BONE & JOINT INFECTIONS
advertisement
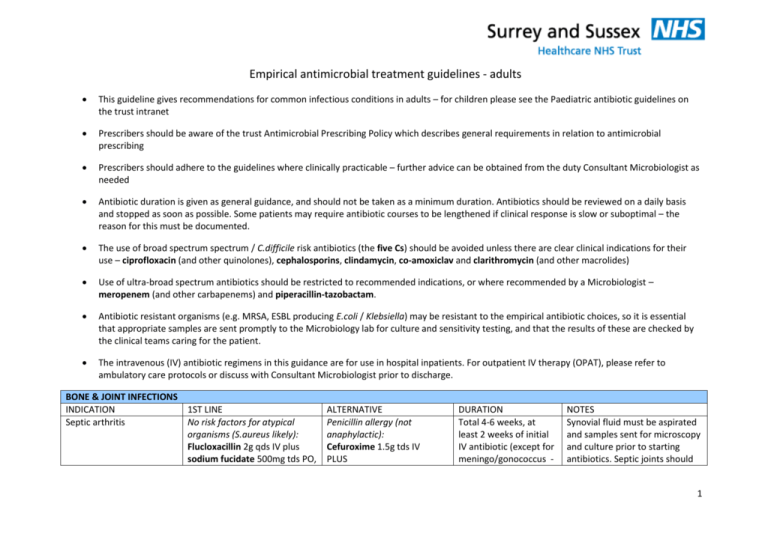
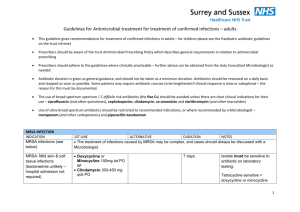
Empirical antimicrobial treatment guidelines - adults This guideline gives recommendations for common infectious conditions in adults – for children please see the Paediatric antibiotic guidelines on the trust intranet Prescribers should be aware of the trust Antimicrobial Prescribing Policy which describes general requirements in relation to antimicrobial prescribing Prescribers should adhere to the guidelines where clinically practicable – further advice can be obtained from the duty Consultant Microbiologist as needed Antibiotic duration is given as general guidance, and should not be taken as a minimum duration. Antibiotics should be reviewed on a daily basis and stopped as soon as possible. Some patients may require antibiotic courses to be lengthened if clinical response is slow or suboptimal – the reason for this must be documented. The use of broad spectrum spectrum / C.difficile risk antibiotics (the five Cs) should be avoided unless there are clear clinical indications for their use – ciprofloxacin (and other quinolones), cephalosporins, clindamycin, co-amoxiclav and clarithromycin (and other macrolides) Use of ultra-broad spectrum antibiotics should be restricted to recommended indications, or where recommended by a Microbiologist – meropenem (and other carbapenems) and piperacillin-tazobactam. Antibiotic resistant organisms (e.g. MRSA, ESBL producing E.coli / Klebsiella) may be resistant to the empirical antibiotic choices, so it is essential that appropriate samples are sent promptly to the Microbiology lab for culture and sensitivity testing, and that the results of these are checked by the clinical teams caring for the patient. The intravenous (IV) antibiotic regimens in this guidance are for use in hospital inpatients. For outpatient IV therapy (OPAT), please refer to ambulatory care protocols or discuss with Consultant Microbiologist prior to discharge. BONE & JOINT INFECTIONS INDICATION 1ST LINE Septic arthritis No risk factors for atypical organisms (S.aureus likely): Flucloxacillin 2g qds IV plus sodium fucidate 500mg tds PO, ALTERNATIVE Penicillin allergy (not anaphylactic): Cefuroxime 1.5g tds IV PLUS DURATION Total 4-6 weeks, at least 2 weeks of initial IV antibiotic (except for meningo/gonococcus - NOTES Synovial fluid must be aspirated and samples sent for microscopy and culture prior to starting antibiotics. Septic joints should 1 Followed by: Flucloxacillin 500mg-1g qds po plus sodium fucidate 500mg tds PO. Sodium fucidate 500mg tds PO discuss with Microbiologist) Severe reactions to betalactams: Teicoplanin 800mg IV stat then: if < 80kg – 400mg IV od if >80kg - 600mg IV od PLUS Sodium fucidate 500mg tds PO Risk factors for atypical organisms (e.g. elderly, recent abdominal surgery, MRSA risk, suspected, meningo/gonococcus, IVDA, ICU patient) – discuss with Micro Infection of orthopaedic prostheses CENTRAL NERVOUS SYSTEM INDICATION 1ST LINE Bacterial meningitis Cefotaxime 2g qds IV (covers N.meningitidis, S.pneumoniae & Haemophilus) For adults >55yrs without typical meningococcal rash, or immunocompromised patient, consider addition of amoxicillin 2g 4-hourly IV (to cover Listeria) be aspirated to dryness as often as required. Patient should be referred to an Orthopaedic Surgeon Directed antibiotic therapy is based on the results of culture of operative samples For empirical therapy, discuss with Microbiologist ALTERNATIVE If history of severe betalactam allergy: Chloramphenicol 25mg/kg qds IV (reduce dose as soon as clinically indicated) PLUS Co-trimoxazole 60120mg/kg/day in 2-4 divided doses if suspected Listeria meningitis DURATION 7 days (meningococcus) 10 days (Haemophilus) 14 days (pneumococcal) 21 days (Listeria) NOTES Acute meningitis is notifiable (to Local Authority Proper Officers) under the Health Protection (Notification) Regulations 2010 Patients with suspected meningococcal disease must be isolated for the first 48hrs of treatment Continued antibiotics should be guided by results of CSF and/or blood culture 2 Patients with probable or confirmed meningococcal disease must be given ciprofloxacin 500mg stat po to eradicate throat colonisation Where pneumococcal meningitis is suspected or possible, consider to start dexamethasone 0.15mg/kg qds for 4 days started with or just before the first dose of antibiotic Antibiotic prophylaxis of family contacts may be indicated if probable or confirmed meningococcal disease – discuss with Health