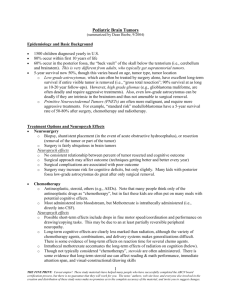
pediatric oncology
advertisement

CHAPTER 8. PEDIATRIC ONCOLOGY BASIC ISSUES IN PEDIATRIC ONCOLOGY Pediatric and adolescent cases represent a small proportion of the worldwide cancer burden. Within Western industrialized nations, the proportion of occurring within the pediatric age range is approximately 2 %. Approximately 10 % of deaths during childhood are related to cancer, making it the most common cause of death from disease (Fig. 8.1). Fig.8.1. Leading causes of death of children between of 1 and 14. (Adapted from US Vital Statistics, 1986) CANCER; 10% congenital anomalies; 8% HIV infection; 1% homicide; 1% suicide; 1% accidents; 44% hart disease; 4% meningitis; 1% pneumonia; 2% cerebral palsy; 1% other; 22% The types and distribution of the malignancies that occur in the pediatric group differ markedly from those that occur in adult populations (Table 8.1). Table 8.1 Distribution of cancer in children younger than 15 years of age by diagnosis (Adapted from Gurney JG, Severson RK, Davis S. Incidence of cancer in children in the US. Cancer, 1995) Acute lynphoblastic leucemia 23.3 % CNS tumors 20.7 % Neuroblastoma 7.3 % Non-Hodgkin's 6.3 % Wilms' tumor 6.1 % Hodgkin's disease 5% Acute myeloid leukemia 4.2 % Rhabdomypsarcoma 3.4 % Retinoblastoma 2.9 % Osteosarcoma 2.6 % Other 2.1 % Etiology and mechanisms of carcinogenesis. Risk factors associated with the development of childhood cancer are principally divided into two categories: endogenous and exogenous. 194 Endogenous factors. It has become increasingly clear that cancer is truly a genetic disease, because overwhelming evidence shows malignancy to be the result of multiple mutations in the DNA of the tumor cell. In contrast to the predominance of somatic mutations, the proportion of pediatric cancer that has a clearly hereditary component is small. Hereditary in this case implies a genetic alteration that has been passed on to the child from a parent or that was a new mutation that occurred in the oocyte or sperm before fertilization. Geneticists categorize disorders by the mechanism of inheritance: constitutional chromosomal abnormality; mendelian autosomal dominant, recessive, or X-linked patterns; and non-mendelian inheritance. The latter category includes inherited disorders that are caused by mutations in multiple genes or mitochondrial DNA or caused by mutations affecting imprinted genes. For any tumor type, the overall inherited fraction is the sum of several different genetic mechanisms. For example, an increased risk of Wilms’ tumor is associated with multiple genetic syndromes, including a chromosomal deletion syndrome, an autosomal dominant disorder, and a syndrome resulting from a disruption of imprinting. Exogenous factors. The main factors are physical, chemical, and biologic agents. The physical agents most commonly studied are ultraviolet radiation, ionizing radiation, and extremely lowfrequency (50-60 Hz) magnetic fields. Some examples of exogenous chemical factors are environmental pollutants, tobacco, aflatoxin, and androgenic steroids. The absolute incidences of cancer as well as the relative frequency of the various pediatric malignancies vary significantly for different age groups. Pediatric cancer is most prevalent in patients between 0 and 4 years of age; approximately 40 % of all malignancies occur during this period. Tumor such as neuroblastoma, Wilms’ tumor, sacrococcygeal teratoma, glioma, hepatoblastoma has their peak frequency in children younger than 5 years of age. This suggests that prenatal factors affecting embryogenesis may be implicated in their pathogenesis. Other tumors such as ovarial teratoma, lymphomad (particularly Hodgkin’s disease), bone sarcoma and most brain tumors do not exhibit frequency peaks in younger children. This possibly reflects the role of postnatal (environmental) factors. Neoplastic transformation of cells in tissue culture and in vivo carcinogenesis are dynamic, multistep and complex processes that can be separated artificially into three phases: initiation, promotion and progression. These phases may be applied to the natural history of virtually all human tumors, including embryonic ones. Initiation is the result of exposure of cells or tissues to an appropriate dose of a carcinogen; an initiated cell is permanently damaged and has a malignant potential. The initiated cells can persist for months or years before becoming malignant. During the promotion phase, initiated cells clonally expand. Promotion may be modulated or reversed by a variety of environmental conditions. In the last phase, progression, the transformed cells develop into a tumor, ultimately with metastasis. Brief overview on metabolic consideration in pediatric cancer. Patients with cancer have associated cachexia with significant weight loss and malnutrition. The reasons for this are obviously multifactorial and may be related directly to the tumor, such as increased metabolic rate, circulating peptides leading to anorexia, and decreased intake resulting from poor appetite or gut involvement. Malnutrition in this patients leads to intolerance of chemotherapyand radiation therapy as well as increased local and systemic infections. Adjunctive nutritional support, either parentarally or enterally, supports the patient during therapy with surgery, chemotherapy, or irradiation. In addition, the use of enteral nutrition protects the gut and is safer and more effective than intravenous nutrition. Nutrients such glutamine and arginine may play a role in protecting the gut and enhancing immune response. Overnutrition may also be harmful because changes in the metabolism of certain nutrients may have immunologic effects. APPROACH TO CHILDHOOD TUMOR DIAGNOSIS Prenatal diagnosis of embryonic tumors The approach for prenatal diagnosis of fetal tumors should be based on three sets of ultrasound signs: general signs, organ-specific signs and tumor-specific signs. The general sonographic features, that should raise the suspicion of an underlying fetal tumor, include: 195 Absence or disruption of contour, shape, location, sonographic texture or size, of a normal anatomic structure; Presence of an abnormal structure or abnormal biometry; Abnormality in fetal movement; Polyhydramnios; Hydrops fetalis. Polyhydramnios is particularly important, because almost 50% of fetal tumors are accompanied by this finding. The underlying mechanisms include interference with swallowing (such as thyroid goiter or myoblastoma), mechanical obstruction (such as gastrointestinal tumors), excessive production of amniotic fluid (such as sacrococcygeal teratoma), and decreased resorption by lung tissue in lung pathology. Intracranial tumors are also commonly associated with polyhydramnios and the mechanism may be neurogenic lack of swallowing or inappropriate polyuria. Tumor-specific signs include pathological changes within the tumor mass (calcifications, liquefaction, organ edema, internal bleeding, neovascularization and rapid changes in size and texture). Organ-specific signs are rare, but in some cases they are highly suggestive of the condition (such as cardiomegaly with a huge solid or cystic mass occupying the entire heart, suggesting intrapericardial teratoma). In some cases, normal and abnormal sonographic findings may mimic fetal tumors. Examples may vary from severe cases of bladder exstrophy (where the protruding bladder mass appears as a solid tumor-like structure), to rare cases of fetal scrotal inguinal hernia (where bowel loops occupy the scrotum, appearing as huge masses). Signs and symptoms in the child with cancer. It is often difficult to diagnose childhood cancer in its early stages because the signs and symptoms are relatively nonspecific and may mimic a variety of other, more common childhood disorders. Obtaining the history is the first step in the diagnostic process, with the chief complaint being the most important initial clue. Although any persistent changes in a child’s health status should be brought to the attention of a physician, there are certain chief complaints that should increase the index of suspition for cancer in a child (table 8.2). Table 8.2. Common chief complaints given by parents that suggest a pediatric cancer Chief complaints Suggested cancer Chronic drainage from ear Rhabdomyosarcoma: Langerrhans cell histiocytosis Morning headache with vomiting Brain tumor Lump in neck that that does not respond to Hodgkin’s or non- Hodgkin’s lymphomas antibiotics Swollen face and neck Non- Hodgkin’s lymphoma, leukemia Mass in abdomen Wilm’s tumor, neuroblastoma, hepatoma Bleeding from vagina Yolk sack tumor, rhabdomyosarcoma Weight loss Hodgkin’s lymphoma Bone pain Leukemia, neuroblastoma Usually the signs and symptoms of childhood cancer are caused by a mass and its disturbance of surrounding normal structures. Less frequently, substances released by the tumor alter normal function. The family medical history may be of paramount importance when the diagnosis of malignancy is a possibility. Detailed history of the parents, siblings, and first cousins should be noted on a family group record. When dealing with pediatric tumors, genetic factors may be important. Established associations with genetic traits and others neoplasm are summarized elsewhere. The major categories of disease linked with an increased risk of cancer are immunodeficiency disorders, metabolic disorders, disorders of chromosomal instability. Certain familial and genetic diseases such as autoimmune diseases, neurofibromatosis, and Down syndrome should be documented. Noninvasive imaging techniques: 196 Plain film chest radiography is the examination of choice for short-term interval evaluation of pulmonary metastases and complications of therapy such as drug reaction and pulmonary infections. The examination is fast, technologically easy, relatively inexpensive, requires no anesthesia or sedation. Plain films of the abdomen are the best simple evaluation of the abdominal mass, abdominal gas pattern and of the presence or absence of intestinal obstruction or free intraperitoneal air. Barium studies are a simple and sensitive means of evaluating gastrointestinal tract lesions. Diagnostic ultrasound (US) examination, particularly when performed with the newest computerized equipment, is an excellent tool in the evaluation of the abdomen, pelvis, and scrotal contents of children. Its utility in examining other areas of the body depends on the amount of bone or gas present in or near the structure to be imaged. Because ultrasound examinations are relatively quick, inexpensive, use no ionizing radiation, have no known complications or side effects, and do not require sedation or anesthesia, they represent the ideal screening examination for the abdomen, retroperitoneum and pelvic organs. US can easily and quickly differentiate solid from fluid-filled masses and usually can