Elective Report - Keele University
advertisement
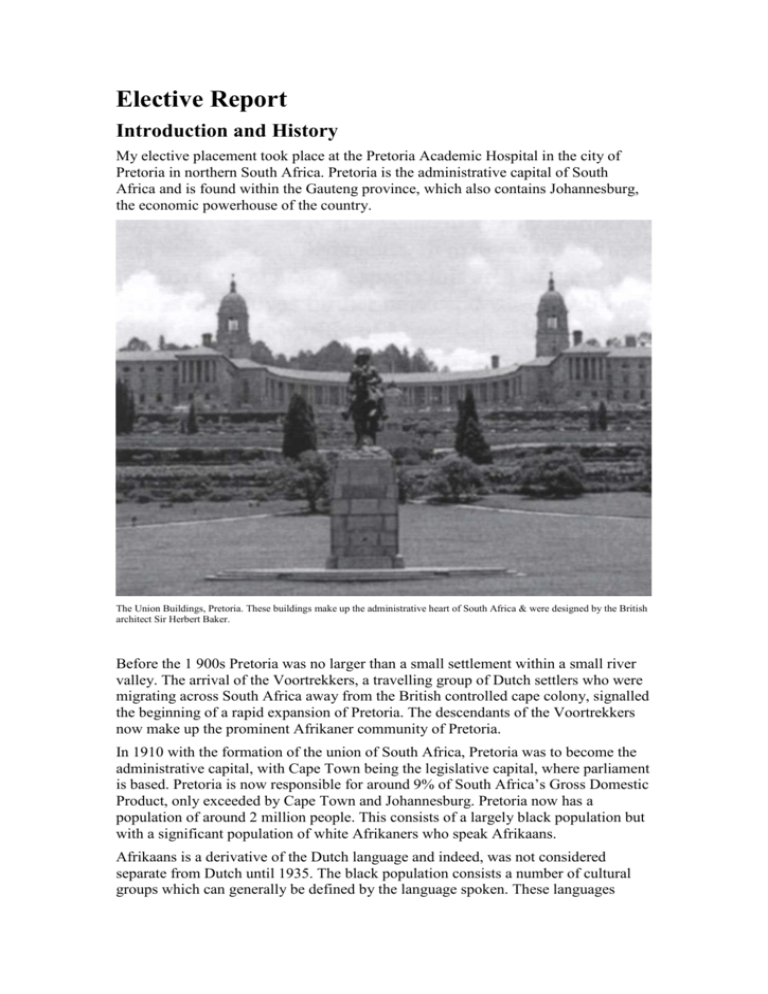
Elective Report Introduction and History My elective placement took place at the Pretoria Academic Hospital in the city of Pretoria in northern South Africa. Pretoria is the administrative capital of South Africa and is found within the Gauteng province, which also contains Johannesburg, the economic powerhouse of the country. The Union Buildings, Pretoria. These buildings make up the administrative heart of South Africa & were designed by the British architect Sir Herbert Baker. Before the 1 900s Pretoria was no larger than a small settlement within a small river valley. The arrival of the Voortrekkers, a travelling group of Dutch settlers who were migrating across South Africa away from the British controlled cape colony, signalled the beginning of a rapid expansion of Pretoria. The descendants of the Voortrekkers now make up the prominent Afrikaner community of Pretoria. In 1910 with the formation of the union of South Africa, Pretoria was to become the administrative capital, with Cape Town being the legislative capital, where parliament is based. Pretoria is now responsible for around 9% of South Africa’s Gross Domestic Product, only exceeded by Cape Town and Johannesburg. Pretoria now has a population of around 2 million people. This consists of a largely black population but with a significant population of white Afrikaners who speak Afrikaans. Afrikaans is a derivative of the Dutch language and indeed, was not considered separate from Dutch until 1935. The black population consists a number of cultural groups which can generally be defined by the language spoken. These languages include Sotho, Tswana and Zulu. Having said this English is widely spoken amongst most groups of the population and is the language most often used in newspapers and television media. The Language used in road signs and other public utilities varies between Afrikaans and English, although there is a general trend of replacing Afrikaans with English, as well as a trend of re-naming streets named after the so-called architects of apartheid to names considered more appropriate for modern South Africa. However, according to my experience this is largely unpopular amongst most South Africans, regardless of race. Most are adamant that they do not want the past to be forgotten. Indeed, there is a very tangible sense of pride about how new South Africa is taking shape, despite the hardships of the past. Many of Pretoria’s streets are lined with Jacaranda trees that blossom mauve in spring, giving rise to the city’s nickname “Jacaranda City”. Pretoria is one of South Africa’s leading academic cities boasting three universities and many thousand students. There is a rather boisterous student community situated towards the east of the city. This area is also home to a large number of restaurants, malls, supermarkets and drinking establishments, in many ways similar to any European city (apart from the prices!). In many respects this area of the city can be seen as the most prosperous, and as one moves further north and west conditions generally deteriorate, especially in the nearby township of Mamelodi. This area still bears the scars of apartheid but is also full of optimism about the future. For example, the Mamelodi Sundown’s soccer team are the reigning champions of the South African soccer league. South Africa has a very turbulent recent history and is still finding its feet since the walls of apartheid fell and Nelson Mandela came to power in 1994. There has been a huge and dramatic cultural shift in a relatively short period of time and in many ways the people of the country are still coming to terms with life in new South Africa. The white minority of the country has played a disproportionately large part in shaping the history of South Africa. This began largely due to the strategic significance of the Cape Sea Route and the colonisation and immigration of the area by many European settlers. The first European settlers were the Dutch (or Boers) who inhabited the Cape of Good Hope in the 1600’s. The Dutch also brought with them many slaves to work in the area, particularly from the Indian subcontinent. The descendants of these slaves now make up a significant proportion of South Africa’s population, particularly along the Wild Coast where curry and bunny chow (a loaf of bread hollowed and filled with curry) are common culinary delights. Following the second Boer war, laws restricting the voting rights of black people were introduced. Despite the abolition of slavery, black people were seen very much as second class citizens and during the following years many more laws were introduced by the white minority that restricted the rights of black people, including where they could live, the jobs they were allowed to do and eventually the use of certain public amenities. This resulted in so-called ‘petty apartheid’ which meant that items such as swimming pools, park benches and telephone boxes were not to be shared by black and white people. Street signage in Pretoria. After many years of difficult struggle, the black population fought against the injustice of apartheid and where eventually victorious. Their struggle was also aided by