Protection Unit. Herpes simplex encephalitis EYE INFECTIONS INDICATION Bacterial conjunctivitis GENITAL INFECTION INDICATION Bacterial vaginosis Acyclovir 10mg/kg tds IV (usually 750mg tds IV) 10-21 days Adequate hydration is required since dehydration increases risk of nephrotoxicity 1st LINE Chloramphenicol 0.5% eye drops, 2-hourly initially, then 4to 6-hourly as infection responds ALTERNATIVE Neomycin 0.5% eye drops 2hourly initially, then 4- to 6hourly as infection responds DURATION Until 48 hours after resolution NOTES Discuss with Ophthalmology if severe 1ST LINE Metronidazole 400mg bd for 7 days OR ALTERNATIVE Metronidazole 0.75% vaginal gel 5g at night for 5 nights OR DURATION See text NOTES Oral metronidazole is as effective as topical therapy, and cheaper 3 Metronidazole 2g stat Clindamycin 2% cream 5g at night for 7 nights Ceftriaxone 500mg stat IM PLUS Doxycycline 100mg bd PO PLUS Metronidazole 400mg bd PO Ofloxacin 400mg bd PO PLUS Metronidazole 400mg bd PO Pelvic sepsis Pelvic inflammatory disease (PID) 14 days (ceftriaxone is a single dose) Ceftriaxone may be omitted if low risk of gonorrhoea Premature rupture of membranes / group B strep prophylaxis Vaginal candidiasis Less relapse with 7 day metronidazole regimen than 2g stat regimen Avoid 2g stat regimen if breastfeeding Treating partners does not decrease relapse rate See section on intra-abdominal sepsis Avoid ofloxacin regimen if high risk of gonococcal PID Essential to test for gonorrhoea and Chlamydia (refer to GUM) Metronidazole may be omitted from the 1st line regimen if side effects are not tolerated. See Maternity Department protocols Clotrimazole 500mg pessary or 10% cream STAT OR Fluconazole 150mg STAT PO INTRA-ABDOMINAL SEPSIS INDICATION 1ST LINE Acute pancreatitis In pregnancy: Avoid oral azole and give intravaginal treatment for 7 days Clotrimazole 100mg pessary at night for 6D Miconazole 2% cream 5g intravaginally bd for 7 days See text All topical and oral azoles give 75% cure ALTERNATIVE DURATION NOTES Antibiotic not given as a routine unless clear clinical evidence of sepsis 4 Gastro-enteritis / food poisoning Intra-abdominal sepsis – appendicitis Amoxicillin 1g tds IV Plus Gentamicin 5mg/kg IV once daily Plus Metronidazole 500mg tds IV If renal impairment (eGFR <60mL/min): Piperacillin-tazobactam 4.5g tds IV If penicillin allergy: Teicoplanin 800mg IV stat then 400mg od (if <80kg) or 600mg IV od (if >80kg) plus Gentamicin 5mg/kg IV once daily Plus Metronidazole 500mg IV tds 5 days if generalised / complicated. 24 hours antibiotics adequate if localised / simple. Bacterial gastroenteritis (e.g. Salmonella / Campylobacter) generally does not require antibiotic treatment Antibiotics should be avoided in colitis due to E.coli O157 (VTEC) because of the increased risk of precipitating haemolytic-uraemic syndrome Serum levels must be checked regularly on all patients receiving regular gentamicin – see gentamicin section of antibiotic guidelines. MAXIMUM 5 DAYS DURATION FOR GENTAMICIN. Avoid repeated gentamicin courses for the same admission. Discuss with Microbiologist if >5 days required. PO switch option: Co-amoxiclav 625mg tds PO, or if penicillin allergic (not anaphylactic) cefalexin 500mg tds PO plus metronidazole 400mg tds PO. 5 Intra-abdominal sepsis – biliary tract (cholecystitis, cholangitis) Co-amoxiclav 1.2g tds IV Followed by co-amoxiclav 625mg tds PO If severe: Piperacillin-tazobactam 4.5g tds IV Followed by co-amoxiclav 625mg tds PO If history of severe allergy to penicillins, use ciprofloxacin 500mg bd PO plus metronidazole 400mg tds PO. Penicillin allergy: Cefuroxime 1.5g tds IV PLUS Metronidazole 500mg tds IV, Followed by Cefalexin 500mg tds PO Plus Metronidazole 400mg tds PO 5-7 days for cholecystitis, 5 days after relief of obstruction for cholangitis Co-amoxiclav is 6 times more likely to cause a cholestatic jaundice than amoxicillin. This can be dangerous, but full recovery is the rule. 5 days for uncomplicated disease. Serum levels must be checked regularly on all patient receiving regular gentamicin – see gentamicin section of antibiotic guidelines. Severe penicillin allergy: Teicoplanin 800mg IV stat then 400mg od (if <80kg) or 600mg IV od (if >80kg) Plus Ciprofloxacin 400mg bd IV followed by 500mg bd PO Plus Metronidazole 500mg tds IV followed by 400mg tds PO Intra-abdominal sepsis diverticulitis Gentamicin 5mg/kg IV once daily Plus Metronidazole 500mg tds IV If renal impairment (eGFR <60mL/min): Piperacillin-tazobactam 4.5g tds IV PO switch option: Co-amoxiclav 625mg tds PO, Longer courses may be required – discuss with Consultant Microbiology for choice MAXIMUM 5 DAYS DURATION 6 or if penicillin allergic (not anaphylactic) cefalexin 500mg tds PO plus metronidazole 400mg tds PO. of agent FOR GENTAMICIN. Avoid repeated gentamicin courses for the same admission. Discuss with Microbiologist if >5 days required. 