD Suggested Members: Start Date: 2/2/05 End Date: Milestones: Dates: Current State 2/23/05 Proposal of Future State Best Practices Identify and Eliminate Waste Implementation Staff Support: Ruth Oskolkoff Materials Management Kathy Ritter 206-598-6300 Surgeon (CV) Gabe Aldea rosk@u.washington.edu Surgeon (Ophthalmology) D. Sapperstein R2 OR Charge Nurse Janet Link Otolaryngology Kevin Kiemele Pharmacy Shabir Somani Admitting Jason Metcalf Stakeholders: Pavilion Pre-op, Main Pre-op, Admitting, Anesthesia, Materials Management, Surgeons, Main OR RN, Pavilion OR RN, Registration Scope: All support activities needed to prepare the resources necessary for surgery before the 1st patient enters the OR at 7:25 am. In Scope: Day ahead prep; Patient check-in; Preparing instruments, supplies, equipments; Room setup; Preparing the 1st patients for surgery; Transport; Anesthesia; documentation compliance and regulatory issues Out of Scope: All labs or patient centered activities except patient check-in and flow on the day of surgery Methodology: Lean o Optimize for Patient Experience o PASCO Outcome Characteristics 1. Safe and patient centered care 2. Compliant with all regulatory requirements 3. All cases start on time a. Zone concept or evolutionary equivalent 4. Minimal unanticipated schedule changes 687302980 2/5/2016 SIP Team Charters 5. Management plan for schedule changes 6. Plan for transplant and emergent cases Outcome Deliverables 1. Document current state process(es) 2. Document best industry practices 3. Value analysis using LEAN methodology a. Identification of optimal patient flow (patient experience) b. Identification of optimal information flow c. Identification of essential variability 4. Design future state process(es) 5. Develop project plan and timeline a. Identify short and long term projects 6. Develop metrics and key indicators 7. Short and long term project completion 8. Strategy for ongoing Performance Improvement Essential Metrics: More accurate delay codes Resource checklist Project Support: Lean Expert; Resources: 687302980 2/5/2016 SIP Team Charters SIP 3 – Last Case Day of Surgery: After Incision for First Case to Midnight Leader: Peter Buckley & Mary Claire Cook Start Date: 2/2/05 Roles Suggested Members: End Date: OR Manager Mary Claire Cook Milestones: Dates: OR Charge Nurse Jim Henkleman Current State 2/23/05 Frontline OR Nurse Proposal of Future State PACU Main Charge RN Mary Mentele Best Practices R2 PACU RN Kim Owen Identify and Eliminate Waste R2 OR MA Kenneth Marbury Implementation PACU Manager Shelley Deatrick Surgeon (Plastic) Jana Cole Surgeon Al Hillel Hospital Assistant PACU Jason Dela Cruz Pavilion RN3 Loretta Stesco Materials Management Leslie Bahr Anesthesiology Karen Domino Patient Representative Mike Smith Main Pre Op RN Gale Uhlenkott Staff Support: Virginia McClure Consultant Roles: Suggested Members: Radiology B. Shuman/Dawn Vincic 206-598-4260 Pharmacy Steve Bird vmcclure@u.washington.edu IP Unit Manager, 6SE Judi Hubbard PCS Director Sherri Del Bene Pathology Melissa Upton Environmental Services Craig Saran Patient Flow Supervisor Shauna Andrus Pavilion C-Core Stakeholders: Pavilion Pre-op, Main Pre-op, Admitting, Anesthesia, Materials Management, Surgeons, Main OR RN, Pavilion OR RN, Registration, HA, ES, PACU Scope: Logistics for all non-first cases In Scope: Patient check-in through holding; Documents/results ready; Procedure time; Turnover; Non-black case management (TBA, Urgent/Emergent); Coordination of rooms, instruments, supplies, and equipments between cases; Bed utilization; Surgeon/patient availability; Transport of patients; hours of staffing coverage; staffing; Family debriefing; Patient arrival time; team incentives; Out of Scope: 1st cases Methodology: Lean o Optimize for Patient Experience o PASCO Outcome Characteristics 1. Patient and family centered, safe a. No rescheduling of elective scheduled cases 2. Scheduled and case time approximate & appropriate 687302980 2/5/2016 SIP Team Charters 3. 4. 5. 6. 7. 8. Minimal "turnover time" Manage educational experience to maintain efficiency and productivity End of the day plan in place by the end of the first case or 9 am Available resources for throughput from OR to inpatient or DC Optimal strategy for urgent elective and emergent cases Highly efficient use of resources a. Efficient and consistent performance 24/7 Outcome Deliverables 1. Document current state process(es) 2. Document best industry practices 3. Value analysis using LEAN methodology a. Identification of optimal patient flow (patient experience) b. Identification of optimal information flow - staff, patient, AND family c. Identification of essential variability 4. Design future state process(es) 5. Develop project plan and timeline a. Identify short and long term projects 6. Develop metrics and key indicators 7. Short and long term project completion 8. Strategy for ongoing Performance Improvement Essential Metrics: Number of overhead pages lowered Patient Satisfaction Survey Project Support: Lean Expert; Resources: 687302980 2/5/2016 SIP Team Charters SIP 4 – Leadership/Culture Leadership and Culture Leader: Alan Artru & Dan Kaiser Start Date: 2/1/05 Roles: Suggested Members: End Date: Administration Lisa Brandenburg Milestones: Dates: Surgeon Doug Wood Current State 2/23/05 Surgeon Chris Wahl Proposal of Future State Surgery Resident Fred Cobey Best Practices CCE & Anesthesiology