international pressure and sanctions. Nelson Mandela was released from Prison in 1992 and the country held its first multi-racial election in 1994 with Mandela’s African National Congress gaining power. The laws that set up the pillars of apartheid were then removed from the statute books. In these shadows, South Africans are fighting to get on with their lives. There is a deep sense of pride about the country and indeed the logo “proudly South African” is seen plastered across everything from food to newspapers. The scars of the past are slowly healing and the different cultural groups who were once at loggerheads are now working together to solve the problems now facing the country, such as spiralling crime and the HIV/AIDS epidemic. When I first arrived in South Africa I was struck by the stark contrast between rich and poor. Those living in the central Pretoria, and other cities I visited live in relative prosperity, with standards similar to those found in England. However, one does not have to travel far to find the old townships where people still live in dire squalor. The townships are areas on the outskirts of major cities where black people were removed to and forced to live during the years of apartheid. The standards of living were horrendously poor, and despite recent government initiatives such as free housing, are still appalling compared to the standards of other parts of the city. The fact is that townships are still occupied solely by black people whilst many prosperous city areas are inhabited by the white minority. During my stay in South Africa I came to realise that although the statutory segregation forced upon the black population by the laws of apartheid have gone, there is now an apartheid which is being driven by pure economics. Black people are still relatively poor compared to the white minority, and they are suffering as a consequence. Recent initiatives such as the Black Economic Empowerment laws are fighting to turn these tables by making it easier for black people to get high paid jobs which, under the laws of apartheid they would have been restricted from getting, but this is a slow process and the rebalancing of economic power is still lagging far behind that of political power for the black population. The Health System The health system in South Africa has also had to adjust quickly following the abolition of apartheid. Previously, hospitals were assigned to particular racial groups, with most resources being spent on those providing health care to white people. Primary care was poorly developed. Now hospitals do not discriminate according to race and the emphasis of the system is shifting from hospital-based care to primary care in the community. This shift is also being mirrored currently in the United Kingdom. Since 1994, more than 700 community clinics have been built or upgraded. Free health care for children under six, and for pregnant or breastfeeding mothers, is becoming increasingly available. However, the challenges in primary health clinics are still enormous. Many clinics still lack basic equipment, drugs, HIV tests and essentials like piped water, telephone access and reliable electricity supplies. The state health care system struggles to deliver health care to 80% of the population, whilst 20% choose private care. The strain on the health care system is amplified by the fact that around 40% of South Africa’s population is unemployed and around 50% are classified as living in poverty. Diseases such HIV/AIDS and poverty-related diseases such as cholera and tuberculosis, as well as malnutrition are the major challenges facing the health care system. In recent years very large sums of money have been spent on raising the awareness of the population of HI V/AIDS and on providing free anti-retroviral drugs to sufferers. My experience has shown me that within the public sector itself there are gross inequalities between tertiary centres (which are often the old ‘white’ hospitals) and secondary centres. Tertiary centres have a very high standard of cleanliness and equipment, including ultrasound CT and MRI scans, and laboratory tests are freely available. The secondary service however, which deals the majority of patients, operates with much harsher constraints and even simple equipment such as needles and syringes can sometimes be hard to come by. The state system is chronically under-funded and spending on drugs per patient, for example, is much less than in the private sector. As well as a shortage of funding, there is also a shortage of doctors, particularly in rural areas. To combat this, the government has made it easier for foreign doctors to practice in South Africa and has made it compulsory for medical school graduates to complete two years of community service in understaffed hospitals and clinics. My Placement My elective placement was in the Pretoria Academic Hospital. The hospital is a purely tertiary healthcare institution, rendering specialized and highly specialized services to medically referred patients. However, the hospital also contains an Accident and Emergency department which receives acute emergencies from the nearby area. The hospital has 832 approved beds, 76 ICU beds, 46 High Care beds, 108 beds in the Oncology Complex, 22 