distinguish the organ of origin of an abdominal mass. Computed tomography (CT) image represents of a thin section of anatomy. The increasing technological sophistication of CT has permitted excellent images of the thorax, abdomen, extremities, cranium, and spine and its contents. Intravenous contrast material is often useful in the thorax to differentiate vascular from nonvascular structures; in the abdomen to better define hepatic, splenic, renal, and adrenal masses; and to differentiate retropritoneal and mediastinal vessels from masses. Appropriate use of oral contrast material is necessary to differentiate intestinal loops from intra-abdominal masses. CT is the modality of choice for identifying most solid tumors. Its major disadvantages for pediatric cancer patients are its cost, ionizing radiation, and the need for conscious sedation or general anesthesia in the young patient. Nevertheless, these disadvantages are slight when compared with the information to be gleaned from these studies. The role of magnetic resonance imaging (MRI) in the evaluation of pediatric oncologic disease has expended at a rapid pace over the last 10 years. Clinical MR is based on “alignment” of the body’s hydrogen nuclei in a strong, uniform magnetic field. MR images represent “slices” through the body that are made up of a specific number of volume elements, called voxels. Using a mathematical process, each voxel is assigned a shade of grey between white and black. The intensity of this shade of gray depends on the amount of energy detected by the receivig coil for each voxel. MRI offers several advantages over CT. In addition to the lack of ionizing radiation, tissue contrast between bone, tumor, muscle, and fat is enhanced on MR. Iodinated contrast agents are not required. Tumor markers. Significant advances have been made in identifying cellular and extracellular tumor markers. Although some of these cellular markers, such as alpha-fetoprotein, have direct clinical usage, many have no direct clinical application. They potentially provide important clues to the presence of a cancer, but even with these advances, the only absolute way to establish the diagnosis of cancer is by pathologic confirmation. Excisional and incisional biopsies are the standard techniques for obtaining diagnostic tissue. An excisional biopsy is preferred by most pathologists, because it yields a greater amount of tissue with fewer artifactual distortions than the smaller incisional biopsy. However, if an excisional biopsy could compromise future therapy in some fashion, it should not be perfomed. Regardless of the particular biopsy technique, the resultant tissue should be placed in 0.9 % saline and immediately transported to the surgical pathology laboratory. Light microscopy, electron microscopy, immunohistochemistry, immunophenotyping of suspected lymphomas, cytogenetic DNA analysis through flow cytometry, and oncogene amplification studies are specialized diagnostic procedures available in many laboratories. GENERAL PRINCIPLES OF SURGERY IN PEDIATRIC ONCOLOGY Routine preoperative evaluation is necessary to exclude congenital or familial problems such as bleeding disorders or malignant hyperthermia. Anemias and coagulation defects are frequent in this population. 197 Many patients may have had treatment with chemotherapy or irradiation before surgery and may have resulting cardiopulmonary abnormalities. Some chemotherapeutic agents may adversely affect coagulation status or platelets. Perhaps the most accurate indicator of adequate coagulation is a normal bleeding time. Because many of these children are immunosuppressed from their disease or from therapy, associated infections or wound healing problems should be investigated. Special techniques may by considered when surgeons operate on small children with large tumors. Certain considerations to minimize intraoperative blood loss and the need for massive transfusion in small children with relatively limited blood volume may be helpful. Acute euvolemic hemodilution was first used in patients undergoing cardiopulmonary bypass and is currently used for many types of surgical procedures when significant blood loss is anticipated. Preoperative radiologic tumor embolization or intraoperative arterial embolization allows resection with less blood loss. Other techniques for minimizing blood loss include ultrasonic aspiration, argon laser beam, cryotherapy, and total hepatic vascular occlusion in liver resection. COMMON PEDIATRIC SOLID TUMORS MALIGNANT LYMPHOMAS Lymphomas are malignant neoplasms of the lymphoid system. Broadly classified as either Hodgkin disease or as non-Hodgkin lymphoma (NHL), these entities are clinically, pathologically, and biologically distinct. MALIGNANT NON-HODGKIN’S LYMPHOMAS (NHL) Most childhood NHL can be classified according to the National Cancer Institute (NCI) formulation as either lymphoblastic, small noncleaved cell (Burkitt or Burkittlike), or large cell lymphomas (LCLs). Burkitt lymphoma (BL) is significantly more common in sub-Saharan Africa, where it accounts for approximately one half of childhood cancers. Pathophysiology. Most malignancies arise as localized disease within the organ or tissue of origin then may secondarily spread via local extension or distant metastases. In contrast, NHL is best regarded as a systemic disease due to the unique anatomy of the lymphoid system and physiology of lymphoid cells, which tend to migrate whether they are normal or malignant. Childhood NHL generally presents as bulky extramedullary (usually extranodal) disease with or without demonstrable dissemination. The distinction between NHL and acute leukemia is arbitrary; thinking in terms of a spectrum from clinically localized disease to overt leukemia is best. Most treatment protocols now define acute leukemia on the basis of marrow involvement greater than some threshold (typically, a blast count >25%), irrespective of the presence of bulky extramedullary disease. In contrast, a tumor accompanied by marrow involvement less than this threshold constitutes stage 4 lymphoma. Causes. In developed countries, most individuals with NHL have no known etiology or association. Several epidemiologic studies suggest a role for pesticide exposure in the development of adult NHL; the case for childhood NHL is less compelling but still under investigation. Immunosuppressed individuals (eg, HIV positive, post–bone marrow transplant) are at higher risk of developing NHL, particularly SNCCL and LCL of B-cell origin. Epstein-Barr virus, which causes B-cell proliferation and in vitro immortalization, has been implicated in most of these lymphomas. Primary CNS lymphoma is more common in these patients. Patients successfully treated for Hodgkin disease are at increased risk of developing NHL. This appears to reflect the combined effects of chemotherapy, radiotherapy, and the immunosuppressive effects of Hodgkin disease. Among pediatric cancer survivors, secondary NHL is less common than in adults. In sub-Saharan Africa, a strong association exists between the development of endemic BL and prior exposure to both malaria (with resultant T-cell suppression) and Epstein-Barr virus. 198 The genetic basis of pediatric NHL has been studied extensively. Each subtype of NHL is characterized by 1 or more molecular lesions that contribute to the malignant phenotype. Many of these are chromosomal translocations involving genes for immunoglobulin (Ig) or T-cell receptor molecules. During normal lymphocyte development, these loci undergo recombination that serves to enhance immunologic diversification. Mistargeted recombination leads to translocations with other genes (typically, those that function to regulate cell growth). The resulting dysregulation of these latter genes contributes to the transformed phenotype. Frequency. Collectively, lymphomas are the third most common childhood malignancy after acute leukemias and brain tumors. Lymphomas constitute 10-12% of childhood cancers. older adolescents, lymphomas surpass brain tumors in incidence, largely due to the increased frequency of Hodgkin disease in this age group. In children, NHL is somewhat less common than Hodgkin disease. However, the incidence of NHL appears to be rising. This trend largely reflects the occurrence of NHL in patients who are immunocompromised (eg, HIV positive) and in patients previously exposed to chemotherapy and radiation as treatment for an unrelated cancer. Clinical manifestations. Presentation is acute or subacute, in contrast to the indolent course that characterizes most adult lymphomas. Duration of symptoms prior to diagnosis is generally 1 month or less. Specific complaints vary and depend upon the predominant site(s) of involvement. Constitutional symptoms are uncommon, except in patients with anaplastic LCL, many of whom exhibit low-grade fever, malaise, anorexia, or weight loss. LCLs are biologically disparate. Accordingly, LCLs have a more varied presentation that may include chest or abdominal complications. Dyspnea or stridor may be present with a mediastinal mass. With superior vena cava syndrome, distended neck veins and plethora also may be observed. Decreased breath sounds are heard secondary to bronchial obstruction or pleural effusion. Thoracic dullness to percussion may be present with pleural effusion. Abdominal tumors (usually SNCCL or B-cell LCL) present with abdominal pain, constipation, mass, or ascites. Abdominal distension or mass may be present with or without tenderness, rebound tenderness, and/or shifting dullness. Non-Hodgkin's lymphoma sometimes presents with acute or subacute abdominal disease such as true or simulated appendicitis, intestinal obstruction, or perforations. Intussusception occurring in children above the age of 2 years should raise the suspicion of a primary pathology, such as Meckel's diverticulum or lymphoma. Bone marrow involvement may cause generalized or migratory bone pain; however, in individuals with NHL, significant cytopenias are uncommon, and their presence suggests a diagnosis of acute leukemia. Localized disease can present as lymphadenopathy (usually firm and nontender), tonsillar hypertrophy, or a mass in virtually any location. However, NHL is primarily an extranodal disease in children. Patients with supradiaphragmatic disease (eg, lymphoblastic lymphoma) often complain of nonproductive cough, dyspnea, chest pain, and dysphagia. Anaplastic LCL (ie, Ki-1+ lymphoma) sometimes presents with painful skin lesions (which may regress spontaneously), bone lesions, peripheral lymphadenopathy, and hepatosplenomegaly. Less commonly, testicular, lung, or muscle involvement is observed. Anaplastic LCL may also exhibit an apparent "cytokine storm," with fevers, vascular leak, and altered blood counts (anemia, thrombocytopenia, leukopenia, leukocytosis). Patients occasionally develop symptomatic CNS involvement prior to diagnosis. Headache, meningismus, cranial nerve palsies, and altered sensorium may be observed. Although CNS involvement at diagnosis is uncommon, patients with NHL (particularly SNCCL) occasionally present with symptoms suggestive of meningoencephalitis. Complications. Rapidly growing or bulky tumors can cause severe metabolic derangement, which may be life threatening. 