Discussion paper - University of Sheffield
advertisement

1
A TWO LEVEL MONTE CARLO APPROACH TO CALCULATING EXPECTED VALUE OF
2
SAMPLE INFORMATION:- HOW TO VALUE A RESEARCH DESIGN.
3
4
Alan Brennan, MSc(a)
5
Jim Chilcott, MSc(a)
6
Samer Kharroubi, PhD(b)
7
Anthony O’Hagan, PhD(b)
8
Johanna Cowan (a)
9
10
(a) School of Health and Related Research, The University of Sheffield, Regent Court, Sheffield S1
11
4DA, England.
12
(b) Department of Probability and Statistics, The University of Sheffield, Hounsfield Road, Sheffield
13
S3 7RH, England.
14
15
Reprint requests to: a.brennan@sheffield.ac.uk
16
17
18
Acknowledgements:
19
20
The authors are members of CHEBS: The Centre for Bayesian Statistics in Health Economics.
21
Particular thanks to Karl Claxton and Tony Ades who helped finalise our thinking at a CHEBS “focus
22
fortnight” event in April 2002. Also to Gordon Hazen, Doug Coyle, Myriam Hunink and others who
23
stimulated AB further at the viewing of the poster at the MDM conference 2002 Finally, thanks to the
24
UK National Coordinating Centre for Health Technology Assessment which originally commissioned
25
two of the authors to review the role of modelling methods in the prioritisation of clinical trials (Grant:
26
96/50/02) and have started us on this path.
27
28
1
29
ABSTRACT (original MDM conference abstract – rewrite)
30
31
32
Purpose: describe a generalised two level Monte Carlo simulation for calculating partial EVSI.
33
34
Background: Claxton has promoted the EVSI concept as a measure of the societal value of research
35
designs to help identify optimal sample sizes for primary data collection. A method applies (using unit
36
normal loss integral formula to calculate EVSI for sample size n), if the net benefit function is normally
37
distributed, and if the proposed sample exercise measures all the model parameters. Whilst common in
38
trials, such conditions are not universal and a generalised method is needed for, so called, partial EVSI.
39
40
Methods: A two level algorithm, originally developed for partial EVPI applications, has been further
41
refined, tested and applied to undertake EVSI calculations. The paper also sets out a mathematical
42
notation for EVSI for parameter(s). The algorithm begins by sampling a 1st value for the parameter of
43
interest (e.g. the underlying true %response rate to a drug, 1) and then… [sampling data (e.g. the
44
response rate found in a trial of n=100, given 1). A Bayesian update for the parameter of interest is
45
calculated (merging the prior probability distribution with the sampled data). This has a revised mean
46
and a smaller variance than the ‘prior’ because new information has been obtained. 1000 monte carlo
47
samples are now generated, allowing the parameter of interest to vary over its Bayesian updated
48
distribution, and all other parameters to vary according to their priors. The expected net benefit of each
49
strategy is examined and the best strategy chosen.] The process in [ ] is repeated for a 2nd monte carlo
50
sample of the parameter of interest, then a 3rd and … 1000 times. The overall mean expected net
51
benefit is compared to the expected net benefit without further data collection - the difference is the
52
EVSI for the research. An illustrative model for two treatments, costs and benefits is used to show
53
EVSI for a trial, a QALY study, both together, a long term follow up, and an all parameter study.
54
55
Results: A mathematical expression for partial EVSI is generated, clearly showing the 2 level monte
56
carlo in terms of 2 “expectations”. Given sample data, Bayesian updating requires an analytic
57
expression to revise parameters of the distribution (given here for normal, beta, gamma and lognormal
58
distributions. More general distributions may require other approximations or MCMC methods.
59
The algorithm applies equally for sets of parameters as for a single one.
60
61
Conclusion: This provides a significant step towards a generalised method for partial EVSI
62
2
63
A TWO LEVEL MONTE CARLO APPROACH TO CALCULATING EXPECTED VALUE OF
64
SAMPLE INFORMATION:- HOW TO VALUE A RESEARCH DESIGN.
65
66
Introduction
67
68
Clinical trials and other health research studies are investments, which hopefully lead to reduced
69
uncertainty about the performance of health technologies and improved decision making on their use in
70
practice. What is the added value of a proposed research study? How much more valuable would it be
71
if its sample size were increased, or its design altered to measure additional data items or to collect
72
information over a longer time? Would a different research question be more appropriate and valuable
73
to decision makers than the proposed study? These questions are important for governmental,
74
academic and indeed commercial healthcare research funding bodies throughout the world. The aim is
75
to allow researchers and funding agencies to rank different options for data collection, including
76
different sample sizes, additional data on resource use and costs, the added benefit of quality of life /
77
utility studies, longer trial durations or alternative study design such as observational or
78
epidemiological studies rather than randomised controlled trials.
79
80
Traditionally, the large investments in, for example, phase III clinical drug trials, have been planned
81
around proving a statistically significant clinical difference i.e. delta (δ). The implied assumption is
82
that, if a clinical delta is shown conclusively, then adoption of the new technology will automatically
83
follow, i.e. in a sense the clinical delta is a proxy for economic viability of the technology. This
84
produces a relatively common problem in cost-effectiveness analysis, where a study may show a
85
clinically important outcome, but not be powered sufficiently to provide enough information for a
86
reasonable estimation of cost-effectiveness. This leaves healthcare decision makers with uncertainty
87
concerning adoption decisions and sometimes with the need to acquire further information before a
88
final decision is made.
89
90
Recent work on valuing research has followed either the value of information direction (as this paper
91
does) or the so-called payback approach (Eddy 1989, Townsend and Buxton 1997, Davies et al 1999,
92
Detsky 1990, Drummond et al 1992, Buxton et al 1994). The payback approach compares the costs
93
and benefits of undertaking a specified technology assessment versus no data collection. Firstly, the
94
analyst lists the possible results of the proposed technology assessment (so-called ‘delta results’), then
95
quantifies the likely changes in practice, health benefits and cost consequences for each delta result,
96
and finally, by estimating the probability of each possible delta result, produces a weighted average
97
(i.e. expected) cost and health benefits for the study. By comparing this with the anticipated cost and
98
health benefit consequences of no data collection, the incremental cost-effectiveness of undertaking the
99
proposed study can be calculated. There are two main shortcomings of this method: firstly, the
100
starting point of the cost-benefit analysis is evaluation of a single specified research proposal, which
101
implicitly assumes that the suggested proposal is optimally designed. In fact, the optimal trial design
102
can only be shown be comparing a range of possible designs. Secondly, in practice the likelihood of the
3
103
different results of the trial (at its simplest positive or negative) has very often been arbitrarily decided,
104
giving rise to a lack of robustness in the payback model’s calculations.
105
106
The expected value of sample information approach has been suggested as a tool to quantify the
107
societal value of research and to identify optimal designs and sample sizes for primary research data
108
collection (Claxton and Posnett 1996, Claxton et al 2001). EVSI differs from the payback approach in
109
that it begins immediately with a cost-effectiveness model of the interventions of interest including an
110
assessment of the existing uncertainty. The decision to adopt a particular intervention policy is made
111
on the basis of the cost-effectiveness decision rule: choose the option with the greatest expected health
112
benefits after adjusting for cost differences between strategies (i.e. the largest expected net benefit).