theatres, 19 Lifts and 80 Consulting rooms in the outpatient department. During the elective period I spent four weeks in the neurology department and four weeks in the internal (general) medicine department. During each of these placements I joined the firm of one of the consultants or professors, which also contained approximately three South African sixth year medical students as well as an intern and a number of registrars. My accommodation was within the commune of a doctor from the hospital. I shared with three German medical students and one Dutch student. I made very good friends with these students and also learnt a lot about the culture in Germany and Holland, as well as how medical education differs. Outside of working hours we also spent time together exploring South Africa from head-to-toe, with our only other companions being the Lonely Planet and a 1984 Volkswagen Jetta. The system of medical education at Pretoria University is slightly different to that of my home University. Sixth year students on each firm split the patients between them and are expected to attend the ward each morning and visit their patients, write follow-up notes and find blood/investigation results from the previous day. The registrar then does a daily ward round. If any further investigations are ordered, it is the responsibility of the student to see that these actually took place and that the results are delivered to the patients file in a timely fashion. Being responsible for your own patients is something which I had never fully experienced in the United Kingdom before. I found it very rewarding and also very captivating as I became truly involved in the care the patient received. I also began to feel a sense of companionship with the patients, many of whom I saw every morning for a number of weeks. Students are also expected to be on-call once per week and each alternate weekend. The students on-call are expected to clerk new patients, formulate a differential or working diagnosis and order preliminary investigations before presenting the patient on the post intake ward round the following day. These sessions can be extremely hard work, particularly if the patient load is heavy. Having said this, these sessions were also very rewarding. As a student I was given a large amount of responsibility and being the first person to see the patient and formulate a working diagnosis was a very worthwhile and educational experience, even if I was too tired to present properly the following morning! Consultant ward rounds took place weekly and after each on-call session. These ward round were very lengthy as each patient (sometimes as many as 30) was discussed in detail. The emphasis was on education of the students and junior doctors and I learnt a great deal from these sessions. Additionally, there were also consultant led teaching sessions (called ‘tats’ by local students) which took place daily, usually in class-room situations. Apart from these commitments there were also weekly out-patient clinics which students were expected to attend and clerk patients and present to the consultant. I formulated a number of learning objectives before and during my elective placement: Integrate with South African Sixth Year Students and Participate with On-call Rota As mentioned earlier I joined the South African final year students on neurology and internal medicine firms and participated with the on-call rota. As mentioned earlier, the on-call work was one of the most satisfying and rewarding experiences of my elective. Of all the patients I clerked and were subsequently admitted, I remember one in particular. Sheila (name has been changed) was 29 years old and presented with a reduced level of consciousness, confusion and a swollen leg. She received initial resuscitation and was ventilated for a time in the high care unit. She subsequently developed ventilator associated pneumonia, for which she was treated. She was then admitted to the general medical ward and the opinion of a vascular surgeon was sought. After investigation it was decided that her left leg would have to amputated below the knee, which had become necrotic due to arterial occlusions. HIV had been ruled out and the working diagnosis was a thrombophilia of unknown aetiology, however, all screening tests subsequently came back negative. During my time on the ward I got to know Sheila quite well and was very happy for her when it was decided that she would be discharged, even though the medical team had no explanation for her sudden vascular event. I was therefore dismayed when during my on-call session the following night she was transported to the hospital by ambulance due to her being found asleep in a supermarket after drinking rather too much alcohol! Practice presentation of patients on ward rounds Medical students in South Africa are very integrated with the clinical firm and actively participate in patient care. I was given many opportunities to present patients on ward rounds in front on consultants and professors and I relished this. This experience boosted my confidence and I now feel more able to present and make valued contributions to ward rounds and ultimately contribute to the overall care of the patient. Practice and improve competency of neurological