199 The initiation of effective chemotherapy acutely increases the risk of complications including hyperkalemia, hyperphosphatemia, hypocalcemia, oliguria, and renal failure. Other immediate risks depend on the site and extent of involvement. These risks vary according to the histologic subtype of disease. Individuals with lymphoblastic lymphoma often present with mediastinal involvement, which may be massive and life threatening. Airway compression is a particular concern and must be considered in any patient with neck or chest disease. Even in the absence of symptomatic airway compromise, the risk of sudden obstruction may exist if a patient undergoes anesthesia for biopsy or central line placement. In these individuals, possibly consider biopsy under local anesthesia or immediate radiation therapy to the airway, provided that another site of disease is outside the radiation field (to allow subsequent histologic confirmation of the diagnosis). Mediastinal tumors also may cause great vessel compression (superior vena cava syndrome) with swelling of the neck, face, and upper extremities. Esophageal compression may cause dysphagia. Pleural effusions sometimes are observed and may be large enough to cause symptoms. In these individuals, thoracentesis may be both therapeutic and diagnostic, thereby obviating biopsies. Most patients with small noncleaved cell lymphomas (SNCCLs) present with abdominal involvement, typically in the ileocecal area and arising from Peyer patches. A potential complication at diagnosis is bowel obstruction due to direct compression, torsion, or intussusception. Because of bowel perforation, some patients exhibit ascites or the clinical picture of acute appendicitis or peritonitis. In equatorial Africa, SNCCL (ie, endemic BL) classically presents as a mass in the jaw, nasopharynx, or orbit. These masses grow rapidly and can be quite disfiguring. Treatment. All children with non-Hodgkin’s lymphoma should be considered for entry into a clinical trial. Treatment planning by a team of pediatric oncologists at as institution with experience in treating pediatric malignancies is strongly recommended to determine, coordinate, and implement optimum treatment. Although the extent of disease may govern to some degree the choice of treatment protocol, the primary therapeutic modality for all histologies and stages of childhood non-Hodgkin’s lymphoma is chemotherapy. This is based on the belief that non-Hodgkin’s lymphomas are generalized diseases and on empirical clinical experience. Children with limited disease have a markedly betted prognosis when treated with chemotherapy than with irradiation alone, and there is good evidence that irradiation adds no therapeutic benefit in this situation but does increase shortterm and long-term toxic effects. In patients with extensive disease, radiotherapy can at best serve only an ancillary role. It has been used as emergency treatment for involvement of the nervous system and sometimes for testicular involvement or for superior vena caval obstruction. Surge may benefit certain patients with small noncleaved cell lymphomas and probably those with large cell lymphomas. Patients in whom tumor can be completely resected before chemotherapy have an excellent prognosis, significantly better than that for patients with unresectable abdominal disease. The role of surgery, however, requires reevaluation in light of recent improvements in prognosis. For this group of patients, it should be restricted to three situations: biopsy for initial diagnosis, laparotomy in patients who present with abdominal emergency, such as intussusception, intestinal perforation, suspected appendicitis, or serious gastrointestinal bleeding; and second look surgery. Surgical resection has immediate benefits for treating emergency situations that go beyond its role in specific therapy. In many such patients, complete resection is performed as part of dealing with the abdominal emergency, and if complete resection without major organ compromise can be performed, it is appropriate to do so. In the absence of a surgical emergency, it is appropriate to attempt complete resection only if modern chemotherapy cannot be given. There is no indication for partial reduction of tumor bulk by surgery. Second-look surgery in patients who still have a residual mass on completion of chemotherapy has sometimes been recommended, although surgical resection in this group of patients does not appear to be advantageous. Patients in whom the residual mass contained no viable tumor had an excellent prognosis, and it was most unlikely that surgery was a contributing factor to this outcome. Patients in whom residual tumor was documented had a poor prognosis despite local therapy. 200 Prognosis. The treatment of non-Hodgkin’s lymphomas in children has improved greatly in the last 15 years. Between 70 % and 90 % of patients with extensive disease can be expected to be cured. HODGKIN DISEASE Hodgkin’s disease (HD) is a malignant disorder of the lymph node that is highly curable with combined modality therapy. The original paper of Hodgkin in 1832 was entitled: “On some morbid appearances of the absorbent glands and spleen”. In that era of anatomic description of disease, investigators were concerned with differentiating inflammatory disease from infection or idiopathic hypertrophy of the lymphoid organs. Following its first description in 1832 and before the malignant nature was elucidated, it was considered an infectious or inflammatory condition. Sternberg in 1898 and Reed in 1902 are generally credited with the first definitive and thorough description of the histopathology of Hodgkin’s disease. Causes. As with most malignancies, the following factors may contribute to development of HD: Genetic predisposition Environmental factors (eg, infectious agents); Immune dysregulation Pathophysiology. HD is a disease of the reticuloendothelial and lymphatic systems. As with other malignant disease, invasion of other organ systems can occur. Clustering of cases within families or racial groups has supported the idea of a genetic predisposition or common environmental link. Several epidemiologic studies have suggested links between HD and certain viral illnesses. The strongest case to date relates to Epstein-Barr virus (EBV), where viral DNA has been noted in Reed-Sternberg cells. The possible role of human herpes virus 6 (HHV6) is also under investigation. While the connection between these infectious agents and HD is intriguing, further study is necessary to define the role these agents might play in the pathogenesis of this malignancy. Morphology. The Reed-Sternberg (RS) cell, which in most cases is a B cell, is the malignant cell in HD. Classically, the RS cell is a large multinucleated cell with abundant cytoplasm. A characteristic clearing is present around the nucleolus, and cells with 2 large nuclei can produce an owl's eyes appearance. The inflammatory background contains lymphocytes, histiocytes, plasma cells, eosinophils, and neutrophils. The morphology of both the RS cell and the inflammatory background vary with histologic subtype. Currently most common, The Rye classification system defines four histologic subtypes of Hodgkin’s disease: lymphocytic predominance (LP), mixed cellularity (MC), Lymphocyte-depleted (LD), and Nodular sclerosis (NS). Age. Hodgkin's disease in children has a peak incidence at 11 to 15 years of age. Staging. Once tissue diagnosis is made, the disease is staged using imaging studies, bone marrow evaluation, and the presence or absence of B symptoms. Staging laparotomy has no role in pediatric HD. The most widely used staging system is the Ann Arbor staging system. Stage I. Involvement of a single lymph node region or of a single extralymphatic organ or site Stage II. Involvement of 2 or more lymph node regions on the same side of the diaphragm or localized involvement of an extralymphatic organ or site and 1 or more lymph node regions on the same side of the diaphragm Stage III. Involvement of lymph node regions on both sides of the diaphragm, which may be accompanied by localized involvement of an extralymphatic organ, or site, or both Stage IV. Diffuse or disseminated involvement of 1 or more extralymphatic organs or tissues with or without associated lymph node involvement Clinical manifestations. The most common presenting symptom for HD is asymptomatic cervical or supraclavicular lymphadenopathy. Two thirds of these patients have mediastinal involvement as well. Constitutional (B symptoms, see below) are observed in 20-30% of patients with this malignancy. 201 Localized symptoms: painless adenopathy, which is usually nontender, is present. Respiratory symptoms: cough or chest pain, stridor or decreased breath sounds on auscultation may be present as a result of mediastinal involvement. Superior vena cava syndrome due to impeded blood return secondary to a mediastinal mass can be observed. Splenomegaly may be observed with abdominal involvement. Isolated disease in the abdomen is unusual. Systemic symptoms: B symptoms result in the upgrading of stage, which is denoted by the suffix B appearing after the numeric stage (eg, stage IIB). Patients without any of these symptoms have the suffix A added after the numeric stage (eg, IIIA). This designation is important because the presence or absence of the following B symptoms has bearing on the prognosis: Unexplained fever with temperature above 38°C for 3 consecutive days Unexplained weight loss of 10% or more within the previous 6 months Drenching night sweats Other systemic symptoms include pruritus, urticaria, and fatigue. Lab studies: Hemoglobin/hematocrit: anemia can be observed in the absence of bone marrow disease, usually because of a destructive process (ie, hemolytic anemia, which may be Coombs positive). Anemia of chronic disease can also be observed depending on duration of disease prior to diagnosis. Platelet count: thrombocytopenia and an idiopathic thrombocytopenia purpura (ITP)– type picture may be present. White blood cell count/differential: abnormalities such as lymphopenia, eosinophilia, and monocytosis may be present. Erythrocyte sedimentation rate (ESR) is usually elevated. Imaging studies: A chest radiograph (CXR) with anteroposterior and lateral projections often shows a mediastinal mass. A mass that occupies more than one third of the intrathoracic diameter carries a poorer prognosis than a smaller mass. CT imaging: Scan the head to include Waldeyer ring, neck, chest, abdomen, and pelvis for sites of disease. Bone scan Lymphangiogram (when CT imaging is not available) Procedures: Bone marrow aspirate and biopsy Tissue biopsy Treatment. Treat children with HD at a pediatric oncology center where pediatric oncologists, radiation therapists, and full ancillary services for children with malignancies are available. Medical Care. In pediatric patients, treatment consists of multiagent chemotherapy and possible radiation therapy. The specifics of both of these regimens vary with the stage of disease. With chemotherapy used in conjunction with radiation therapy, patients with early stage HD have long-term survival rates of close to 100%. Patients with more advanced disease, especially those with B symptoms, have survival rates of greater than 80%. Many different combinations of chemotherapy are used. In general, advanced-stage disease requires more cycles of chemotherapy than localized disease. Recent protocols have focused on decreasing the long-term toxicity of therapy. This has been accomplished by alternating courses of active multichemotherapies, as well as substitution of newer less toxic agents for some members of the traditional MOPP regimen (mechlorethamine, vincristine, procarbazine, prednisone). Involved-field and extended-field radiation is used depending on the extent of disease. Because of the effects of radiation therapy on musculoskeletal growth in children as well as the increased risk of second malignancies in the radiation field (such as breast cancer in adult survivors of HD who were treated with mantle radiation), low-dose radiation is used in conjunction with chemotherapy. 