113
Where there is large uncertainty, the adoption decision based on current information could turn out to
114
be sub-optimal, and so obtaining more data on uncertain parameters reduces uncertainty and adds value
115
by reducing the chance of making a sub-optimal adoption decision. Because collecting data also incurs
116
costs, a trade-off exists between the expected value of the additional data and the cost of obtaining it.
117
In this framework, the research design problem involves two components: what data to collect (i.e.
118
upon which uncertain model parameters should data be collected) and how much data to collect
119
(sample size)?
120
121
To date most methodological development has focussed on the expected value of perfect information
122
(ref Brennan MDM or CHBS discussion paper, Karl, Coyle) i.e. the expected value of perfect
123
knowledge on all parameters in the model (overall EVPI) or perfect knowledge on subgroups of
124
parameters (partial EVPI). Earlier work (Claxton and Posnett 1996, Claxton et al 2001) on EVSI
125
focussed upon relatively simple proposed data collection exercises (i.e. collect data on every uncertain
126
model parameter in one single data collection exercise with a single specified sample size) and was
127
valid in a relatively small number contexts (technically, the uncertainty in the net benefit function must
128
be a normally distributed function for the so-called ‘unit normal loss integral’ formula to be valid).
129
Given that most cost-effectiveness models of interventions and most proposed research studies focus
130
on more complex situations than this, a generalised method for calculating partial EVSI is required.
131
132
This paper describes a generalised method to quantify the value of alternative proposed research
133
designs. The approach uses Bayesian methods and two level Monte Carlo sampling and simulation, to
134
produce the expected value of sample information for uncertain parameters in the cost-effectiveness
135
model. A detailed algorithm for undertaking the EVSI calculation process is developed and the
136
mathematical formulation for the calculations is presented. An important component is the synthesis of
137
the existing uncertainty for a parameter with the simulated data collection, which requires a process
138
called Bayesian updating. The Bayesian updating procedure is described for the normal, beta, gamma
139
and lognormal distributions and methods for other distributions are discussed. To test its feasibility
140
and to explore the interpretation of the results, the methodology is applied to an illustrative cost-
141
effectiveness model comparing two interventions. EVSI results can be calculated for each different
4
142
sample size but this paper also examines an interpolation method so that EVSI for smaller or larger
143
sample sizes can be estimated to reduce the need for larger numbers of simulations.
144
145
1035 words - Intro
146
147
Method
148
149
The two level EVSI algorithm
150
151
The general algorithm to calculate EVSI involves setting up decision model for the possible
152
interventions, characterising uncertainty with probability distributions, simulating a variety of results
153
for a proposed collection of further data, synthesising the existing (prior) evidence with the simulated
154
collected data, and finally evaluating the impact of the data collected on the decision between the
155
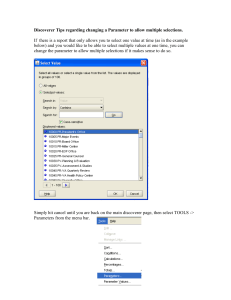
interventions. Box 1 describes the detailed structure of the algorithm.
156
Box 1: General Algorithm to Calculate EVSI
0. Set up a decision model –to compare the costs and health benefits of different interventions,
including adoption decision rule, e.g. “select strategy if marginal cost per QALY is < $50,000”,
enabling net benefits (i.e. $50,000 * QALYs – Cost) to be calculated.
1. Characterize uncertainty – for each model parameter (i) identify appropriate probability
distributions to characterise existing evidence and uncertainty e.g. % response rate to drug is beta
(a, b)
2. Work out the ‘baseline decision’ given current evidence – use the probabilistic sensitivity analysis
approach to simulate, say 10,000 sample sets of, uncertain parameter values by Monte Carlo
sampling. Use the decision model to identify the intervention that provides highest net benefit on
average over the simulations.
3. Define a proposed data collection - decide on a proposed sample size for collecting data on each
of the parameters of interest (e.g. a trial of n=100 to collect data on the % response rate to a drug).
4.
Begin a loop to simulate the possible variety of results from the proposed data collection. –
There are two sources of variety in the possible results. The first is the uncertainty about the true
underlying value of the parameter of interest. The second is that, even given the true underlying
value of the parameter of interest, there is random chance associated with data collection of a
specific finite sample size. Both need to be accounted for in the simulation.
Sample the data collection:
a) sample the true underlying value for parameter of interest (i) from its prior uncertainty
5
(e.g. use Monte Carlo to sample the true underlying value for the % response rate to a drug
from the probability distribution identified in step 1, say sample 1 for i= 60%)
b) sample simulated data (Xi) given the sampled true underlying value of parameter of interest
(e.g. sample the mean value for the response rate found in a trial of n=100, given i= 60%).
5.
Synthesise existing evidence with simulated data - for each parameter, combine the prior
knowledge with the simulated data collection using Bayesian updating techniques. The result is a
simulated posterior probability distribution for true value of the parameter of interest. Typically,
the posterior has a revised mean and a smaller variance than the prior probability distribution.
6.
Examine the impact of the simulated data collection on the decision between interventions Re-run the probabilistic sensitivity analysis on the decision model. Allow parameters of interest
to be sampled from their posterior probability distributions (step 4) and remaining parameters
(those with no additional collected data) to be sampled from prior probability distributions (step
1). Identify the ‘revised decision’ - the intervention that provides the highest net benefit on
average over the simulations, and compare this to the ‘baseline decision’.
7.
Quantify the added value of the simulated data collection – if the ‘revised decision’ is different to
the ‘baseline decision’ then the simulated data collection has added value.
the expected net benefit of the ‘revised decision’ (step 6)
The value of simulated data =
.
minus the expected net benefit of the ‘baseline decision’ (step 2).
Record the ‘revised decision’ and its average net benefit. Then, loop back to repeat steps 4 to 7,
say 1,000 times, in order to simulate the variety of results from the proposed data collection.
8.
Quantify the Expected Value of the Sample Information (EVSI) for the proposed data collection
–After all of the loops to simulate the variety of possible results from the proposed data
collection, the EVSI is simply the average of the results obtained in step 7.
Hence,
EVSI for proposed data collection =
average net benefit provided by the ‘revised decisions’
.
average net benefit provided by the ‘baseline decision’.
minus
157
158
159
6
160
Mathematical formulation
161
162
The general algorithm is reflected in the detailed mathematical formulation for the EVSI calculations
163
as described below.
164
165
Let,
166
be the set of uncertain parameters for the model, with defined prior probability distributions
167
d
be the set of possible decisions i.e. interventions
168
NB(d,) be the net benefit function for decision d, which also depends on the parameters
169
E[f(x)] denote the expected value of a function f(x)
170
i
be the parameters of interest for possible data collection
171
-i
be other parameters, for which there will be no further data collection. Note {} ≡ {i} U {-
172
i}
173
p(i)
be the prior probability distribution for the true underlying value of i
174
p(-i)
be the prior probability distribution for the true underlying value of -i
175
Xi
be the (simulated) data collected on i
176
p(i|Xi) be the posterior probability distribution for the value of i having obtained the data Xi
177
178
First, consider the situation where we have only the current existing evidence (prior information).
179
Given current information we will evaluate the expected net benefit of each decision strategy in turn
180
and then choose the baseline decision that gives the highest expected net benefit.