examination There was plenty of opportunity for me to practice my examination skills under the supervision of registrars and consultants. It was interesting to see different techniques used for eliciting certain signs such as the babinski reflex. At the end of my placement I also sat the neurology practical examination with the South African students and received excellent feedback on my performance. My experience in South Africa has reinforced to me how examination of the patient is an art which must be practiced thoroughly. One must employ years of experience to elicit certain subtle clinical signs. Being taught and being able to practice clinical examination of the neurological system by the professor of neurology at Pretoria was a particular highlight for me, and it was very enjoyable to watch a master at work. My learning with regards to the examination of patients was reinforced by presenting my patients on the academic ward round each week and being grilled about what I deduced from my findings! Explore and gain an understanding of common neurological conditions in South Africa This experience was gained from ward rounds and teaching sessions, as well as personal reading in the hospital library. The most common conditions I witnessed during my stay were HIV/AIDS related neurological conditions. These included cerebrovascular accidents (which are much commoner in patients with HIV) and meningitis, often with organisms rarely seen in the United Kingdom, such as Cryptococcus. I also noted that the average neurological patient in South Africa is much younger than the average neurological patient in the United Kingdom, where chronic conditions of the elderly such as Parkinson’s disease appeared more prevalent during my medical education. I initially found working in an environment with such a high HIV prevalence daunting and was rather worried that I would be putting myself at risk. However, I soon discovered that appropriate safeguards were in place and that gloves were readily available. Working in this type of environment is normal for South African medical students and I found that it was possible to take appropriate safety measures without interfering with efficient patient care. Practice Lumbar Puncture In the United Kingdom I have had little opportunity to perform a lumbar puncture. For this reason I decided that a good goal for my elective would be to perform a number of lumbar punctures. I mentioned this fact to my registrar on arrival and gave him my mobile telephone number. My registrar then rung me on a number of occasions, firstly to simply observe him conducting a lumbar puncture and then to perform them for myself. I now feel competent in performing lumbar puncture independently and am aware of the indications and contraindications of the procedure. I am also more able to interpret the results of cerebrospinal fluid analysis. As well as lumbar puncture, I also practiced a number of other procedures which will be useful for me as a medical student and future doctor. These included phlebotomy and venous cannulation, catheterisation, ophthalmoscopy & arterial blood gas sampling. Experience working in an environment with strict economic constraints Although my neurology placement was within a tertiary public hospital, I was still aware of economic constraints, particularly in the choice of drugs. One of the main reasons I am fond of the National Health Service in the United Kingdom is the fact that, in general, the same treatments are available to everyone, regardless of their economic status. I feel uneasy in situations where poorer people receive an inferior standard of care simply because they have less money. Having said this, one has to work within the constraints of the system and do the best you can to help people within these barriers. I am glad that I put myself in this situation because, after all, this is how health care is organised in the vast majority of countries. Understand the importance of HIV/AIDS in neurological disease As mentioned earlier, HI V/AIDS is one of the most common disease found in South African hospitals and indeed many wards are filled with patients who are suffering from complications of the disease. Neurological complications of HIV which I witnessed whilst on my elective included HIV-related dementia, cryptococcal meningitis and primary CNS lymphomas. For a number of patients the first presentation of HIV was to the neurology department with a meningoencephalitis. Patients given a new diagnosis of HIV were counselled by the medical team and professional counsellors. As a student I was expected to counsel patients regarding HIV blood testing and the implications of a positive and negative result. I conducted this on a number of occasions and performed a number of HIV tests. Conclusion My elective was an extremely enjoyable and educational experience. I feel that I have learnt a lot about medicine, but also a lot about myself. I have experienced not only a different health care system but also a different culture and way of life. I feel this has broadened my horizons and made me more knowledgeable about the world. As a doctor I will meet people from all over the world, and my experiences on my elective have wet my appetite for this opportunity.