202 Surgical care. A staging laparotomy and splenectomy is currently not routinely performed in patients with HD. In patients with suspicious lesions on imaging performed for staging, biopsy is sometimes necessary if the findings may alter the treatment regimen. Complications. Most complications are due to recurrence of disease or adverse effects of treatment. Prognosis. The overall 5-year survival rate for HD is 91%. Patients with localized disease have a higher rate (>90%) than those with advanced-stage disease (as low as 70%). WILMS’ TUMOR (NEPHROBLASTOMA) Wilms’ tumor or nephroblastoma is the most common childhood abdominal malignancy. In the past 3 decades, the multidisciplinary approach to this tumor has become an example for successful cancer treatment. Currently, survival rates of children affected with this neoplasm approximate 80-90%. Understanding of the molecular mechanisms that contribute to the development of Wilms’ tumor has greatly expanded over the past years, making Wilms’ tumorigenesis a model for the understanding of the development of other tumors. Causes. Wilms’ tumor is thought to be caused by alterations of genes responsible for normal genitourinary development. Examples of common congenital anomalies associated with Wilms’ tumor are cryptorchidism, double collecting system, horseshoe kidney, and hypospadias. Environmental exposures, although considered, seem less likely to play a role. Pathophysiology. The first Wilms’ tumor suppressor gene at chromosome arm 11p13, was identified as a direct result of the study of children with Wilms’ tumor that also had aniridia, genitourinary anomalies, and mental retardation (WAGR syndrome). Karyotypic analysis of these children revealed constitutional deletions within the short arm of one copy of chromosome 11. Subsequently, the 11p13 locus was demonstrated to encompass a number of contiguous genes, including the aniridia gene PAX6 and the Wilms’ tumor suppressor gene WT1, which was cloned in 1990. WT1 encodes a transcription factor critical to normal kidney and gonadal development. The characterization of this novel tumor suppressor gene has provided insight into the mechanisms underlying normal kidney development and Wilms’ tumorigenesis. The WT1 gene has now been shown to be the specific target of mutations and deletion events in a subset of sporadic Wilms’ tumors, as well as in the germline of some children with genetic predisposition to this cancer. A second Wilms’ tumor predisposing gene has been identified (but is not yet cloned) telomeric of WT1, at 11p15. This locus has been proposed based on studies of patients with both Wilms’ tumor and Beckwith-Wiedemann syndrome (BWS), another congenital Wilms’ tumor predisposition syndrome linked to chromosome arm 11p15. BWS is an overgrowth syndrome characterized by visceromegaly, macroglossia, and hyperinsulinemic hypoglycemia. In addition, patients with BWS are predisposed to several embryonal neoplasms including Wilms’ tumor. Thus far, a few candidate loci for Wilms’ tumor and BWS have been proposed. These include the insulinlike growth factor II gene (IGFII), H19 (an untranslated RNA) and p57kip2. Frequency. Wilms’ tumor affects approximately 10 children per one million before the age of 15 years. In 5-10% of cases, both kidneys are affected either at the same time (synchronous bilateral Wilms’ tumor) or one after the other (metachronous bilateral Wilms’ tumor). Age. The median age at diagnosis is approximately 3.5 years. The median age is highest for unilateral unicentric cases (36.1 mo) and lowest for synchronous bilateral Wilms’ tumor (25.5 mo). Sex. Among patients with unilateral Wilms’ tumor, the male-to-female ratio was 0.92:1.00. For patients with bilateral disease, the male-to-female ratio was 0.60:1.00. Race. Wilms’ tumor is relatively more common in blacks than in whites and is less common in East Asians. Clinical History. The most common presentation is an asymptomatic abdominal mass discovered by the parent or physician. Occasionally the child presents with haematuria, but symptoms are often non203 specific: abdominal fullness, abdominal pain, gastrointestinal upset, fever, weight loss, malaise, and anaemia. Hypertension is sometimes detectable. A small number of patients who have hemorrhaged into their tumor may present with signs of hypotension, anemia, and fever. Rarely, patients with advanced-stage disease may present with respiratory symptoms related to the presence of lung metastases. Physical. Examination often reveals a palpable abdominal mass. Pay special attention to features of those syndromes (WAGR and BWS) associated with Wilms’ tumor, ie, aniridia, genitourinary malformations, and signs of overgrowth. Rarely, a left varicocele arises as a result of tumor occlusion of the left renal vein. Examination of the abdominal mass should be performed carefully. Concern has been raised that palpating a mass too vigorously could lead to rupture of a large tumor into the peritoneal cavity. Lab Studies Complete blood cell count Chemistry profile including kidney function tests and routine electrolytes with calcium Urinalysis Coagulation studies Cytogenetics studies An 11p13 deletion as in the WAGR syndrome (Wilms’, aniridia, genitourinary abnormalities, mental retardation) A duplication of the paternal allele 11p15 as in BWS Mutational analysis of the WT1 gene in cases where Denys-Drash syndrome (intersexual disorders, nephropathy, Wilms’ tumor) is suspected Imaging Studies Renal ultrasonography (with dynamic imaging of the renal vein and interior vena cava). CT scanning. Abdominal CT scanning helps determine the tumor's origin, lymph node involvement, bilateral kidney involvement, and invasion into major vessels (eg, inferior vena cava or liver metastases). If findings on chest CT scanning are positive while chest radiographic findings are negative, diagnostic biopsy of the lesions noted on the chest CT scan is recommended. Chest radiography (4-field) - Detects lung metastases (Patients with lung lesions on chest radiography receive whole lung radiotherapy.) Procedures Histopathologic confirmation of disease is essential. Consequently, in North America, patients with suspected Wilms’ tumor undergo nephrectomy immediately. During this procedure, the contralateral kidney is explored to ensure that the disease is indeed unilateral, and lymph node biopsies are obtained for staging purposes. Lymph node dissection is not indicated. In contrast to immediate surgery, most European centers make a presumptive diagnosis of Wilms’ tumor based on findings on imaging studies alone. The SIOP centers prefer to administer prenephrectomy chemotherapy. In North America, immediate nephrectomy is not performed in bilateral disease at presentation, when sparing of renal tissue becomes important. Transcutaneous biopsy is not indicated and may in fact complicate treatment. Patients with negative findings on chest radiography and positive findings on CT scanning of the lungs require tissue diagnosis of the lung nodule(s) because several conditions such as histoplasmosis, atelectasis, pseudotumor, intrapulmonary lymph node, and pneumonia can mimic pulmonary metastases. Histologic Findings. The classic histologic pattern is composed of epithelial, blastemal, and stromal elements (triphasic). Approximately 90% of all renal tumors have the so-called favorable histology (FH). Three to 7% of Wilms’ tumors are characterized by anaplastic changes, a feature that, if present diffusely throughout the tumor, predicts for poor outcome. Wilms’ tumors with anaplastic changes are called unfavorable histology Wilms’ tumors. Finally, 2 tumor types previously included in the unfavorable histology Wilms’ tumor category are in fact clearly separate malignant entities. This includes clear cell sarcoma of the kidney (CCSK) and rhabdoid tumor of the kidney (RTK). Medical Care. The usual approach in most patients is nephrectomy followed by chemotherapy with or without postoperative radiotherapy. Table 1 summarizes the current approach 204 to patients with Wilms’ tumor according to the fifth National Wilms’ Tumor Study Group (NWTSG) study report (NWTS-5). Table 8.3. Current approach to Wilms’ tumor by stage and histology Stage, Histology Surgery Chemotherapy Radiotherapy* Stage I or II with FH Vincristine Nephrectomy Stage I with anaplasia Dactinomycin None Stage III or IV with FH Vincristine Stage II, III, or IV with Nephrectomy Dactinomycin focal anaplasia Doxorubicin Yes Vincristine Stage II, III, or IV with Doxorubicin diffuse anaplasia Nephrectomy Yes Cyclophosphamide Stage I, II, III, or IV CCSK Etoposide Cyclophosphamide Stage I, II, III, or IV RTK Nephrectomy Etoposide Yes Carboplatin *Current radiotherapy dosage is approximately 1080 cGy for the abdomen and 1200 cGy for the lung. Only patients with stage IV with lung metastases receive whole lung radiotherapy. Further Inpatient Care. No precautions on activity are advised, although the patient and parents should be aware that after therapy the patient only has one kidney. Activities such as boxing and hockey that carry an inherent risk of kidney injury should be avoided. Up to a third of patients with Wilms’ tumor can present with hypertension. The blood pressure usually normalizes after nephrectomy but occasionally requires longer therapeutic