5 days where there is adequate source control (e.g. drainage/debridement). Where source control is not possible (e.g. abscess, persistent colonic leak) a longer duration of antibiotic will be required. Serum levels must be checked regularly on all patients receiving regular gentamicin – see gentamicin section of antibiotic guidelines. If history of severe allergy to penicillins, use ciprofloxacin 500mg bd PO plus metronidazole 400mg tds PO. Intra-abdominal sepsis – peritonitis Amoxicillin 1g tds IV Plus Gentamicin 5mg/kg IV once daily Plus Metronidazole 500mg tds IV If renal impairment (eGFR <60mL/min): Piperacillin-tazobactam 4.5g tds IV If penicillin allergy: Teicoplanin 800mg IV stat then 400mg od (if <80kg) or 600mg IV od (if >80kg) plus Gentamicin 5mg/kg IV once daily Plus Metronidazole 500mg IV tds PO switch option: Co-amoxiclav 625mg tds PO, or if penicillin allergic (not anaphylactic) cefalexin 500mg tds PO plus metronidazole 400mg tds Discuss with Microbiologist for antibiotic options where prolonged antibiotics are needed . For discharge possibilities may be oral antibiotics or outpatient IV antibiotics (OPAT). MAXIMUM 5 DAYS DURATION FOR GENTAMICIN. Avoid repeated gentamicin courses for the same admission. Discuss with Microbiologist if >5 days required. 7 PO. If history of severe allergy to penicillins, use ciprofloxacin 500mg bd PO plus metronidazole 400mg tds PO. Liver abscess Piperacillin-tazobactam 4.5g tds IV PLUS Metronidazole 400mg tds PO Penicillin allergy: Teicoplanin 800mg IV stat then 400mg od (if <80kg) or 2-6 weeks -Send serum for amoebic serology -Send pus for culture and adjust antibiotic regimen as per sensitivity results -Avoid long courses of metronidazole wherever possible given risk of toxicity e.g. peripheral neuropathy -Discuss antibiotic options with Microbiologist at the time of hospital discharge DURATION 10 days NOTES Most cases are self limiting viral infections which do not need antibiotics If patient has had more than 5 days of oral Penicillin V then use Co-amoxiclav 1.2g IV TDS. If patient has infectious mononucleosis (glandular fever) and >5 d oral Penicillin V use Cefuroxime 750mg IV TDS and 600mg IV od (if >80kg) plus Ciprofloxacin 500mg BD PO plus Metronidazole 400mg tds PO RESPIRATORY TRACT – UPPER INDICATION 1ST LINE Bacterial tonsillitis / Penicillin V 500mg qds PO pharyngitis Severe Tonsillitis Benzyl Penicillin 1.2 g qds IV PLUS Metronidazole 400mg tds PO (500mg IV TDS if unable to swallow) ALTERNATIVE Penicillin allergy: Clarithromycin 250-500mg bd PO Clarithromycin 500mg IV BD PLUS Metronidazole 400mg PO TDS (500mg IV TDS if unable to swallow) 10 days (switch to PO when possible) 8 Acute otitis media Amoxicillin 500mg tds PO Penicillin allergy: Clarithromycin 250-500mg bd PO 5 days Malignant otitis externa Piperacillin/ tazobactam 4.5g tds IV Consult microbiologist Acute Parotitis Co-amoxiclav 1.2g tds IV Acute Mastoiditis Co-amoxiclav 1.2g tds IV Clarithromycin 500mg bd IV PLUS Metronidazole 400mg tds PO (500mg tds IV if unable to take PO) Cefuroxime 1.5g tds IV PLUS Metronidazole 400mg tds PO (500mg tds IV if unable to take PO) Prolonged IV may be required – Consult microbiologist 7 days If severe type 1 hypersensitivity (anaphylaxis): Teicoplanin 400mg od IV PLUS Ciprofloxacin 500mg bd PO PLUS Metronidazole (as above). 7 days Metronidazole 500mg IV TDS OM resolves in 24h in 60% without antibiotics and does not prevent deafness. Consider 2 or 3 day delayed antibiotics. Immediate antibiotics indicated if otorrhoea. Review microbiology results IV Clarithromycin - risk of phlebitis. Switch to PO as soon as possible Consider PO switch ASAP Switch Co-amoxiclav 1.2g IV to 625mg tds PO If penicillin allergy: Switch Cefuroxime 1.5g IV + Metronidazole 500mg IV to Cefalexin 500mg tds PO and Metronidazole 400mg tds PO If severe type 1 hypersensitivity(anaphylaxis): Teicoplanin 400mg IV - no PO equivalent (consult microbiologist) PLUS Ciprofloxacin 400mg bd PO PLUS 9 Metronidazole 400mg tds PO Acute rhinosinusitis 7 days Consider delayed 7 day antibiotics Immediate antibiotics if purulent nasal discharge Consider Azithromycin or Doxycycline in patients not tolerating / allergic to Clarithromycin. Up to 8 weeks Recommended as per