181
182
Expected net benefit of ‘baseline decision’ = max E NB(d, )
(1)
d
183
184
Next, consider a proposal to collect further information on the subset of parameters of interest, i. Any
185
data collected would be used to update our understanding about the true underlying value of i, giving a
186
new probability distribution with a revised posterior mean and typically a smaller standard deviation.
187
Given a particular simulated dataset Xi, the ‘revised decision’ can be made by evaluating each
188
decision strategy in turn and then choosing the one with the highest expected net benefit i.e.
189
max E NBd , | X i .
d
190
191
The variety of possible results of the data collection means this expression needs to be evaluated across
192
all possible results for the data collection exercise. That is, the overall expected net benefit following
193
the proposed data collection is given by:
194
195
Expected net benefit of ‘revised decision’ |proposed data: = E X i max E NBd , | X i
d
(2)
196
7
197
This expression clearly shows the two levels of expectation involved. The outer expectation relates to
198
the variety of possible results of the proposed data collection exercise (i.e. the loop which begins at step
199
4 in the algorithm). The inner expectation relates to the evaluation of the decision model under
200
remaining uncertainty having obtained the proposed data (i.e. step 6 in the algorithm where the ‘revised
201
decision’ is evaluated using the probabilistic sensitivity analysis approach allowing the parameters of
202
interest to be sampled from their posterior probability distributions p(i|Xi) and the remaining
203
parameters (those with no additional collected data) to be sampled from their prior probability
204
distributions p(-i)).
205
206
Finally then, the expected value of sample information (EVSI) for the proposed data collection exercise
207
is given by the expected net benefit of the ‘revised decision’ given the proposed data collection (2)
208
minus the expected net benefit of the ‘baseline decision’ (1).
209
EVSI E Xi max E NBd , | X i max E NB(d, )
d
(3)
d
210
211
8
212
Bayesian Updating - synthesising the existing evidence with the simulated data
213
214
Technically, the most demanding part of undertaking EVSI calculations is synthesising the existing
215
prior evidence with the simulated data to form a simulated posterior probability distribution for the
216
parameter of interest. The generalised mathematical equation is given by Bayes theorem (reference
217
useful books from Tony’s preliminary reading list on Bayes). The complexity of the synthesis required
218
depends upon the form of the probability distributions for both the parameter concerned and the related
219
data. For a limited set of distributions, the synthesis of existing evidence and simulated data can be
220
done using a simple formula. These so-called conjugate distributions are such that the functional form
221
of the probability distribution does not change as new data is added. Examples (detailed below),
222
include the normal, beta (binomial), gamma (poisson) and lognormal distributions. Other conjugate
223
distributions include ….. (Tony / Samer complete). For more complex or non-conjugate distributions,
224
simple analytic formulae for Bayesian updating are not possible and the only approach is to use
225
estimation methods. The most commonly used estimation method uses the mathematics of Markov
226
Chain Monte Carlo (reference Spiegelhalter / MCMC papers) to estimate a posterior probability
227
distribution. Typically, this involves a potentially time consuming MCMC simulation (at step 5 in the
228
algorithm) using freely available software such as WinBUGS (refs and website).
229
230
Bayesian updating: Normal distribution
231
232
The normal distribution can represent uncertain cost-effectiveness model parameters, which are
233
continuous variables distributed symmetrically around a mean value (no skewness), and which might
234
include both positive and negative values. The exact shape of the probability distribution is determined
235
by the two normal distribution parameters, the mean μ and standard deviation σ. The normal
236
distribution is particularly useful when representing the uncertainty in an average. An example of a
237
cost-effectiveness model parameter that might take a normal distribution could be the mean utility
238
change for patients who respond to a drug treatment. Typically, the value of such a cost-effectiveness
239
model parameter might be estimated from a clinical trial or observational study of individual patients’
240
utilities before and after treatment. This individual patient level data (or the mean and 95% confidence
241
interval from a published report of the study) would be used to estimate the prior mean μ0 and prior
242
standard deviation σ0 for the cost-effectiveness model parameter, given current evidence.
243
244
Box 2 part A provides the mathematics for the process of Bayesian updating for normal distributions
245
and three worked examples using illustrative data on a model parameter: utility gain for drug
246
responders. The process begins with the prior mean μ 0 and standard deviation σ0 assigned from
247
existing evidence, where necessary incorporating expert opinion. For the normal distribution updating
248
formula a third parameter is needed, that is the population level standard deviation σ pop, which
249
represents patient level uncertainty. (E.g. the individual patient level uncertainty in the utility gain for
250
drug responders σpop may be 0.2 but the uncertainty in the mean σ0 may be 0.1, lower because the
251
uncertainties of many patients will average out to give less uncertainty in the mean). The next step is
9
252
to simulate a data collection exercise of the chosen sample size. For some other distributions it is
253
necessary to simulate sample data at the individual patient level, but for the normal distribution the
254
process can be shortcut by simulating the sample mean. First, sample a true underlying value for the
255
cost-effectiveness model parameter μ0sample from the prior probability distribution Normal(μ 0, σ02).
256
Second, simulate the mean of the data collected X given this sampled true underlying value μ 0sample
257
from the probability distribution Normal(μ 0sample, σ2pop/n). Thus, we account firstly, for the uncertainty
258
in the true value of the parameter, and secondly, for the random variation in data collection due to the
259
sample size n, which has greater effect for a smaller chosen sample size n. The final step is to
260
synthesise the simulated data with the prior information using the formulae in (j) and (k).
261
262
The worked examples show that as new simulated data is obtained, the estimated mean of the
263
parameter is adjusted and the standard deviation (uncertainty in the mean of the parameter) is reduced.
264
Figure 1 illustrates the results for 3 separate simulated data samples, showing the impact on the mean
265
and variance of the model parameter. We observe that the posterior mean can take values across the
266
full range of the prior probability distribution. The posterior variance is the exactly same for all 3
267
simulated data sets and examining the formula shows that the posterior variance is independent of the
268
simulated data X but depends only on the size of the sample n. The formula also shows that shows
269
the posterior variance is always lower than the prior variance. Finally, there is a clear relationship
270
between the proposed sample size n and the posterior variance. If the sample size is very small, the
271
posterior variance approaches the prior variance i.e. we have little additional certainty. As the sample
272
size approaches infinity, the posterior variance approaches zero and we are nearing ‘perfect
273
information’.
274
275
Insert Figure 1.
276
10
277
Figure 1. Bayesian Updating
278
Part A Normal distribution: Posterior distributions after sampling 50 cases
Frequency (10,000 samples)
1600
1400
Prior
1200
Posterior after
Sample 1
1000
800
600
Posterior after
Sample 2
400
Posterior after
Sample 3
200
0
0
900
800
700
600
500
400
300
200
100
0
0%
Prior
Posterior after
Sample 1
Posterior after
Sample 2
Posterior after
Sample 3
20%
40%
60%
80%
% response rate for drug
100%
Part C Gamma distribution: Posterior distributions after sampling 50 cases
Frequency (10,000 samples)
281
282
1
Part B Beta distribution: Posterior distributions after sampling 50 cases
Frequency (10,000 samples)
279
280
0.5
Utility gain for drug responder
2000
Prior
1500
Posterior from
Sample 1
1000
Posterior from
Sample 2
500
Posterior from
Sample 3
0
0%
50%
100%
Mean Side Effect Rate
283
284
285
11
286
Bayesian updating: Beta (Binomial) distribution
287
288
The beta distribution can represent uncertain cost-effectiveness model parameters, which are
289
proportions, probabilities or percentages. The beta distribution is fundamentally linked to data for
290
which the answer is either “yes” or “no”, i.e. binomial data often expressed with only the values 0 and
291
1 (). The exact shape of the probability distribution is determined by the two beta distribution
292
parameters, a and b. An example of a cost-effectiveness model parameter that might take a beta
293
distribution could be the percentage of patients who respond successfully to a drug. At an individual
294
level, each patient has only two possible results, “response” or “no response”. Again, existing evidence
295
from clinical trial or observational study data should be used to quantify the prior distribution e.g.