intervention. Five to 10% of patients present at diagnosis with acquired von Willebrand disease. If present, excessive bleeding during surgery should be expected and prenephrectomy therapy instituted. Whenever possible, the use of blood derivatives should be avoided because of the potential for transmission of viral infections. Instead, an initial trial of desmopressin (DDAVP), a drug that promotes the release of vWF from storage sites and has been shown effective in most patients with type I von Willebrand disease and in some type II cases, is recommended. If administered, fluid and electrolyte balance should be monitored carefully. If DDAVP is ineffective, cryoprecipitate or a specific vWF concentrate should be administered. Further Outpatient Care. The patient must be seen at the follow-up clinic after completing all therapy. The purpose of follow-up care is to check for recurrence and also late effects of therapy. Table 8.4 outlines the types and frequency of radiographic studies during the follow-up period according to the NWTSG. Table 8.4. Imaging Studies Recommended for follow-up of children with Wilms’ tumor free of metastasis at diagnosis* Wilms’ tumor type Imaging studies Off-treatment schedule FH (stages I, II, and III) Anaplastic histology (stages I, II, and III) After 6 weeks and 3 months postoperatively; then every 3 Chest radiography months (5 times), then every 6 months (3 times), then yearly (2 times) Patients aged <48 Abdominal months at diagnosis ultrasonography with nephrogenic rests Every 3 months for 6 years 205 (all stages) Patients aged >48 months at diagnosis Abdominal with nephrogenic rests ultrasonography (all stages) FH (stage I and II) FH (stage III) Every 3 months for 4 years Abdominal ultrasonography Yearly (6 times) Abdominal ultrasonography After 6 weeks and 3 months postoperatively; then every 3 months (5 times), then every 6 months (3 times), then yearly (2 times) Unfavorable histology Abdominal Every 3 months (4 times), then (all stages) ultrasonography every 6 months (4 times) *Subsequent imaging studies should be performed as clinically indicated. Complications. The primary treatment, nephrectomy, may damage kidney function. However, additional treatment modalities may cause damage to several organs such as the heart, lungs, liver, bones, and gonads. In addition, both chemotherapeutic agents and radiation therapy can induce second malignant neoplasms. Renal function. Children with Wilms’ tumor are at risk for impaired renal function primarily related to the nephrectomy performed as part of treatment. In selected patients, ie, those who receive radiation therapy, the function of the remaining kidney can be further endangered. The development of compensatory postnephrectomy hypertrophy of the remaining kidney has been well documented in patients with Wilms’ tumor. NWTSG data suggest that most patients with unilateral Wilms’ tumor do not develop serious long-term renal complications. By contrast, renal function can be impaired for those with bilateral disease. The most common cause for renal failure in patients with bilateral Wilms’ tumor is bilateral nephrectomy. Treatment-related injury (eg, radiation-induced damage, surgical complications) of the remaining kidney is the second leading cause of renal insufficiency. Cardiac function. Congestive heart failure is a well-known complication following the administration of anthracyclines. Therefore, patients with Wilms’ tumor who receive anthracyclines, most commonly doxorubicin, should be monitored for cardiac dysfunction. Pulmonary function. Because radiation therapy can affect pulmonary function, patients with Wilms’ tumor metastatic to the lung who are treated with bilateral pulmonary irradiation require pulmonary function monitoring. The total lung capacity (TLC) and vital capacity (VC) of patients receiving bilateral irradiation can be expected to decrease by 50-70% of predicted. Hepatic function. The liver of patients treated for Wilms’ tumor may be damaged by several cytotoxic agents, including dactinomycin, and irradiation. Some patients with Wilms’ tumor have been reported to develop hepatic veno-occlusive disease (VOD). This is primarily a clinical diagnosis characterized by hepatomegaly or right upper quadrant pain, jaundice, ascites, and unexplained weight gain. The syndrome occurs both in patients with Wilms’ tumor undergoing upfront nephrectomy as well as in those receiving combination chemotherapy prior to surgery. Using the currently accepted radiotherapy techniques, radiation-induced hepatitis is rare in survivors of Wilms’ tumor. Gonadal function. Women who received whole abdominal irradiation in childhood can develop ovarian failure. Male patients are at risk for testicular failure after the administration of radiation therapy (whole abdomen) or certain chemotherapeutic agents, most notably alkylating agents. Prognosis. Approximately 80-90% of diagnosed children survive with current multimodality therapy. Patients with FH tumors have at least an 80% overall survival rate at 4 years after initial diagnosis, even in patients with stage IV disease. 206 Synchronous bilateral cases have a 70-80% survival rate, while those with metachronous tumors have a 45-50% survival rate. The prognosis for patients who relapse is not good, with only 3040% expected to survive after retrieval therapy. NEUROBLASTOMA Neuroblastoma is a tumour of neural crest origin which may occur in the adrenal medulla or anywhere along the sympathetic ganglion chain, namely in the neck, thorax, abdomen, and pelvis. Seventy-five per cent of tumours occur in the abdomen (adrenal medulla 50 %, paraspinal ganglia 25 %), 20 % occur in the thorax, and 5 % occur in the neck and the pelvis. Causes. Conclusive associations with environmental factors have not been proved in neuroblastoma. Hereditary factors are important in NB since a few cases exhibit predisposition following a dominant pattern of inheritance. The most characteristic cytogenetic abnormality of neuroblastoma is deletion of the short arm of chromosome 1 in locus 36 (1p36) occurring in 50 to 70% of primary diploid tumors. Another consistent chromosomal aberration identified in 25 to 30% of neuroblastoma cells is the presence of double-minute chromosomes, small fragments of chromatin containing multiple copies of the oncogene N-myc produced by amplification. N-myc protooncogene is found on chromosome 2p and its activation results in tumor formation. Pathology. Macroscopically, the tumor appears as a very vascular, nodular, friable, solid mass which grows rapidly and invades the adjacent tissues. Areas of haemorrhage, necrosis, and cystic degeneration are not uncommon Microscopically, a neuroblastoma is composed of small, round cells with little cytoplasm. The cells are arranged in rosettes which have fine nerve fibres in the centers. The degree of differentiation varies widely among different neural crest tumours: the most mature form is the benign ganglioneuroma. Spontaneous maturation of neuroblastoma to ganglioneuroma is a rare but welldescribed phenomenon. Stages. The Evans classification for neuroblastoma staging comprised: Stage I: tumor confined to an organ of origin. Stage II: tumor extending beyond an organ of origin, but not crossing the midline. Ipsilateral lymph nodes may be involved. Stage III: tumor extending beyond midline. Bilateral lymph nodes may be involved. Stage IV: remote disease involving skeleton, bone marrow, soft tissue or distant lymph nodes. Stage IVS: same as stage I or II with presence of disease in liver, skin or bone marrow. Frequency, age. The incidence of neuroblastoma is 9.6 per million populations. Of all patients, 50 % are younger than 2 years and 90 % are younger than 8 years; the peak incidence occurs at 18 months of age. Boys are affected slightly more often than girls. Clinical manifestations. The signs and symptoms of neuroblastoma reflect the location of primary, regional, and metastatic disease. Most primary tumors occur within the abdomen. Infants also have more thoracic and cervical primary tumors. In about 1 % of patients, a primary tumor cannot be found. Most children with neuroblastoma are diagnosed by the age 5 years, and the diagnosis is rare after the age of 10 years. Abdominal disease results in complaints of fullness, discomfort, and, rarely, gastrointestinal tract dysfunction. Physical examination commonly reveals a fixed, hard abdominal mass. There may be weight loss, failure to thrive, fever, anemia, abdominal fullness, abdominal pain, anorexia, nausea, and vomiting. Rarely, the child presents with intractable diarrhea due to production of vasoactive intestinal polypeptide by the tumor. Occasionally, hypertension and flushing may be caused by excessive catecholamine production. Pelvic neuroblastoma can cause disturbances of urinary function and defecation. Neuroblastoma sometimes presents with symptoms such as bone pain, subcutaneous nodules, and jaundice caused by metastatic lesions. 207 Diagnosis. Ultrasonography distinguishes neuroblastoma (solid, extrarenal) from cystic lesions and renal tumours. The radiographic detection of calcification in the tumour is suggestive of neuroblastoma. In children with an abdominal neuroblastoma, intravenous urography shows displacement rather than distortion of the pelvicaliceal system. A skeletal survey and chest radiograph are mandatory to detect possible metastases. CT gives good anatomical data about the tumour. Recent studies suggest that magnetic resonance imaging (MRI) is useful both to delineate the primary tumor and to evaluate bone marrow metastasis, vessel involvement, and extension into spinal cord. Treatment. The treatment modalities traditionally employed in the management of neuroblastoma are surgery, chemotherapy, and radiation therapy. The role of each method is determined by the natural history of individual cases considering stage, age, and histological features. Surgery plays the pivotal role in the management of neuroblastoma. Depending of the timing, operative procedures can have diagnostic as well as therapeutic functions. The goals of primary surgical procedures, performed before any other therapy, are to establish the diagnosis, to provide tissue for biological studies, to stage the tumor surgically, and to attempt to excise the tumor, if feasible. In delayed primary or second look surgery, the surgeon determines response to therapy and removes residual disease when possible. Chemotherapy is the predominant modality of management in management in neuroblastoma. Cyclophosphamide, vincristine, cisplatin, and doxorubicinare are the cornerstone of multiagent management. Drug combinations have been developed that take advantage of drug synergism, mechanism of cytotoxicity, and differences in side effects. Radiation therapy has been used in the multimodality management of residual neuroblastoma, bulky unresectable tumors, and