Gene Peterson Identify and Eliminate Waste Anesthesiology Peter Buckley/ E Kharasch Implementation Anesthesiology Karen Domino Anesthesia Tech/Hospital Assistant Joe Fitzgerald/Abdul Ramzan CRNA Gail Weiner RN Management Susan Grant Surgical Tech Neil Kovacs Frontline OR RN Melissa Marshburn Patient Representative Laura Gerber PACU Cindy Riplinger Inpatient Nursing Janice Cherin OD&T Kurt O’Brien Staff Support: Virginia McClure Consultant Roles: Suggested Members: HR Consultant Jennifer Petritz 206-598-4260 SOM Representative Julie Reid vmcclure@u.washington.edu Stakeholders: Surgeon; RN; Anesthesiologist; HA; ES; CRNA; Anesthesia Tech; C-Core; Surgical Tech; PreOp; PACU Scope: Activities within the Surgical Services In Scope: All cultural & leadership aspects within the walls of Surgical Services; Performance incentives; Out of Scope: Pre-Anesthesia Clinic; Surgical Clinics; Support Organizations; Methodology: Lean o Optimize for Patient Experience o PASCO Outcome Characteristics 1. Safe and patient and family centered care 2. Specific responsibilities and accountabilities 24x7 3. Inspired, accessible, knowledgeable leadership at all levels 4. Incentives for team development and participation 5. "Can do" attitude - for our patients and ALL of our customers 6. Consistent across all of surgical services, all day, every day 7. Interdisciplinary 8. Transparent 9. Professionalism Outcome Deliverables 1. Document current leadership and governance structure 687302980 2/5/2016 SIP Team Charters 2. Document best industry practices 3. Value analysis using LEAN and formal leadership evaluations 4. Design future state. Recommendations regarding future state: effective governance structure and VALUE a. Front line contributions, interdisciplinary and by consensus b. Rules, protocols, guidelines for recurring operational/staffing/culture issues 5. Ongoing leadership training 6. Strategy for ongoing optimization of Culture and Leadership - survival and succession strategy Essential Metrics: No bumps- every case finds a docking gate Same answer same question- any leader Patient Centered Project Support: Lean Expert Resources: 687302980 2/5/2016 SIP Team Charters SIP 5 – Strategic Planning Strategy/Strategic Planning Leader: Ed Walker & Ernie Weymuller Start Date: 1/31/05 Roles: Suggested Members: End Date: Administration Judy Canfield Milestones: Dates: Surgeon Dave Flum Current State 2/23/05 RN Susanne Loven-Skolnik Proposal of Future State Anesthesiology Peter Buckley Best Practices CRNA Mark Schierenbeck Identify and Eliminate Waste Finance Lisa Brandenburg Implementation Clinical Oversight Susan Grant Transplant Jorges Reyes Ambulatory Surgery Mgr Renae Burchiel-Battie Electronic Patient Record Andy Bowdle PACU RN Shelley Deatrick Patient Representative TBD Staff Support: Kimberly Knight Consultant Roles: Suggested Members: Quality Consultant Jim Perkins/Dave Flum 206-598-6090 Planning Con Helen Shawcroft kknight@u.washington.edu Baldridge Consultant Preston Simmons IT Services Tom Martin SOM Representative Julie Reid Stakeholders: Everyone in Surgical Services; Administration, UW Medicine Scope: All surgical patients through the continuum of the surgical process In Scope: Core services of the OR, future projections in coordination with or development of the current strategic planning (number of OR’s, sites, growth of business, business plan development, specialty growth); Capacity planning and impact analysis of all essential organizations; All evening and weekend cases; Marketing Out of Scope: Governance; Daily operations Methodology: Lean o Optimize for Patient Experience o PASCO Outcome Characteristics 1. Safe patient and family-centered care 2. Alignment of performance vs. incentives 3. Right sizing of ambulatory and complex case capacity for current and projected UW strategic planning goals 4. Graceful integration with hospital workflow that transcends traditional boundaries a. Optimal utilization of Pavilion resources b. IT infrastructure (e.g.) Electronic patient record in OR (e.g.) System-wide wireless patient tracking system 5. System for coordination with other UWMC strategic planning around capacity and specific program development 687302980 2/5/2016 SIP Team Charters 6. Standardized process for transplant cases 7. Standardized process for evening and weekend urgent-elective and emergent cases 8. Policy for allocation and reallocation of block time 9. Sufficient beds for all cases Outcome Deliverables 1. Environmental Scan, OR capacity, actual delivery of surgical services a. UW and UW Medicine b. Locally and regionally (Seattle, WA, WWAMI) c. Nationally 2. Identify best practices for strategic planning in surgical services 3. Document current processes for strategic planning, where they exist a. Document other strategic initiatives that affect the OR in UW Medicine and UWMC 4. Strategic planning process evaluation using LEAN principles 5. Coordinated incentive system for all team members aligned with UWMC principles and best industry practice 6. Proposal for optimized strategic planning process a. Baseline strategic plan (including Marketing) 7. Coordination of PI in surgical services with Center for Clinical Excellence Essential Metrics: Pt. Satisfaction feedback - after a number of surgeries get detailed patient feedback Use of OR space Lower manipulation of day-to-day work Project Support: Lean Expert Resources: 687302980 2/5/2016