296
percentage responders will be a distribution Beta(a0,b0) where a0 is the number of patients who
297
responded, b0 is the number of patients who did not respond, and the prior mean for the response rate is
298
a0/(a0 + b0).
299
300
Box 2 part B provides the mathematics for the process of Bayesian updating for beta distributions and
301
three worked examples using illustrative data on another model parameter: drug response rate. The
302
process begins with the quantifying the prior parameters a0 and b0. The next step is to simulate a data
303
collection exercise of the chosen sample size. First, sample a true underlying value for the response
304
rate parameter resp_rate0sample from the prior probability distribution Beta(a0,b0). Second, simulate the
305
number of responders y, which might arise from the proposed sample size n given this sampled true
306
underlying value resp_rate0sample from the probability distribution Binomial (n, resp_rate 0sample). Again,
307
we account firstly, for the uncertainty in the true value of the parameter, and secondly, for the random
308
variation in data collection due to the sample size n, which has greater effect for a smaller chosen
309
sample size n. The final step is to synthesise the simulated data with the prior information to give the
310
posterior distribution using the very simple formula posterior is Beta(a 0+y, b0+n-y).
311
312
The worked examples show that as new simulated data is obtained, the estimated mean of the
313
parameter is adjusted and the standard deviation (uncertainty in the mean of the parameter) is reduced.
314
Figure 1 part B illustrates the results for 3 separate simulated data samples, showing the impact on the
315
mean and variance of the model parameter. We observe that the Beta distribution based on small
316
sample sizes (as in the prior) is skewed but as larger samples are obtained it appears (and can be
317
approximated by) normal. As with the updated normal distribution, the posterior mean can take values
318
across the full range of the prior probability distribution. The posterior variance is not exactly the same
319
for all 3 simulated data sets because mathematically it depends on the sampled data, and in these
320
examples the closer that sample is to a response rate of 100%, the smaller the posterior variance.
321
Finally, again there is a relationship between the proposed sample size n and the posterior variance. If
322
the sample size is very small, the posterior variance approaches the prior variance i.e. we have little
323
additional certainty. As the sample size approaches infinity, the posterior variance approaches zero and
324
again we are nearing ‘perfect information’.
325
12
326
Bayesian updating: Gamma (Poisson) distribution
327
328
The Poisson distribution is often used to model the number of events happening during a specified unit
329
of time, working under the assumption that event occurrence is random but with a constant mean event
330
rate λ. The gamma distribution is related and can be used to express the uncertainty in the mean event
331
rate λ. The exact shape of the probability distribution is determined by the two gamma distribution
332
parameters, a and b and thus λ ~ Gamma (a,b). An example of a cost-effectiveness model parameter
333
that might take a gamma distribution could be the mean number of side effects experienced by patients
334
in a year. At an individual level, each patient will experience a discrete number of side effects. The
335
mean number of side effects cannot be negative, and the distribution may be skewed as most patients
336
will experience some side effects but a few may experience many. Again, existing evidence from
337
clinical trial or observational study data should be used to quantify the prior distribution for the average
338
rate e.g. mean number of side effects experienced by patients in a year will be a distribution
339
Gamma(a0,b0) where a0 is prior side-effect rate multiplied by the prior sample size reported from
340
existing evidence, and b0 is 1divided by the prior sample size. The resulting prior mean is a 0*b0 and
341
the prior variance is a0*b02.
342
343
Box 2 part C provides the mathematics for the process of Bayesian updating for gamma distributions
344
and three worked examples using illustrative data on a model parameter: mean side-effect rate for drug.
345
The process begins with the quantifying the prior parameters a 0 and b0. The next step is to simulate a
346
data collection exercise of the chosen sample size. First, sample a true underlying value for the side-
347
effect rate parameter sideeffect_rate0sample from the prior probability distribution Gamma(a 0,b0).
348
Second, given this sampled true underlying value, simulate the number of side effects (y1, y2, … yn) for
349
each of the n patients in the proposed sample from the probability distribution
350
Poisson(sideeffect_rate0sample). This is slightly different from the normal and beta distributions because
351
it is necessary to sample individual-level data. Again, we account firstly, for the uncertainty in the true
352
value of the parameter, and secondly, for the random variation in data collection due to the sample size
353
n, which has greater effect for a smaller chosen sample size n. The final step is to synthesise the
354
simulated data with the prior information, using the simple formulae in Box 2 row9 and row10, to give
355
the posterior distribution for mean number of side effects per person:
356
357
The worked examples show that as new simulated data is obtained, the estimated mean of the
358
parameter is adjusted and the standard deviation (uncertainty in the mean of the parameter) is reduced.
359
Figure 1 part C illustrates the results for 3 separate simulated data samples, showing the impact on the
360
mean and variance of the model parameter. We observe that the Gamma distribution based on small
361
sample sizes (as in the prior) is skewed but (check) as larger samples are obtained it appears (and can
362
be approximated by) normal. As with the updated normal distribution, the posterior mean can take
363
values across the full range of the prior probability distribution. The posterior variance is not exactly
364
the same for all 3 simulated data sets because mathematically it depends on the sampled data. Finally,
365
again if the sample size is very small, then the posterior variance approaches the prior variance i.e. we
13
366
have little additional certainty, whilst if the sample size approaches infinity, the posterior variance
367
approaches zero and we are nearing ‘perfect information’.
368
369
Bayesian updating for other distributions
370
371
Some other distributions are of related functional forms to the normal, beta and gamma and can use
372
adjustments to the analytic formulae presented in Box 2 for Bayesian updating. The lognormal
373
distribution (where log(X) ~ N(, )) is a useful skewed distribution allowing only positive values and
374
can often be used for cost parameters. To update a lognormal parameter, it is necessary to convert into
375
a normal distribution (by raising e to the power of the variable), form the Bayesian posterior for the
376
normal distribution as shown above, and then convert the normal posterior back into a lognormal
377
distribution. Similarly, the exponential distribution, is a special case of the gamma distribution (a=1)
378
and can use the same updating formula.
379
380
Other distributions do not have conjugate properties and cannot use simple formulae for Bayesian
381
updating. Examples include the Erlang, Gumbel and Weibull distributions. If there is no simple
382
conjugate based formula for updating the current standard approach is to use simulation approaches to
383
generate an estimate of the posterior distribution. These simulation approaches are based on
384
mathematics called Markov Chain Monte Carlo (references). Freely available software such as
385
WinBUGS (http://www.mrc-bsu.cam.ac.uk/bugs/) (references) allows the user to input the prior
386
distribution and relevant data, and then run thousands of iterations of Markov Chain Monte Carlo
387
analysis to create a posterior distribution. This process takes some time depending on the complexity
388
of the prior and the data.