disseminated disease. More recently, the role of radiation therapy in neuroblastoma continues to be refined with the improviment in multiagentchemotherapyand the increasing trend toward developing risk-related treatment groups based on age, stage, and biologic features. Of the new approaches which are being tried high-dose chemotherapy, total body irradiation, and allogeneic or autologous bone marrow transplantation appear particularly promising for neuroblastoma patients with a poor prognosis. Prognosis. The overall 3-year survival rate for all stages of neuroblastoma is 30% to 50 %. Young children with stage I/II have a better outcome. A poor outcome is characteristic of higher stages, older patients and those with bone cortex metastasis. Other prognostic variables are: the site of primary tumor development, maturity of tumor, presence of positive lymph nodes, high levels of ferritin, neuron-specific enolase, and diploid DNA. Neuroblastomas in newborns, cystic tumors, bilateral tumors in infants, and infants less than one year of age with neuroblastoma stage IV-S can undergo neuronal cell differentiation with spontaneous regression. It is thought that high level of TRK-A (transmembrane tyrosine kinase receptor) found in these cases might explain differentiation and regression as high level of this glycoprotein is associated with a favorable prognosis. Regression might be associated with nonaffected tumor cell apoptosis. RHABDOMYOSARCOMA A malignant tumor of mesenchimal cell origin is called a sarcoma. Mesenchymal cells normaly mature into skeletal muscle, smooth muscle, fat, fibrous tissue, bone, and cartilage. Rhabdomyosarcoma is thought to arise from immature mesenchimal cells that are committed to skeletal muscle lineage, but these tumors can arise in tissues in which striated muscle is not normally found, such as urinary bladder. Rhabdomyosarcoma (RMS), the most common soft tissue sarcoma in infants and children, represents about 5-15% of all malignant solid lesions. RMS arises from a primitive cell type and occurs in mesenchymal tissue at almost any body site excluding brain and bone. Causes. Most rhabdomyosarcoma occurs sporadically. Approximately 5% are associated to syndromes such as Beckwith-Wiedemann, the neurofibromatosis, basal cell nevus, and the fetal 208 alcohol syndrome. Other risk factors in the development of RMS include maternal use of marijuana and cocaine, exposure to radiation, and maternal history of stillbirth. Pathology. In children, rhabdomyosarcoma usually occurs in embryonic tissue that is capable of muscular differentiation. Cross striations and positive staining with the periodic acid are characteristic histological features. Electron microscopy reveals intracytoplasmic filaments and Zband materials. Antibodies against myosin and myoglobin are now available for diagnostic immunohistochemistry. The Intergroup Rhabdomyosarcoma Study divides tumors into 5 types: embryonal (57 %), alveolar (19 %), botryoid (6 %), undifferentiated (17 %), pleomorphic (1 %). The predominant histologic type in infants and small children is embryonal rhabdomyosarcoma, occurring in the head and neck, genitourinary tract and retroperitoneum. Embryonal rhabdomyosarcoma is associated with a favorable prognosis. Botryoid rhabdomyosarcoma is a subtype of the embryonal variety, which ordinarily extends into body cavities such as bladder, nasopharynx, vagina, or bile duct. The alveolar cell type, named for a superficial similarity to the pulmonary alveoli, is the most common form found on the muscle masses of the trunk and extremities, and is seen more frequently in older children and young adults. Alveolar rhabdomyosarcoma is associated with a poor prognosis. This unfavorable prognosis is the result of early and wide dissemination, bones marrow involvement and poor response to chemotherapy. Age. Rhabdomyosarcoma has a peak incidence before the age of five years, and a second surge during early adolescence. Head, neck and pelvic malignancies are more prevalent in infancy and early childhood, while trunk, extremity and paratesticular sites are largely a disease of adolescents. Clinical manifestations. Clinical findings, diagnostic evaluation and therapy depend upon location of the primary tumor. Head and neck RMS are most common and may be parameningeal or non-parameningeal. Patients with parameningeal tumours of the nasopharynx and paranasal sinus, apart from having local symptoms, are at risk of developing intracranial problems. Orbit-eyelid tumors produce proptosis and occasionally ophtalmoplegia. Tumors in this site are usually diagnosed before distant dissemination has taken place. Nonorbital parameningeal sarcomas arise most commonly in the nasopharynx and paranasal sinuses, the middle ear and mastoid region. These tumors usually produce nasal, aural, or sinus obstruction. Cranial nerve palsy, sometimes multiple, indicates direct extension toward the meninges. Headache, vomiting, and systemic hypertension may result from intracranial growth of tumor after erosion of contiguous bone at the cranial base. Genitourinary tract sarcomas are most frequently seen in the bladder and prostate. Bladder tumors tend to grow intraluminally, in or near the trigone, and have a polypoid appearance on endoscopic examination. Hematuria, urinary obstruction can occur. Affected children are usually younger than 4 years of age. Prostate tumors usually produce large pelvic masses with or without urethral strangury. These tumors can occur in infants or older children. Sarcomas of the extremity are characterized by swelling in the affected body part. Pain, tenderness, and redness may occur. The trunk, paratesticular tissues, perineum, retroperitoneum, abdominal viscera (liver, biliary tract, pelvis), and thorax are all known primary sites of rhabdomyosarcomas. Diagnosis. Biopsy (open, percutaneous, or endoscopic) is required for diagnosis and histological typing, which directs therapy. The extent of the tumour is defined by imaging techniques such as ultrasound, computed tomography (CT), or magnetic resonance imaging (MRI). Treatment is determined on an individual basis, according to the site, stage, and histological type of the tumor. Treatment of rhabdomyosarcoma should be multimodal, consisting of chemotherapy, surgery, and radiotherapy. 209 Surgery is the most rapid way to ablate the disease, and it should always be used if subsequent function or cosmetic will not be greatly impaired. In sites such as vagina and urinary bladder and most head and neck sites, incisional biopsy (for diagnosis) may be the only feasible surgical procedure because of proximity to vital blood vessels and nerves, cosmetic consideration, or both. The second-look operation is used to resect residual tumor after the administration chemotherapy or local radiotherapy. Radiation therapy can eradicate residual tumor cells from sites where surgical therapy alone cannot ablate the mass, especially in the head, neck, and pelvis. Preoperative chemotherapy may reduce the extent of surgery required and should be considered. Postoperative chemotherapy is helpful in eradicating residual disease and micrometastases. Chemotherapy is the primary treatment for patients with metastatic disease at presentation. The commonly used drugs are a combination of cyclophosphamide, vincristine, actinomycin D, and Adriamycin. Doxorubicin, DTIC (ditriazoimidazole carboximide), cisplatin, and ifosfamide have also been known to be effective agents. Prognosis. The overall 2-year survival rate is 65 %. Unfavourable histology, including alveolar monomorphous round cell or anaplastic tumours, is associated with a bad prognosis. Rhabdomyosarcomas of the distal genitourinary tract and the orbit have the best prognosis, while tumours of the extremities and trunk and the mucosal sites (perineum, retroperitoneum, abdominal viscera) have the worst prognosis. MALIGNANT HEPATIC TUMORS Primary neoplasms of the liver constitute between 0.5 % and 2 % of pediatric tumors and are the tenth most frequent tumor in children. A compilation of published series of hepatic tumors in children indicates that 57 % are malignant. Approximately 60 % of benign liver tumors are hemangiomas or hamartomas. Most of these lesions appear during the first 6 months of life. Benign vascular tumors can reach considerable size in infancy and may have an alarming clinical presentation, including high-output congestive heart failure (from arteriovenous shunting), hemorrhage and bleeding with evidence platelet consumption, and shock from rupture of a vascular tumor mass. Cavernous hemangioma and hemangioendothelioma are the two most important benign lesions that must be distinguished from malignant hepatic tumors. The most common malignant hepatic tumors are hepatoblastoma (HB) and hepatocellular carcinoma (HCC). Pathology. Hepatoblastoma is most often unifocal, and the right lobe of the liver is more commonly affected. Microscopic vascular spread may be found beyond an apparently encapsulated tumor. The gross appearance is that of a lobulated, bulging, tan mass, often punctuated by geographic areas of necrosis and surrounded by a pseudocapsule. The tumor has no association with cirrhosis. There are two morphologic types of hepatoblastoma. The pure epithelial type contains either fetal or embryonal cells or admixtures of the two. The mixed hepatoblastoma contains mesenchymal tissue in addition to the epithelial elements. Hepatocellular carcinoma in childhood is similar in gross and microscopic features to its adult counterpart, except for the lack of underlying cirrhosis in most pediatric cases. At the time of diagnosis, the tumor is often extensively invasive or multicentric, so resection is possible in fewer than 30 % of patients. Hemorrhage and necrosis within the tumor are found than in hepatoblastoma, and pseudoencapsulation is less notable. The tumor is often bile stained. HCC is distinguished from hepatoblastoma microscopically by the presence of cells larger than normal hepatocytes, broad trabeculae, considerable nuclear pleomorphism, nucleolar prominence, and absence of hematopoiesis. Clinical manifestation. Hepatoblastoma most frequently presents as an abdominal mass in children younger than 2 years. Some cases are first noted on routine physical examination, which is remarkable for the abdominal distention and associated hepatic enlargement. A discrete mass is not usually palpable. Splenomegaly is occasionally present. Rarely, the first presentation is acute 210 abdominal crisis secondary to rupture of the tumor. Jaundice, evidence of weight loss are present in a minority of patients. Severe osteopenia with back pain and pathologic fractures is present in 20 % to 30 % of patients; some degree of osteopenia is present in the majority of patients and regresses with tumor resection. Other infrequent features include hemihypertrophy and isosexual precocity, with