EPOS2012 (European Position Paper on Rhinosinusitis) Benzyl Penicillin 1.2 g qds IV PLUS Metronidazole 400mg tds PO (500mg IV TDS if unable to swallow) Clarithromycin 500mg bd IV PLUS Metronidazole 400mg tds PO (500mg tds IV if unable to take PO) 10 days If patient has had a course of oral Penicillin V then use Cefuroxime 750mg tds IV PLUS Metronidazole 500mg tds IV Cefuroxime 1.5g tds IV PLUS Metronidazole 400mg tds PO (500mg tds IV if unable to swallow) Consult microbiologist only if type 1 anaphylaxis 7-10 days ALTERNATIVE Or, if penicillin allergy: Doxycycline 100mg bd PO DURATION 5 days Amoxicillin 500mg tds PO Doxycycline 100mg bd PO (double dose if severe) If persistent infection: use agent to cover anaerobes - Co-amoxiclav 625mg tds PO OR add Metronidazole 400mg tds PO to Doxycycline Chronic rhinosinusitis Clarithromycin 500mg bd PO for 2 weeks followed by Clarithromycin 250mg bd PO for up to 8weeks Peritonsillar abscess (Quinsy) Supraglottitis RESPIRATORY TRACT - LOWER INDICATION 1ST LINE Acute bronchitis Usually none, but if severe: Amoxicillin 500mg tds PO NOTES Predominantly viral – antibiotics usually not required in previously healthy adults 10 Acute exacerbation of COPD Amoxicillin 500mg tds PO (1g tds IV for first 48hrs if severe) Doxycycline 100mg bd PO If severe, or no response to 1st line: Co-amoxiclav 1.2g tds IV for 48hrs, then 625mg tds PO OR If penicillin allergy (not anaphylactic) and severe, or no response to 1st line: Cefuroxime 1.5g tds IV for 48hrs, followed by Cefalexin 500mg tds PO to complete 5 days If severe reaction to betalactams: Clarithromycin 500mg bd PO (500mg bd IV for first 48hrs if severe) 5 days Community acquired pneumonia (CAP) – mild CURB-65 score <1 Amoxicillin 500mg – 1g tds PO Doxycycline 100mg bd PO OR Clarithromycin 500mg bd PO 5-7 days Community acquired pneumonia (CAP) moderate CURB-65 score >2 Benzylpenicillin 1.2g qds IV initially, then amoxicillin 500mg-1g tds po PLUS Clarithromycin 500mg bd po (IV for first 48hrs if required) Switch from IV to PO antibiotic at 48hrs if improving If penicillin allergy: Doxycycline 100mg bd PO 7 days If risk factors for resistant organisms, see section below. If penicillin allergy and unable to take oral medication: Teicoplanin 800mg IV stat then: if < 80kg – 400mg IV od if >80kg - 600mg IV od PLUS COPD exacerbations are often caused by viruses, but bacterial infection may co-exist. Antibiotics are indicated if: Increased volume of sputum Increased purulence of sputum Increased shortness of breath IV antibiotics should be converted to oral equivalents once fever has resolved (usually within 48hrs). Do not give a macrolide (e.g. clarithromycin) as a matter of routine unless evidence of pulmonary infiltrates on CXR or patient is allergic to penicillin. CAP should have evidence of consolidation on CXR Use CURB-65 score for severity assessment, score must be documented. Assign one point to each of the following: -Mental Confusion -Urea >7mmol/L (disregard if pre-existing) -Respiratory rate >30/min 11 Clarithromycin 500mg bd IV Followed by switch to PO doxycycline after 48hrs -Blood pressure systolic <90mmHg or diastolic <60mmHg -Age >65yrs If severe (anaphylactic) penicillin allergy and unable to take oral medications: Teicoplanin 800mg IV stat then: if < 80kg – 400mg IV od if >80kg - 600mg IV od PLUS Levofloxacin 500mg bd IV Followed by switch to PO doxycycline after 48hrs Community acquired pneumonia (CAP) in patients with risk factors for resistant organisms, or if recommended by Consultant Chest Physician or Microbiologist: Risk factors: - admission to ICU - hospitalised with 14 days - significantly immunocompromised: - HIV infection >10mg/day prednisolone other immunosuppressive agents Co-amoxiclav 1.2g tds IV initially, then Co-amoxiclav 625mg tds PO PLUS Clarithromycin 500mg bd IV, followed by Clarithromycin 500mg bd PO If penicillin allergy: Cefuroxime 1.5g tds IV PLUS Clarithromycin 500mg bd IV, followed by a switch to Doxycycline 100mg bd PO If severe (anaphylactic) penicillin allergy: Teicoplanin 800mg IV stat then: if < 80kg – 400mg IV od if >80kg - 600mg IV od PLUS Levofloxacin 500mg bd IV When clinically resolving switch to Doxycycline 100mg bd PO Up to 3 weeks antibiotic treatment may be required if atypical cause suspected or confirmed (e.g. Legionnaires’ disease) CURB-65 score >3 = severe CAP. Requires hospital admission. Send urine for Legionella and pneumococcal antigen. 