389
390
14
391
Box 2. Bayesian updating for the Normal, Beta and Gamma Distributions
Mathematical Formulae
Part A: Normal distribution
Worked Examples
Sample 1
Sample 2
Sample 3
Example: utility gain of responders
a
0
= prior mean
0.3
0.3
0.3
b
0
= prior standard deviation
0.1
0.1
0.1
c
I0
= 1/σ02 prior precision
1/0.12= 100
1/0.12= 100
1/0.12= 100
d
pop
= patient level standard deviation
0.2
0.2
0.2
e
N
= sample size
50
50
50
f
μ0sample = random sample from N~(0, 0)
0.3545
0.2615
0.1545
g
X
= sample mean from N~(μ0sample, σ2pop/n)
0.3425
0.2389
0.1977
h
2X
= 2pop/n = sample variance
0.22/50 = 0.0008
0.22/50 = 0.0008
0.22/50 = 0.0008
i
IS
= 1/2X = precision of the sample mean
1/0.0008= 1250
1/0.0008= 1250
1/0.0008= 1250
j
I I X
1 0 0 S
I0 I S
100 0.3 1250 0.3425
100 1250
100 0.3 1250 0.2389
100 1250
100 0.3 1250 0.1977
100 1250
= 0.3505
= 0.2644
= 0.1653
k
= posterior mean
2pop / n 2
1 2
2 / n 0
pop
0
= posterior standard deviation
0.0008
0.01
0.01 0.0008
0.0008
0.01
0.01 0.0008
0.0008
0.01
0.01 0.0008
= 0.0272
= 0.0272
= 0.0272
Part B Beta distribution
Example: % response rate for drug
l
a0
= number of patients who responded
7
7
7
m
b0
= number of patients who did not respond
3
3
3
n
0
= a/(a+b) = prior mean
70%
70%
70%
o
20
0.1892
0.1892
0.1892
50
50
50
50.12%
70.63%
90.24%
28
34
43
35
41
50
25
19
10
58%
68%
83%
0.2390
0.2128
0.1366
=
a0b0
= prior variance
(a0 b0 ) (a0 b0 1)
2
p
n
= sample size
q
resp_rate0sample = sample from Beta (a0 b0)
r
y
= sample no. responders | resp_rate0sample
from Binomial (n, resp_rate0sample).
s
a1
= a0 + y
= posterior patients who responded
t
b1
= b0 + n – y
= posterior patients who did not respond
u
1
= a1/(a1+b1) = posterior mean
v
21
=
a1b1
= posterior variance
(a1 b1 ) (a1 b1 1)
2
Part C: Gamma distribution
15
Example: side effects per annum
1
a0
= event rate*(number of patients in study)
1
1
1
2
b0
= 1 / (number of patients in study)
0.25
0.25
0.25
3
0
= a0*b0 = prior mean
25.00%
25.00%
25.00%
4
20
= a0*b02 = prior variance
0.0625
0.0625
0.0625
5
n = sample size
50
50
50
6
sideeffect_rate0sample = from Gamma(a0, b0)
10.07%
21.66%
44.11%
7
(y1, yn) = from poisson (sideeffect_rate0sample)
7
10
20
n
a1 a0 yi
i 1
n
y
i 1
i
8
n
y
i 1
i
11
n
y
i 1
i
21
8
b1
1
(1 / b0 n)
0.0185
0.0185
0.0185
9
1
= a1*b1 = posterior mean
14.81%
20.37%
38.89%
10
21
= a1*b12 = posterior variance
0.0027
0.0038
0.0072
392
393
16
394
Illustrative Model
395
396
To test the algorithm and explore the results, a hypothetical cost-effectiveness model was developed
397
comparing two strategies: treatment with drug T0 versus treatment with drug T1. Figure 2 shows the
398
nineteen model parameters, with prior mean values shown for T0 (column a), T1 (column b) and hence
399
the incremental analysis (column c). Costs for each strategy include “cost of the drug” and cost of
400
hospitalisations - “the percentage of patients receiving the drug who were admitted to hospital” x “days
401
in hospital” x “cost per day in hospital” (e.g. cost of strategy T0 = £1,000 + 10% x 5.20 x £400 =
402
£1,208). Health benefits are measured as QALY gained and come from two sources: responders
403
receive a utility improvement for a specified duration, and some patients have side effects with a utility
404
decrement for a specified duration (e.g. QALY for strategy T0 = 70% responders x 0.3 x 3 years + 25%
405
side effects x –0.1 x 0.5 years = 0.6175). The threshold cost per QALY () is set at £10,000 (i.e. net
406
benefit of T0 is = £10,000* 0.6175 – £1,208 = £4,967) and model results using only central estimates
407
show that T1 (£5,405) has greater net benefit than T0 (£4,967), which means that our baseline decision
408
should be to fund T1.
409
410
Insert Figure 2 –
411
412
The uncertain model parameters are characterised with normal distributions, standard deviations are
413
shown in columns (d) and (e.). Uncertainty in mean drug cost per patient is very low, but other cost
414
related uncertainties in %admissions, length of stay, cost per day are relatively large. For health
415
benefits, uncertainties in % response rates are relatively large, uncertainty in mean utility gain for a
416
responder to T1 is less than that for a responder to T0 (short-term trials of the newer treatment T1 have
417
measured the utility gain more accurately), but uncertainty in the duration of response for T1 is higher
418
(long-term observational data on T1 is not as complete as for T0). The patient level uncertainty for
419
each variable is given in columns (f) and (g).
420
421
The general algorithm for EVSI calculation was applied to the illustrative model using 1000
422
simulations for both the inner and the outer expectations and the formula for normal distributions
423
Bayesian updating from Box 2. The simulations were performed in EXCEL, sampling from normal
424
distributions using the RAND and NORMINV functions together with macro programming to loop the
425
process. EVSI calculations were performed for sample sizes of 10, 25, 50, 100 and 200 in addition to
426
EVPI calculations. The EVSI was analysed for each individual parameter and also five different
427
proposed data collection exercises based on subgroups of parameters. The five subgroups were:- a) a
428
proposed randomised controlled clinical trial measuring only response rate parameters (parameters
429
5,15), b) an observational study on utility only (parameters 6,16), c) a trail combined with utility data
430
collection (parameters 5,6,15,16), d) an observational study of the duration of response to therapy
431
(parameters 7,17) and finally e) a trial combined with utility study alongside an observational study on
432
duration of response (parameters 5,6,7,15,16,17).