penile and testicular enlargement in males and presents of pubic hair. The most common presentations of hepatocellular carcinoma are abdominal distention and right upper quadrant mass. These may be superimposed on the symptoms of preexisting disease such as tyrosinemia or cirrhosis. Abdominal pain occurs in approximately half of patients, and nausea and vomiting are common. Systemic manifestations, including fever, weight loss, and anorexia, are more common than in hepatoblastoma, and the duration of symptoms is short (mean, 1 or 2 month). Hemoperitoneum with an acute abdominal crisis is well recognized first presentation. Jaundice occurs in approximately 25 % of cases. Splenomegaly may be present when the patient has coexisting cirrhosis, as may other features of chronic liver disease. Polycythemia is occasionally present because of the extrarenal production of erythropoietin. Diagnosis Laboratory test Mild normochromic normocytic anemia is usual, although polycythemia is occasionally seen in HCC Thrombocytosis Modest elevations of liver enzymes and alkaline phosphatase Elevation of AFP level Diagnostic imaging Plain radiographs of the abdomen demonstrate the presence of a right upper quadrant mass, sometimes with calcification. Sonogfraphy is particularly useful in establishing the presence of an intrahepatic mass and differentiating solid from cystic masses. CT scanning can be used to define both local and distant extent of tumor involvement. The multiplanar capability of MRI aids in determining tumor extend, and MRI may be more accurate than CT in regard. MRI can also define vascular involvement and response to chemotherapy. Treatment Cure of malignant liver tumors in children is not possible without complete resection of the primary tumor; anatomic hepatic lobectomy has been necessary. Children have an excellent capacity for hepatic regeneration and can tolerate resection of up to 80 % of the liver. The advent of effective chemotherapy may permit cure in the presence of initially unresectable or metyastatic disease. Preoperative chemotherapy can convert a nonresectable tumor to a respectable one, has eradicated pulmonary metastases completely, and has eliminated multinodular tumor foci in the liver. The main chemotherapeutic agent is Adriamycin. Vincristine, cyclophosphamide, and 5-fluorouracil are also included in some regimens. Radiotherapy may also be used selectively. Before beginning therapy of hepatic tumor, an accurate tissue diagnosis is essential, so standard open liver biopsy is generally performed when the abdomen is opened at the time of the proposed resection. The presence of unresectable tumor in the liver would seem to provide a premier context for orthotopic liver transplantation. Prognosis. . Patients who have tumours completely resected have a survival rate of 80 % at 2 years. TERATOMAS Teratomas are tumors comprising more than a single cell type derived from more than one germ layer. A significant degree of confusion has arisen regarding nomenclature for the various 211 subtypes of teratomas. The word itself is derived from the Greek word teraton, meaning monster, and was used initially by Virchow in the first edition of his book on tumors, which was published in 1863. Teratomas range from benign, well-differentiated (mature) cystic lesions to those that are solid and malignant (immature). Besides being mature, with malignant transformation, teratomas also may be monodermal and highly specialized. The term dermoid cyst was coined in the veterinary literature in 1831 by Leblanc when he removed a lesion that resembled skin at the base of a horse’s skull, which he called a kyste dermoid. Both terms, now more than a century old, still are in general use and often are used interchangeably. The earliest implications were that dermoids were composed predominantly of elements similar to skin and its appendages, while teratomas had no such limits. Dermoids now are recognized as often being trigeminal and containing practically any type of tissue. In those who continue to make a distinction, dermoids are tumors that maintain rather orderly arrangements, with well-differentiated ectodermal and mesodermal tissues surrounding endodermal components. Teratomas, specifically solid teratomas, essentially are devoid of organization; thus, the presence of some degree of organization, a high degree of cellular differentiation, and cystic structure differentiates dermoids from teratomas. Pathophysiology of teratomas. Teratomas are made up of a variety of parenchymal cell types representative of more than a single germ layer, usually all 3. Arising from totipotential cells, these tumors typically are midline or paraxial. The most common location is sacrococcygeal (57%). Because they arise from totipotential cells, they are encountered commonly in the gonads (29%). By far the most common gonadal location is the ovary, although they also occur somewhat less frequently in the testes. Cystic teratomas occasionally occur in sequestered midline embryonic cell rests and can be mediastinal (7%), retroperitoneal (4%), cervical (3%), and intracranial (3%). Cells differentiate along various germ lines, essentially recapitulating any tissue of the body. Examples include hair, teeth, fat, skin, muscle, and endocrine tissue. Mature cystic teratomas can result in significant morbidity. Potential complications vary depending on the site of occurrence. SACROCOCCYGEAL TERATOMA Definition and Epidemiology. Sacrococcygeal teratomas (SCT) are diagnosed commonly in the prenatal period, and complications may occur in utero or during or after birth. Potential complications in utero include polyhydramnios and tumor hemorrhage, which can lead to anemia and nonimmune hydrops fetalis. If significant atrioventricular shunting occurs within the tumor, hydrops may result from high-output cardiac failure. Development of hydrops is an ominous sign. If it develops after 30 weeks’ gestation, the mortality rate is 25%. If it is recognized, delivery is recommended as soon as lung maturity is documented. Development of hydrops before 30 weeks’ gestation has an abysmal prognosis, with a 93% mortality rate. Antenatal diagnosis of SCT is very important and increasingly being made with fetal sonography. On ultrasound, SCT may be solid or mixed in echogenicity with interspersed or peripheral cystic components. The imaging of tumors which contain calcification varies in terms of increased echogenicity or echogenicity and shadowing Classification. Sacrococcygeal teratomas are classified according to the degree of exterior component or intrapelvic extension: Type I tumors are predominantly external, attached to the coccyx, and may have a small presacral component (45.8%). No metastases were associated with this group. Type II tumors have both an external mass and significant presacral pelvic extension (34%) and have a 6% metastases rate. Type III tumors are visible externally, but the predominant mass is pelvic and intraabdominal (8.6%). A 20% rate of metastases was found in this group. Type IV lesions are not visible externally but are entirely presacral (9.6%) and have an 8% metastases rate. Clinical manifestations. Sacrococcygeal teratomas are commonly very large ( average 8-10 cm ), well encapsulated and grossly lobulated. These masses possess both cystic and solid components. SCT is nearly always arising from the tip of the coccyx. 212 Benign teratomas usually produce no functional impairment. The presence of bladder or bowel dysfunction suggest a malignant lesion. Evidence for venous or lymphatic obstruction or lower leg paralysis is found more commonly in malignant tumors. In addition, pressure on a meningomeylocele will often be noticeably transmitted to the anterior fontanel. 15% of patients have associated congenital anomalies: imperforate anus, sacral bone defects, duplication of uterus or vagina, spina bifida, meningomyelocele. SCT is the most common congenital neoplasm of the fetus with an incidence of 1 in 40,000 births. About 80 per cent occur in girls, but it is more often malignant in boys. A substantial number have been encountered in twins. Most cases are asymptomatic in utero and diagnosed after birth. Fetuses with this malformation are at risk for significant perinatal morbidity and mortality. Complications. Postpartum morbidity associated with sacrococcygeal teratomas is attributable to associated congenital anomalies, mass effects of the tumor, recurrence, and intraoperative and postoperative complications. Approximately 10% of sacrococcygeal teratomas are associated with other congenital anomalies, primarily defects of the hindgut and cloacal region, which exceeds the baseline rate of 2.5% expected in the general population. Tumor mass and associated polyhydramnios frequently caused pre-term labor and delivery; fetal survival depended on lung maturity. Massive hemorrhage into the tumor with secondary fetal exsanguination sometimes occurred spontaneously in utero or was precipitated by labor and delivery. Dystocia, secondary to tumor bulk or tumor rupture, sometimes complicated delivery. Finally, in a few cases, placentomegaly and/or hydrops evolved, which, in turn, precipitated rapid fetal death. Differential diagnosis: meningomyelocele , rectal abscess , dermoid cyst , angioma , lipoma, neurogenic tumor, pilonidal cyst. Treatmen is primarily surgical, including removal of the coccyx. In fetuses with tumors larger than 5 cm, cesarean delivery should be considered to prevent dystocia or tumor rupture. Because of the poor prognosis associated with development of hydrops prior to 30 weeks’ gestation, these fetuses may benefit from in utero surgery. In most cases, sacrococcygeal teratomas should be resected electively in the first week of life, since long delays may be associated with a higher rate of malignancy. Complete excision should be done through a chevron-shaped buttock incision, with careful attention to the preservation of the muscles of the rectal sphincter. The coccyx always should be resected with the tumor, as failure to do so results in a 35-40% recurrence rate. Hemorrhage from the middle sacral vessels and hypogastric arteries is the most common complication. Malignant = surgical excision + chemotherapy + radiation (metastases to lung, bone, liver). Prognosis: Benign - disease free survival is greater than 90%; malignant - significant mortality, although good progress has been made recently in treatment of these tumors. Time of diagnoses is key: < 2 months of age, only 7-10% are malignant Age 1 year, 37% malignant Age 2 years, 50% malignant OVARIAN TERATOMA Mature cystic teratomas account for 10-20% of all ovarian neoplasms. Not only are they the most common ovarian germ cell tumor but also the most common ovarian neoplasm in patients younger than 20 years. They are bilateral in 8-15% of cases. Mature cystic teratomas of the ovary often are discovered as incidental