7 days If condition of mild/moderate CAP worsens after 48hrs of antibiotic therapy, treat as sever CAP. If MRSA colonised, consider addition of teicoplanin. Narrow spectrum antibiotic therapy (e.g. benzylpenicillin + clarithromycin) is validated in patients who do not have risk factors for resistant organisms (Charles PG et al, Clin Infect Dis 2008; 46:1512-21) 12 - - active treatment for cancer prior organ transplantation Primary atypical pneumonia Clarithromycin 500mg bd IV/PO Switch from IV to PO at 48hrs if improving Legionnaires’ disease: In addition to clarithromycin, add Rifampicin 300-600mg bd PO Psittacosis: Use a tetracycline e.g. Doxycycline 100mg bd PO 14 days, may require up to 21 days Send urine for antigen testing where Legionella suspected Mycoplasma can be detected by sending nose/throat viral swabs for respiratory PCR Psittacosis – diagnosis is by serology – discuss with Microbiologist where suspected Aspiration pneumonia Amoxicillin 500mg tds PO (IV 500mg-1g tds IV for first 48hrs if required) PLUS Metronidazole 500mg IV / 400mg PO tds If penicillin allergy: Doxycycline 100mg bd PO PLUS Metronidazole 500mg IV / 400mg PO tds If unable to take PO medication, replace doxycycline with Teicoplanin 800mg IV stat then: if < 80kg – 400mg IV od if >80kg - 600mg IV od 5-7 days Routine antibiotic treatment is not required for aspiration unless there is persistence of chest signs or fever for 48hrs post aspiration. Community acquired pneumonia (CAP) in patients with influenza like illness (influenza season) Treat for CAP as above. If treated with Benzylpenicillin or Amoxicillin, add Flucloxacillin 500mg-1g qds IV Penicillin allergy: Treat as above for CAP Treat influenza with oseltamivir / zanamivir Additional flucloxacillin not required for patients receiving co-amoxiclav, cefuroxime or 13 Hospital acquired LRTI without pneumonia Doxycycline 100mg bd PO If failed recent course of doxycycline: Co-amoxiclav 625mg tds PO 5 days Hospital acquired pneumonia (HAP) – nonsevere Doxycycline 100mg bd PO If severe (anaphylactic) penicillin allergy: 5-7 days If contraindication to doxycycline or unresponsive to doxycycline: Co-amoxiclav 625mg tds PO (1.2g tds IV for first 48hrs if required), Or if penicillin allergy: Cefuroxime 1.5g tds IV (add metronidazole if aspiration suspected) Levofloxacin 500mg bd IV/PO Add Metronidazole if suspected aspiration. Diagnosis of HAP: New or progressive infiltrate + clinical characteristics plus at least one of: -Fever >38oC -Leucocytosis or leucopenia -Purulent secretions If unresponsive after 48hrs treatment, treat as severe HAP If unresponsive after 48hrs treatment, treat as severe HAP Hospital acquired pneumonia (HAP) – severe (not Pseudomonas, not ventilated) Amoxicillin 1g IV tds plus Temocillin 2g IV bd Replace Amoxicillin with Teicoplanin or Vancomycin if known MRSA colonised Add Flucloxacillin if methicillin- If penicillin allergy (not severe): Meropenem 500mg tds IV (1g tds IV if ICU). Add Teicoplanin or Vancomycin if known MRSA colonised teicoplanin. Not indicated in the absence of purulent / mucopurulent sputum. Of most benefit if patient has increased dyspnoea and increased purulent sputum. Hospital acquired pneumonia is defined as pneumonia that occurs 48 hours or longer after admission or admission within the last 7 days. 7 days (10-14 days if S.aureus) Routine antibiotic treatment is not required for aspiration unless there is persistence of chest signs or fever for 48hrs post aspiration. -Temocillin is not active vs Pseudomonas or staphylococci – add additional antibiotic as suggested if colonised with these -There are no UK guidelines to assess severity of HAP, but the following criteria, in addition to the HAP features above, would 14 sensitive (MSSA) colonised Add Clarithromycin if suspected atypical pneumonia Add Metronidazole if suspected aspiration Hospital acquired pneumonia (HAP) – ventilator associated pneumonia or colonised with Pseudomonas SOFT TISSUE INFECTION INDICATION Animal or human bite Piperacillin-tazobactam 4.5g tds IV Add Teicoplanin or Vancomycin if known MRSA colonised Add Clarithromycin if suspected atypical pneumonia 1ST LINE Co-amoxiclav 625mg tds PO suggest severe pneumonia: New mental confusion Respiratory rate 30/min or more Hypoxia (PaO2 <8kPa or SaO2 <92% on any FiO2) Bilateral or multilobular chest XRay shadowing Blood pressure systolic BP <90mmHg or diastolic <60mmHg Add Clarithromycin if suspected atypical pneumonia If severe penicillin allergy: Teicoplanin 800mg IV stat then: if < 80kg – 400mg IV od if >80kg - 600mg IV od PLUS Ciprofloxacin 400mg bd IV Add Metronidazole if suspected aspiration Teicoplanin 800mg IV stat then: if < 