433
17
434
Figure 2: Illustrative Model
Part a) Model Parameters and Uncertainty
Model Parameters
Parameter mean Values
T0
a
£1000
10%
5.20
400
70%
0.300
3.0
25%
-0.10
0.50
(1) Cost of Drug T0
(2) % Admissions on T0
(3) Days in Hospital on T0
(4) Cost per day on T0 or T1
(5) % Responding on T0
(6) Utility Change on T0
(7) Duration of response (yrs) on T0
(8) % Side Effects on T0
(9) Change in utility if side effect on T0
(10) Duration of side effect (yrs) on T0
Central Estimate Results
Total Cost
Total QALY
Cost per QALY
Net Benefit of T1 versus T0
Threshold cost per QALY = £10,000
435
(11) Cost of Drug T1
(12) % Admissions on T1
(13) Days in Hospital on T1
(14) Cost per day on T0 or T1
(15) % Responding on T1
(16) Utility Change on T1
(17) Duration of response on T1
(18) % Side Effects on T1
(19) Change in utility if side effect T1
(20) Duration of side effect on T1
£1208
0.6175
£1956
£4967
T1
b
£1500
8%
6.10
400
80%
0.300
3.0
20%
-0.10
0.50
Incremental
c
£500
-2%
0.90
10%
-5%
0.00
-
£1695
0.7100
£2388
£5405
£487
0.0925
£5267
£437.80
Uncertainty in
Parameter Mean
Standard Deviation
T0
T1
d
e
1
1
2%
2%
200
200
200
200
10%
10%
0.100
0.050
0.5
1.0
10%
5%
0.02
0.02
0.20
0.20
Individual Patient
Level Variability
Standard Deviation
T0
T1
f
g
500
500
25%
25%
200
200
200
200
20%
20%
0.200
0.200
1.0
2.0
20%
10%
0.10
0.10
0.80
0.80
Part b) Model Results for Overall Uncertainty
436
Cost Effectiveness Plane from 1,000 samples
Cost Effectiveness Acceptability Curves
437
Cost Effectiveness Acceptability of T1 versus T0
£2,000
438
100%
£1,500
90%
439
80%
£1,000
Inc Cost
£0
-1.4
-1.2
-1
-0.8
-0.6
-0.4
-0.2
0
0.2
-£500
0.4
0.6
0.8
1
1.2
1.4
1.6
Probability Cost Effective
70%
£500
60%
T1
50%
T0
40%
30%
-£1,000
20%
-£1,500
10%
0%
-£2,000
£-
£20,000
£40,000
£60,000
£80,000
Inc QALY
Threshold (MAICER)
£100,000
£120,000
£140,000
18
440
Interpolating the EVSI curve
441
442
The expected value of sample information for a sample size of 50 should clearly be higher than for that for
443
a simple size of n=10, and lower than EVSI for n=100. Thus we expect a smooth curve for the relationship
444
between EVSI and n. The lower bound of EVSI for a sample size of zero is clearly zero (there is no value
445
to be obtained from no data). The upper bound for the curve is given by the expected value of perfect
446
information (there is no greater value to be obtained than that from an infinite sample which produces
447
perfect accuracy for the value of the uncertain parameter). Conceptually we expect that the curve will be
448
monotonic (increases with n) and show diminishing returns (the additional value obtained from increasing
449
the sample size from 5,050 to 5,100 is lower than the value obtained by increasing the sample size from 50
450
to 100. Given this knowledge, a series of exponential form curves were investigated to determine a
451
common functional form for the relationship between EVSI and sample size n.
452
453
454
455
19
456
Results
457
458
Para 1 - Basic model results
459
460
Using prior mean values for illustrative model parameters, the results show a cost difference of £487, with
461
strategy T1 the more expensive. Strategy T1 also has better health outcomes, providing 0.0925 more
462
QALYs. The incremental cost per QALY is £5,267, which is below our decision threshold of £10,000 per
463
QALY. When measured on the net benefit scale, T1 provides £5,405 compared with T0 at £4,967
464
(difference = £437.80), which means that our baseline decision should be to adopt strategy T1.
465
Probabilistic sensitivity analysis confirms this and also shows that T1 provides greater net benefits on
466
54.5% of samples. So, given our existing uncertainty, there is actually a high chance (45.5%) that the
467
alternative strategy T0 would provide more net benefit than current baseline decision T1. This suggests
468
that obtaining more data on the uncertain parameters might help us with our decision. Overall EVPI
469
measures the expected net benefit we would gain if we were to obtain perfectly accurate knowledge about
470
the value of every parameter in the decision model. Overall EVPI for our illustrative model is £1,352 per
471
patient, which is equivalent to 0.1352 QALYs expected gain if perfect knowledge about every parameter
472
were obtained.
473
474
Para 2 - EVSI results for individual parameters, and meaning
475
476
The EVSI results (Table 1 part a) show that further data collection on 6 of the 19 individual model
477
parameters would potentially be valuable. The uncertain parameter with the greatest impact on the current
478
decision is the duration of response on treatment T1. The partial EVPI for this parameter is £803 and the
479
EVSI for a sample of n-50 is £768. The duration of response for patients on T0 causes slightly less
480
decision uncertainty - partial EVPI is £267, and EVSI for n=50 is £256. The second set of important
481
parameters concern utility change if a patient successfully responds to treatment. Utility change on T0
482
response is a key uncertain parameter (EVPI £656, EVSI for n=50 is £617). The final parameters causing
483
decision uncertainty are drug response rates, with both T1 and T0 showing EVSI results for n=50 of the
484
order of £200. Each of the other 13 model parameters had EVSI values lower than £5. For some of the
485
parameters, even small samples would be valuable – some of the EVSI curves (Figure 3) are steep precisely
486
because there is relatively little existing knowledge of the exact values of these important parameters.
487
EVSI for a parameter is often higher if existing uncertainty is higher e.g. standard deviation for mean utility
488
change on T0 response is twice as high as that for utility change on T1 response, and EVSI results are
489
correspondingly higher. However, large uncertainty does not always result in high EVSI values because it
490
is only if the decision between strategies is affected that the uncertainty is relevant. For example, the
491
standard deviation for % side effects on T0 is twice as high as for T1 but both parameters have negligible
492
EVSI results because this uncertainty does not affect the decision.
493
494
20
495
Para 3 - EVSI results for 4 subgroups, and EVSI results for all 6 parameters (i.e. 5 th subgroup)
496
497
EVSI results for groups of parameters are often more useful and relevant in practice than those for single
498
individual parameters. For example, a long-term observational study might measure duration of response
499
for both T0 and T1 (2 model parameters), or a randomised controlled trial might measure response rates
500
and utility changes for both drugs (4 model parameters). EVSI results for parameter groups (Table 1 part
501
b) show that the duration parameters remain the most important pairing, with EVPI for duration of response
502
to both T0 and T1 at £887 and EVSI (n=50) at £856. A study of utilities for both is slightly less valuable
503
(EVSI n=50 is £716), whilst a randomised clinical trial measuring response rates to both drugs is
504
considerably less valuable (EVSI n=50 is £330). A study to measure all 6 of the important model
505
parameters has EVPI of £1,351 and an EVSI for n=50 samples of £1,319. These results also demonstrate
506
that EVSI for a combination of parameters is not the simple addition of EVSI for individual parameters,
507
because parameters interact in the net benefit functions for each strategy. The EVSI curves are relatively
508
steep (Figure 4), with 90% to 95% of the EVPI provided by a sample of n=50, 98% by a sample of n=100,
509
and 99% by a sample of 200.
510
511
Para 4 - EVSI curve fitting
512
513
Investigation of the functional form of the EVSI curves produced a mathematical equation to fit the curves,
514
at least for the illustrative model examined here. The first equations examined followed the form EVSI(n)
515
= EVPI * exp(-λ/n) and EVSI(n) = EVPI * (1 – 1/ (1+n)), but neither provided an adequate fit. The
516
functional form which did fit the curves was EVSI(n) = EVPI * (1 – exp(-*(n))). Given the results for 5
517
different sample sizes, the best fit was calculated using EXCEL Solver to minimise the sum of squared
518
differences between the actual data and the fitted curve on a normalised scale (i.e. dividing each curve by
519
the relevant EVPI so that the maximum value is 1.00). Figure 5 shows the actual data (symbols) and the
520
fitted curve for one parameter, rising form zero and tending to the EVPI. Figure 6 shows all of the curves,
521
with values of ranged from 0.22 to 0.57 for increasing steepness. The sum of squared difference error
522
statistics ranged from 0.0004 to 0.0033, showing a consistently good fit in our illustrative model.