80kg – 400mg IV od if >80kg - 600mg IV od PLUS Ciprofloxacin 400mg bd IV ALTERNATIVE Penicillin allergic: Doxycycline 100mg bd PO PLUS Metronidazole 400mg tds PO 7 days (10-14 days if S.aureus or P.aeruginosa) DURATION 7 days NOTES Prophylactic course may be shorter (5 days) Alternative options for penicillin allergy are less effective and patient progress should be reviewed If human bite, assess risk fo blood borne viruses (hepatitis B & C, HIV) 15 If animal bite abroad, assess risk of rabies Cellulitis of limb – mild (No signs of systemic toxicity & no uncontrolled co-morbidities) Flucloxacillin 500mg qds PO Penicillin allergic: Clarithromycin 500mg bd PO 7 days Cellulitis of limb – moderate / severe (Sepsis syndrome or complicating comorbidities) Benzylpenicillin 1.2g qds IV PLUS Flucloxacillin 1g qds IV, Penicillin allergic / MRSA colonised: Teicoplanin 800mg IV stat then: if < 80kg – 400mg IV od if >80kg - 600mg IV od 7-10 days Diabetic foot – infection of soft tissue / cellulitis without ulceration Diabetic foot ulcer When clinically improving switch to flucloxacillin 500mg qds PO Non severe: Flucloxacillin 500mg qds PO Severe: Flucloxacillin 2g qds IV then to flucloxacillin 500mg qds PO when clinically improving Non-severe: Co-amoxiclav 1.2g tds IV, then to co-amoxiclav 625mg tds PO Severe: (Systemic signs, in limb threatening infection, or otherwise judged severe) Piperacillin-tazobactam 4.5g If exposure to fresh water at site of skin break: Add Ciprofloxacin 750mg bd PO Penicillin allergic: Clindamycin 450mg qds PO Non-severe / penicillin allergic: Clindamycin 450mg qds PO PLUS Ciprofloxacin 500mg bd PO (avoid ciprofloxacin if MRSA carrier – seek advice from Microbiology) Review for suitability for outpatient IV therapy: Ceftriaxone 2g IV once daily Teicoplanin IV if MRSA colonised Draw demarcation line to follow progress Swab wound if broken skin Check for previous MRSA result 7-10 days 7-14 days Add teicoplanin if MRSA colonised Severe / penicillin allergic: 16 tds IV Add teicoplanin if MRSA colonised. Diabetic foot infection osteomyelitis Flucloxacillin 500mg qds PO PLUS Sodium fusidate 500mg tds PO Neck abscess Co-amoxiclav 1.2g IV TDS Necrotising fasciitis / Fournier’s gangrene Piperacillin – tazobactam 4.5g tds IV PLUS Teicoplanin 800mg IV stat then: if < 80kg – 400mg IV od if >80kg - 600mg IV od PLUS Gentamicin 5mg/kg once daily (see gentamicin section, needs drug level checked) PLUS Metronidazole 500mg tds IV or 400mg tds PO Clindamycin 450mg tds PO 6 weeks If no improvement after 4-6 weeks (XRay): Switch to Ciprofloxacin 500mg bd PO to cover pseudomonas. If MRSA infection: Rifampicin 300mg bd PO PLUS Doxycycline 200mg stat, then 100mg once daily PO (if MRSA isolate is susceptible) Clarithromycin 500mg bd IV PLUS Metronidazole 400mg tds PO (500mg tds IV if unable to take PO) If penicillin allergic: Teicoplanin 800mg IV stat then: Suspected if red, swollen, sometimes painful joint or toe in the presence of nearby infected ulcer Underlying bone is usually exposed XRay may be normal in early stages If initial XRay is negative and osteomyelitis is suspected, an MRI should be performed (NICE CG 119: Inpatient management of diabetic foot problems, Feb 2012) 7 days Depends on clinical response Prompt assessment by surgeons is essential re debridement 17 Gentamicin 5mg/kg once daily (see Gentamicin section – needs monitoring of drug levels) if < 80kg – 400mg IV od if >80kg - 600mg IV od PLUS Gentamicin 5mg/kg once daily (see Gentamicin section – needs monitoring of drug levels) PLUS Metronidazole 500mg tds IV or 400mg tds PO Clarithromycin 500mg bd PO 7 days Discuss with ophthalmology Pre-septal cellulitis (around eye) - mild Pinna/Facial Cellulitis (superficial skin / soft tissue) Co-amoxiclav 625mg tds PO Flucloxacillin 1g qds IV PLUS BenzylPenicillin 1.2g qds IV Clarithromycin 500mg bd IV 7 days IV Clarithromycin - risk of phlebitis. Switch to PO as soon as possible Facial cellulitis – odontogenic and other deep soft tissue infections Co-amoxiclav 1.2g tds IV Cefuroxime 1.5g tds IV PLUS Metronidazole 400mg tds PO (500mg tds IV if unable to take PO) 7 days Gentamicin – risks of nephrotoxicity and ototoxicity Gentamicin duration should be kept <5 days wherever possible – review results of cultures and switch antibiotics according to sensitivities If severe type 1 hypersensitivity (anaphylaxis): In renal impairment (eGFR <60ml/min), Gentamicin can be replaced with Ciprofloxacin 400mg bd IV (500mg bd PO if able to take oral medications) Teicoplanin 400mg od IV PLUS Gentamicin 5mg/kg/day plus Metronidazole (as above). Severe pre-septal cellulitis Co-amoxiclav 1.2g IV TDS Cefuroxime 1.5g tds IV PLUS 7 – 10 days Gentamicin – risks of 18 Metronidazole 400mg tds PO (500mg tds IV if unable to take PO) and ALL orbital cellulitis nephrotoxicity and ototoxicity Gentamicin duration should be kept <5 days wherever possible – review results of cultures and switch antibiotics according to sensitivities If severe type 1 hypersensitivity (anaphylaxis): Teicoplanin 400mg od IV PLUS Gentamicin 5mg/kg/day PLUS Metronidazole (as above). SYSTEMIC SEPSIS INDICATION Sepsis – source unclear 1ST LINE Amoxicillin 1g tds IV PLUS Gentamicin 5mg/kg stat (review need for further doses, if continuing drug levels will need to be monitored – see Gentamicin section) Review clinical progress – change antibiotic to regimen as determined by likely source – see relevant sections. ALTERNATIVE If penicillin allergy: Cefuroxime 1.5g tds IV PLUS Gentamicin 5mg/kg stat (review need for further doses, if continuing drug levels will need to be monitored – see Gentamicin section) If severe penicillin allergy (type 1 immediate reaction): Teicoplanin 400mg 12-hourly IV for 3 doses, then 400mg once daily PLUS Ciprofloxacin 400mg bd IV (750mg bd PO if able to take In renal impairment (eGFR <60ml/min), Gentamicin can be replaced with Ciprofloxacin 400mg IV BD (500mg BD PO if able to take oral medications) DURATION 48hrs in the first instance, subsequent antibiotic choice and duration depends on the source of infection – refer to relevant sections of the empirical guidelines. NOTES Definition of sepsis: The systemic inflammatory response syndrome (SIRS) plus clinical evidence of infection. SIRS is defined by 2 or more of: Temp <36°C or >38°C Heart rate >90 beats/min Respiratory rate >20 breaths/min WBC count <4 or >12 x 109/L Initial regimen for sepsis (not severe sepsis) of unknown source, where a chest or urinary infection is thought most likely. Results of recent microbiology samples (e.g. urine and sputum) 19 oral medications) PLUS Gentamcin 5mg/kg stat (review need for further doses, if continuing drug levels will need to be monitored – see Gentamcin section) Severe sepsis Piperacillin-tazobactam 4.5g tds IV PLUS Gentamicin 5mg/kg stat (review need for further doses, if continuing drug levels will need to be monitored – see Gentamicin section) Penicillin allergy (not anaphylactic) or recent ESBL: Meropenem 1g tds IV If MRSA colonised: Add Vancomycin or Teicoplanin (see relevant sections for advice on dosing and monitoring) If severe penicillin allergy: Teicoplanin 800mg IV stat then: if < 80kg – 400mg IV od if >80kg - 600mg IV od PLUS Ciprofloxacin 400mg bd IV (750mg bd PO if able to take oral medications) PLUS Gentamicin 5mg/kg stat (review need for further doses, if continuing drug levels will need to be monitored – se Gentamicin section) must be reviewed if available as this may direct a broader regimen. Antibiotic regimen should be changed to that appropriate to likely source after clinical review. 7-10 days Severe sepsis is sepsis plus evidence of organ dysfunction Definition of sepsis: The systemic inflammatory response syndrome (SIRS) plus clinical evidence of infection. SIRS is defined by 2 or more of: Temp <36°C or >38°C Heart rate >90 beats/min Respiratory rate >20 breaths/min WBC count <4 or >12 x 109/L Organ dysfunction is defined as sepsis plus any of the following: Systolic BP <90mmHg Oliguria (output<0.5ml/kg/hr) Hypoxaemia (SpO2<95% on >60% O2) Altered mental status Lactate >4mmol/L 20 EWS >5 Septic shock is defined as severe sepsis with refractory arterial hypotension or hypoperfusion abnormalities in spite of adequate fluid resuscitation. Neutropenic fever Piperacillin-tazobactam 4.5g qds IV PLUS Gentamicin 5mg/kg once daily (drug levels should be monitored, see Gentamcin section) If penicillin allergic: Teicoplanin 800mg IV stat then: if < 80kg – 400mg IV od if >80kg - 600mg IV od PLUS Ciprofloxacin 750mg bd PO PLUS Gentamicin 5mg/kg once daily IV (drug levels should be monitored, see Gentamcin section) Dependent on clinical response. Definition of neutropenic sepsis: Discuss with Microbiology Three sets of blood cultures must be taken prior to Neutrophil count 0.5 x 109 per litre or lower PLUS, either: temperature >38°C Or other signs and symptoms 2nd line regimen (unresponsive to 1st line): Teicoplanin 800mg IV stat then: if < 80kg – 400mg IV od if >80kg - 600mg IV od PLUS Meropenem 1g tds IV Endocarditis Acute onset, IVDU, MRSA Vancomycin (see vancomycin section for dosing) 21 colonised, or prosthetic