523
524
21
525
Table 2: EVSI per patient based on 1000 x 1000 Monte Carlo Simulations
Part a) EVSI Results for Individual Parameters (£ per patient)
Sample Size
Parameter
10
25
50
100
% responding to T0
172
194
215
222
200
223
Perfect
230
Utility change if respond to T0
526
588
617
644
644
656
Duration of response (years) T0
207
244
256
261
266
267
% responding to T1
146
179
183
192
189
197
Utility change if respond to T1
148
221
250
290
302
320
Duration of response (years) T1
654
741
768
777
796
803
Part b) EVSI Results for Parameter Groups (£ per patient)
% responding to T0 and T1
297
331
330
355
357
359
Utility change if response to T0 and T1
605
669
716
736
769
768
Duration of response to T0 and T1
690
815
856
855
860
887
% responding and utility change if response to
T0 and T1
776
853
878
877
907
916
% responding, utility change and duration of
response to T0 and T1
1100
1217
1277
1310
1321
1350
526
527
22
528
£1,400
Value of Information
£1,200
Duration of reposnse T1
£1,000
Utitlity if T0
£800
Utitlity if T1
Duration of response T0
£600
% Responding T0
% Responding T1
£400
£200
£0
50
100
150
200
250
Sample Size (n)
529
530
Figure 3: EVSI per patient for Individual Parameters
531
532
£1,400
All Six main Paramenters
Value of Information
£1,200
Trial + Utility Study (%
responding & utility T0 & T1)
£1,000
Duration Study (duration of
response to T0 & T1)
£800
Utility Study (Utility T0, Utility T1)
£600
Trial (% reponding T0, %
responding T1)
£400
£200
£0
50
100
150
200
250
Sample Size (n)
533
534
Figure 4: EVSI per patient for Parameter Groups
535
536
23
537
Function : - EVSI = EVPI * [1-
EXP( -0.2181 * sqrt(n)) ]
£400
Value of Information
EVPI = £320
£300
Acutal EVSI
£200
Exponential Fit
£100
£0
50
100
150
200
250
Sample Size (n)
538
539
Figure 5: Fitting an Exponential Functional Form to the EVSI curve – Parameter Utility
540
Function : - EVSI = EVPI * [1-
EXP( * sqrt(n)) ]
£1,600
£1,400
Value of Information
£1,200
£1,000
£800
£600
All Six Main Parameters
0.4989
Trial + Utility Study
0.5654
Duration Study
0.4797
Duration of response T1
0.5187
Utility Study
0.4489
Utility Change respond T0
0.4806
Trial Study
0.5256
Utitlity Change respond T1
0.2181
Duration of response T0
0.4731
% Responding T0
0.4034
% Responding T1
0.4301
£400
Symbols = Acutal EVSI data
£200
Lines = Fitted Exponential Curves
£0
50
100
150
200
250
Sample Size (n)
541
542
Figure 6: Fitting Exponential Functional Forms – All Parameters
543
24
544
Discussion
545
546
Para 1 - Summary of the process, show it can be done and the kind of results that can be obtained.
547
548
The methodology presented here assesses the potential value of different research designs in terms of
549
expected health and monetary gain accruing from the research. The approach demands a clear description
550
of the health policy options in a decision model, a quantified characterisation of the uncertain variables, a
551
description of the proposed data collection exercise, and finally the calculation of expected value of sample
552
information via the 2 level monte carlo simulation incorporating Bayesian updating. The illustrative model
553
demonstrates the feasibility of the approach. The results presented are typical, showing which research is
554
most valuable to the policy decision and what sample sizes would be large enough to aid the decision
555
maker.
556
557
Para 2 – Effect of thinking this way on model construction
558
559
EVSI often has implications for decision model construction and characterisation of uncertainty because
560
possible further data collection forces additional rigour in specifying probability distributions. This rigour
561
applies to the specification of confidence intervals on parameters. The simple task of quantifying an
562
implied sample size n0 for these prior confidence intervals can be useful. For example, we specified a
563
standard deviation of 0.1 for the uncertainty in the mean utility change following response to T0. Given
564
our specified patient level uncertainty of 0.2, we can use a simple formula for the normal distribution case
565
[20 = 2pop/n0] to work out the implied sample size of our specified prior uncertainty. The result is n0=2
566
for mean utility change following response to T0 and n0=4 for the mean utility change following response
567
to T1, while the equivalent calculations for cost of the drugs gives n0=500. This explains the high EVSI for
568
utilities parameters in our model and the low EVSI for costs of drugs. The rigour also applies to the
569
mathematical form of the probability distributions. Triangular distributions may sometimes be considered,
570
but as soon as the analyst considers the properties of the individual patient level data, the triangular
571
specification is often seen to be inappropriate. We characterised the uncertainty in mean response rate to
572
T0 as a normal distribution, which might be reasonable large sample sizes, as the central limit theorem
573
suggests uncertainty in a sample mean follows a normal distribution. However, data on an individual
574
patient will measure whether there is response i.e. a Yes or No dichotomous variable, and so it is clear that
575
a Beta distribution is the correct characterisation of uncertainty in mean response rate. Sometimes analysts
576
might consider expressing the uncertainty in mean utility as a Beta distribution, the rationale being it would
577
lie between 0 to 1 and many probability distribution shapes are possible. However, we know the Beta
578
distribution must have individual level data that is dichotomous, and it is clear that individual patient level
579
utility data would not just produce 0 or 1 but individual results anywhere on the range between. A normal
580
distribution may well be the correct approach for characterising uncertainty in mean utility.
581
25
582
Para 3 Correlation
583
584
EVSI also brings into focus the correlation between uncertain parameters. This can have at least two
585
effects. Firstly, data collected about one parameter may also provide evidence about another parameter.
586
For example discovering that the utility change for a responder to T0 is actually at the high end of its prior
587
uncertain range may well imply that the utility change for a responder to T1 may also be higher than
588
expected. Building correlations into the model of uncertainty would therefore be important. One way to
589
achieve this is to restructure the model so that utility of T0 is an uncertain parameter and then the difference
590
between T1 and T0 utility is a second uncertain parameter. Another way would be to sample the 2
591
parameters as part of a multi-variate joint normal distribution with a specified variance-covariance matrix,
592
incorporating the covariance to reflect our knowledge about correlation. This is less easy in EXCEL but
593
straightforward in software such as R. Both of these re-parameterisations would affect the C-E plane
594
scatter-plot and the CEAC curve for the decision model. The second effect is that the extent of correlation
595
itself may be an uncertain variable. Thus correlation moves from affecting the shape of uncertainty in the
596
C-E plane scatter-plot, to being a parameter within the model itself upon which EVPI and EVSI
597
calculations can be done – how valuable would policy decision makers consider data on correlation
598
between variables? This may be particularly useful in the context of epidemiological or observational
599
studies, where the underlying causality of disease or health system processes is being explored. A further
600
intensification of the methodology would involve incorporating the existing evidence on related parameters
601
into a WinBUGs based evidence synthesis to determine an integrated analysis of correlations, variable
602
dependence and probability distributions before the EVSI calculations are performed.