valve Endocarditis – Indolent (subacute) presentation and native valve PLUS Gentamicin 1mg/kg bd (see gentamcin section – need drug levels) PLUS Rifampicin 300 - 600mg bd PO if prosthetic valve Amoxicillin 2g 4-hourly IV PLUS Gentamicin 1mg/kg bd IV (see gentamcin section – need drug levels) Line infection – peripheral cannula infection (nonsepsis) Flucloxacillin 500mg qds PO (only if MRSA screen is negative) Line infection - central / tunnelled line sepsis and peripheral cannula infection with sepsis IV Vancomycin (see vancomycin section for dosing) commencing antibiotics Definitive antibiotic therapy is directed by culture and sensitivity – discuss with Microbiologist Penicillin allergic: Vancomycin IV (see vancomycin section for dosing) PLUS Gentamcin 1mg/kg tds IV (see gentamcin section – need drug levels) If penicillin allergic or MRSA positive: Doxycycline 100mg bd PO (most MRSA isolates are doxycycline sensitive, but if not, manage as below) Three sets of blood cultures must be taken prior to commencing antibiotics – at least 6 hours apart where possible. Definitive antibiotic therapy is directed by culture and sensitivity – discuss with Microbiologist 7 days NOT in patients with features of systemic sepsis Consider antibiotic therapy where VIP score 3-4 MRSA screening swab status must be checked 7 days Central / tunnelled lines generally require removal – discuss with Microbiology as appropriate For central / tunnelled line sepsis, collect central and peripheral blood cultures prior to starting antibiotics If associated bacteraemia, follow Microbiology advice for regimen / duration 22 Consider adding a stat dose of gentamicin if risk factors for gram negative infection For peripheral cannula infection – commence if VIP score 5 URINARY TRACT INFECTION INDICATION 1ST LINE Lower UTI Nitrofurantoin 50mg qds PO (avoid if eGFR <40ml/min) OR Trimethoprim 200mg bd PO (avoid if eGFR <30ml/min Complex UTI – Gentamicin 5mg/kg once daily Failure of either 1st line IV for 2 doses then review treatments, recent culture results. urological surgery, structural abnormalities of If eGFR <60mL/min, take urinary tract, oral route trough level 20 hours post 1st unviable dose and await result – only redose when level <1mg/L In moderate/severe renal impairment, consider Temocillin as alternative if not penicillin allergic (see dosing opposite) ALTERNATIVE If resistant to 1st line / renal failure / other contraindication (e.g. pregnant): Cefalexin 500mg bd PO DURATION Female: 3 days Male: 5-7 days If gentamicin resistant ESBL/ampC E.coli or Klebsiella from a recent urine sample: Temocillin 2g bd IV 2 days Gentamicin, followed by 5 days of antibiotic as directed by urine sensitivity If penicillin allergic AND gentamicin resistant ESBL/ampC E.coli or Klebsiella from a recent urine sample: Meropenem 500mg tds IV If not penicillin allergic but with impaired renal function: If eGFR 30-60mL/min: Temocillin 1g bd IV If eGFR 10-30mL/min: Temocillin 1g once daily IV 7 days for Temocillin / Meropenem NOTES Send urine for culture and sensitivity before starting antibiotics -Review results at 48hours, consider IV to oral switch or cessation of antibiotics -De-escalate where possible to narrow spectrum antibiotic -Bacteriuria (or positive dipstick) in the absence of clinical signs and symptoms of UTI does not warrant antibiotic treatment (unless in known risk group) -Catheter related bacteriuria does not require treatment unless clinical evidence of infection -Temocillin is not active vs Pseudomonas & gram positive organisms – use other agents for these 23 If eGFR 10mL/min: Temocillin 500mg once daily IV Pyelonephritis Co-amoxiclav 1.2g tds IV Add gentamicin 5mg/kg stat if severe (review need for further doses, if continuing drug levels will need to be monitored – see Gentamcin section) Followed by: Co-amoxiclav 625mg tds PO Penicillin allergic: Ciprofloxacin 750mg bd PO (400mg bd IV if unable to take oral medications) OR Gentamicin 5mg/kg once daily (see gentamcin section – need drug levels) 7-10 days (if coamoxiclav), 7 days if ciprofloxacin or gentamicin -The following patients are at risk of ESBL/ampC producing E.coli / Klebsiella: >65 yrs of age long term catheter in situ recent urological procedure ESBL/ampC +ve E.coli or Klebsiella in the previous 24 months Pyelonephritis defined as: Renal angle tenderness plus presence of two SIRS criteria: Temp <36°C or >38°C Heart rate >90 beats/min Respiratory rate >20 breaths/min WBC count <4 or >12 x 109/L If eGFR <20mL/min discuss antibiotic choice with Microbiology. 24