603
604
Para 4- Further methods development work Computation time issues are important
605
606
Some further development of the method would be useful, particularly how to deal with probability
607
distributions beyond the normal, beta and gamma. Work is needed on other conjugate distributions, to
608
produce additional formulae for Bayesian updating and to examine their usefulness in the context of real
609
decision models. For non-conjugate distributions there are two options. One option for Bayesian updating
610
would be to use MCMC methods (refs ?include Jim transplantation work), although this would incur
611
significant additional computation on each sample of the possible data collected. The only other option is
612
to use approximation methods, the topic of our current investigations (Ref both Laplace approximation and
613
Weibull MDM abstracts). Work is needed also to improve computational efficiency. In our study on EVPI
614
calculations (ref EVPI paper) we explored the number of outer and inner level simulations required to
615
achieve accurate results in the 2 level algorithm. The same issues apply in EVSI and work to establish a
616
rule of thumb for the number of inner and outer level simulations would be useful. For computationally
617
intensive decision models, e.g. patient level simulation models of one hour per model run, the replacing the
618
model with an emulator or meta-model is valuable (ref Paul Simon and Jim’s MS EVI). The emulator
619
produces similar results but in a fraction of the time enabling 2 nd order simulations for EVSI to be
26
620
undertaken in a reasonable time. A particularly useful approach is the Gaussian process emulator (Ref
621
Jeremy and Matt)
622
623
Para 5 – Generaliseability
624
625
The algorithm and mathematics presented are generalisable to any decision model with any decision rule.
626
The exponential functional form for EVSI curves is not however. It has a shape showing even small
627
samples of data would be valuable. Consider an instance where a moderate amount of clinical trial data
628
already exists and a further very small trial is planned. Conceptually one would expect that the new very
629
small trial would add little to the policy decision, especially if the trial protocol or setting is slightly
630
different to the earlier study implying the potential for a biased or skewed sample from the underlying
631
population. If a larger new trial were planned, of size equal to the original, then this may have substantial
632
impact on the decision, for example through formal meta-analysis of the two studies. If an extremely large
633
trial were planned, say 50 times larger than the original, then one would expect the new study to dominate
634
the evidence and be of considerable value. This suggests that EVSI curves may be S shaped in some
635
circumstances rather than the inverted exponential shown in our study. This conceptual thinking also
636
suggests that it may be necessary to extend EVSI calculation methods to incorporate possible bias, or
637
heterogeneity between planned trials and those making up the existing prior evidence.
638
639
Para 6 – Implications - for related fields
640
641
How this approach relates to the traditional frequentist approach for calculating sample size for a clinical
642
trial also requires research. The traditional approach (refs ? Machin,?) specifies a clinically significant
643
difference , and assesses the probability that such a difference would be found in the trial by pure chance
644
if in fact there were no true difference between treatments. The traditional levels of significance () and
645
power () are used to determine the sample size n, which would show that a true clinically significant
646
difference exists. There are many issues which Bayesian statisticians view as ill-conceived with this
647
approach, not least the lack of accounting for existing prior evidence. However, it is used across the world
648
in commercial and governmental contexts and delivers the benefits of simplicity and useability. It would
649
be useful to research the comparison of sample size results against the EVSI approach. There is a link - in
650
the traditional approach, the implied decision rule is that clinicians will adopt a treatment with a proven
651
clinically significant difference . In the EVSI approach, the decision model rule is that policy makers will
652
adopt a treatment if its cost-effectiveness is below . Given the enormous expansion of health economics
653
as an influencing factor over the adoption of new treatments, it is clear that these two modelled decision
654
rules are linked and likely to be coming closer together. There are likely to be mathematical modelling
655
methods to examine the interaction between the two approaches, as well as more pragmatic studies of how
656
decisions are really made and which decision model is closest to real life. In the first instance, comparison
657
of the implied sample sizes of the two approaches in the design of clinical trials would aid understanding.
27
658
659
A key advantage of the EVSI approach is that is helps consider the value other kinds of data collection,
660
including economic cost and quality of life data, not just clinical efficacy. The traditional approach on
661
these issues is to consider data collection on resource use and sometimes quality of life data alongside
662
clinical trials. The illustrative model demonstrates common problems with this, i.e. long-term follow-up on
663
disease progression is often more important than another trial, resource use within clinical trials is often the
664
same between two arms, and quality of life data is necessary.
665
666
Para 7 - Importance of this approach
667
668
The EVSI calculations shown here take a societal perspective on the value of the research and are therefore
669
directly relevant to governmental agencies funding health technology assessments. They are also of value
670
to commercial investors in research because they prefigure the likely cost-effectiveness and uncertainty
671
analysis which governmental reimbursement authorities in many countries use to assess pharmaceuticals.
672
Thus commercial companies might utilise this approach to predict the likely response of governemental
673
agencies concerning the evidence gaps in a reimbursement analysis, and hence commission related studies
674
to their existing product evidence earlier in the process. Finally ofcourse, the decision rule used for
675
adoption can be re-examined in terms of commercial incenticves and models of the sales, profit and
676
payback on commercial research incorporated into the framework in order to make explicit decisions in the
677
R&D cycle of product development on the value of further data collection. (? Ref Neil Hawkins or papers
678
from FF 6).
679
680
Para 8- Sum up the conclusion and importance of this paper.
681
682
In summary, this paper presents a clear methodology for assessing the value of different research designs in
683
terms of expected health and monetary gain accruing from the research. The mathematics and algorithm
684
are generaliseable to many situations and the illustrative model demonstrates the feasibility of the approach.
685
It is hoped that the approach will now be implemented in many more health economic evaluations, as a
686
relatively simple extension of probabilistic sensitivity analysis. This in turn, should lead to a more coherent
687
analysis of the prioritisation and design of health technology assessment studies.
688
689
690
691
28
692
References
693
694
Eddy DM. Selecting technologies for assessment. Int J Technol Assess Health Care 1989; 5: 485-501.
695
696
Townsend J, Buxton M. Cost effectiveness scenario analysis for a proposed trial of hormone replacement
697
therapy. Health Policy 1997; 39: 181-94.
698
699
Davies L, Drummond M, Papanikoloau P. Prioritising investments in Health Technology Assessment: can
700
we assess the potential value for money? Discussion Papers. York: University of York Centre for Health
701
Economics; 1999. 170.
702
703
Detsky AS. Using cost-effectiveness analysis to improve the efficiency of allocating funds to clinical trials.
704
Stat Med 1990; 9: 173-84.
705
706
Drummond MF, Davies LM, Ferris FL III. Assessing the costs and benefits of medical research: the
707
diabetic retinopathy study. Soc Sci Med 1992; 34: 973-81.
708
709
Buxton M, Elliott R, Hanney S, Henkel M, Keen J, Sculpher M, Youll P. Assessing payback from
710
Department of Health research and development: preliminary report, Vol. 2, Eight case studies. Uxbridge:
711
Health Economics Research Group, Brunel University; 1994. 19 Part 2.
712
713
Claxton K, Posnett J. An economic approach to clinical trial design and research priority-setting. Health
714
Econ 1996; 5: 513-24.
715
716
Claxton K, Neumann PJ, Araki S, Weinstein MC. Bayesian value-of-information analysis. An application
717
to a policy model of Alzheimer’s disease. Int J Technol Assess Health Care 2001; 17: 38-55.
718
719
29