findings on physical examination, during radiographic studies, or during abdominal surgery performed for other indications. Asymptomatic mature cystic teratomas of the ovaries have been reported at rates of 665% in various series. When symptoms are present, they usually consist of abdominal pain (47.6%), abdominal mass or swelling (15.4%), and abnormal uterine bleeding (15.1%). Bladder symptoms, gastrointestinal disturbances, and back pain are less frequent. When abdominal pain is present, it usually is constant and ranges from slight to moderate in intensity. Torsion and acute rupture 213 commonly are associated with severe pain. Hormonal production is thought to account for cases of abnormal uterine bleeding, but histologic examination has not provided evidence of this theory. Complications of ovarian teratomas include torsion, rupture, infection, hemolytic anemia, and malignant degeneration. Torsion is by far the most significant cause of morbidity, occurring in 3.2-16% of cases. Several series have demonstrated that increasing tumor size correlates with increased risk of torsion. Rupture of a cystic teratoma may be spontaneous or associated with torsion and occurs in approximately 1-4% of cases. Rupture may occur suddenly, leading to shock or hemorrhage with acute chemical peritonitis. Chronic leakage also may occur, with resultant granulomatous peritonitis. Prognosis after rupture usually is favorable, but the rupture often results in formation of dense adhesive disease. Infection is uncommon and occurs in only 1% of cases. Coliform bacteria are the organisms most commonly implicated. Autoimmune hemolytic anemia has been associated with mature cystic teratomas. In several series, removal of the tumor resulted in complete resolution of symptoms. In this context, radiologic imaging of the pelvis may be indicated in cases of refractory hemolytic anemia. In its pure form, mature cystic teratoma of the ovary always is benign, but in approximately 2% of cases, it may undergo malignant transformation into one of its elements. The prognosis for patients with malignant degeneration is dismal, with 5-year survival rates reported in the range of 1531%. The prognosis appears to be somewhat better if the malignant element is squamous rather than adenocarcinoma. Mature cystic teratomas of the ovaries should be removed by simple cystectomy rather than salpingo-oophorectomy. Although the rate of malignant degeneration is only 1%, the cyst should be removed in its entirety, and if immature elements are found, the patient should undergo a standard staging procedure. The patient should be counseled appropriately about the risks and benefits of laparoscopy and laparotomy. Ample literature supports laparoscopy as an acceptable alternative approach in resection. Benefits include reductions in postoperative pain, blood loss, hospital stay, and total cost. Risks include prolonged operative time, increased operating room costs, and potential need for a prompt second staging procedure if an unexpected malignancy is revealed. Some studies have found an increased intraoperative spillage rate with laparoscopy, while others have not. Spillage is associated with increased risk of chemical peritonitis (estimated incidence of 0.2%) and increased risk of adhesion formation. The risks of recurrence (4%), as well as malignant degeneration (0.17-2%), should be discussed. TESTICULAR TERATOMA The incidence of all testicular tumors in men is 2.1-2.5 per 100,000. Germ cell tumors represent 95% of testicular tumors after puberty, but pure benign teratomas of the testis are rare, accounting for only 3-5% of germ cell tumors. The incidence of all testicular tumors in prepubertal boys is 0.5-2 per 100,000, with mature teratomas accounting for 14-27% of these tumors. It is the second most common germ cell tumor in this population. Childhood testicular teratomas are uniformly benign, with no documented cases of retroperitoneal or lung metastasis in differentiated lesions. Most morbidity is a result of surgical or postoperative complications, such as hemorrhage or infection. The mortality rate is less than 1 per million. Pure teratomas of the testis are rare. During and after puberty, however, even mature teratomas (composed of entirely mature histologic elements) can metastasize to retroperitoneal lymph nodes or systemically, regardless of their histologic appearance. Morbidity is associated with growth of the tumor, which may invade or obstruct local structures and become unresectable. Malignant transformation is significantly more common in testicular teratomas than in their ovarian counterparts, and recurrence risk is around 20% in both mature and immature testicular teratomas. 214 Testicular teratomas most often present as a painless scrotal mass, except in the case of torsion. The masses are firm or hard in 83% of cases. Most are not tender and do not transilluminate. Testicular pain and scrotal swelling occasionally are reported with teratomas, but this is nonspecific and simply indicates torsion until proven otherwise. Hydrocele frequently is associated with teratoma in childhood. On examination, the testis is diffusely enlarged, rather than nodular, although a discreet nodule in the upper or lower pole sometimes can be appreciated. Testicular teratomas traditionally have been treated by simple or radical orchiectomy. More recently, conservative excision by enucleation also has been recommended for prepubertal teratomas of the testis. The risk of malignancy increases with maturation of the testes, and this is a significant concern in children at or near puberty. In this group, areas of normal surrounding testicular tissue should be excised and sent for frozen section. If frozen section reveals areas of maturity, proceeding to orchiectomy is recommended. Enucleation or partial orchiectomy for teratoma in pubertal or adult males is not recommended. HAMARTOMAS AND VASCULAR MALFORMATION NAEVI The term naevus refers to a hamartomatous malformation of the skin. Naevi may be principally composed of dermal elements, such as connective tissue naevus, melanocytes (naevocellular naevus), vascular elements, or epidermal elements (epidermal naevi). Epidermal naevi Epidermal naevi are verrucous or wart-like and are frequently present at birth although may develop later in childhood or (rarely) in adult life. They may be small, resembling true viral warts, but more typically they form large linear plaques or linear arrays of warty papules. Rarely, large areas of the body surface may be covered by linear or swirling arrays of these lesions. Epidermal naevi are typically asymptomatic, although large linear naevi may become spontaneously inflamed, with the development of pruritus and erythema of the lesions and surrounding skin. Histologically, epidermal naevi are characterized by acanthosis and hyperkeratosis. Cytological atypism is not seen. They are most commonly removed for cosmetic reasons. Such treatment may involve excision with primary closure, electrodesiccation, carbon dioxide laser ablation, or cryosurgery. Epidermal naevi are generally of little consequence to the general health of the patient. Very rarely, they may be associated with congenital malformations of underlying osseous and soft tissue structures, particularly when lesions occur on the head and neck. Malignant transformation within epidermal naevi is exceedingly rare, except in the case of a naevus sebaceus. Naevus sebaceus is a type of epidermal naevus that occurs exclusively on the scalp or face. Histologically, naevus sebaceus is characterized by the same type of epidermal proliferation seen in other epidermal naevi, but large mature sebaceus glands and apocrine glands are also present. Before puberty, naevus sebaceus is typically a smooth-surfaced flat plaque with slightly yellowish or yelloworange colour. When it occurs on the scalp, which is the most common site, the absence of hair within the lesion may bring it to attention. At puberty, the sebaceous element within the naevus begin to hypertrophy and the surface becomes more verrucous. Unlike other epidermal naevi, naevus sebaceus may occasionally undergo malignant transformation, with the formation of basal cell carcinoma within the lesion. Since such transformation occurs in only about 5 %of patients with naevus sebaceus, the common practice of excising these lesions prophylactically is controversial. Benign tumours such as syringocystadenoma papilliferum may also occur within these naevi. Connective tissue naevi Connective tissue naevi are generally present at birth. They consist of firm, flesh-coloured papules and plaques and are usually solitary. The hair follicle orifices may be prominent within lesions, giving them the appearance of pig skin. Connective tissue naevi are usually idiopathic and are 215 not associated with any other disease, with the exception of the shagreen patch that occurs in tuberous sclerosis. Histologically, connective tissue naevi are composed of dense aggregations of dermal elements, usually collagen fibres or elastic fibres, or both. Connective tissue naevi are harmless, although they may be excised for cosmetic or functional reasons. HAEMANGIOMAS AND VASCULAR MALFORMATIONS Haemangiomas are proliferations of mature vascular elements. These endothelium-lined vascular spaces are most commonly capillary sized, but larger cavernous spaces also are found, especially in large lesions. Different clinical types of haemangiomas are commonly recognized. Strawberry haemangiomas may be present at birth but, more typically, develop during the first few weeks of life. They are seen in approximately 3 % of newborn infants, and 80 % are solitary, although multiple haemangiomas also occur. Strawberry haemangiomas range in size from 1 mm to many centimetres. The lesions are well-demarcated, lobular, bright red nodules with a spongy consistency. The surface of the lesion is studded with small capillary tufts, which produce the resemblance to a strawberry. Strawberry haemangiomas seldom require treatment, since the vast majority involute spontaneously by the age of 6 or 7 years. Treatment may be required, however, for lesions situated on the eyelids, nares, or lips, where they may cause functional impairment. Rarely, giant strawberry haemangiomas, particularly those with a cavernous component, may be associated with thrombocytopenia, presumably due to platelet sequestration with the lesion. This phenomenon, known as the Kasabach-Merritt syndrome, may require surgical treatment if other measures fail. Administration of corticosteroids, which may stimulate gradual involution of lesions is often used as first-line treatment for rapidly growing strawberry haemangiomas. Surgical excision and carbon dioxide laser ablation are often successful, but may produce unacceptable scarring. The efficacy of dye laser treatment is currently being evaluated and promises to be effective. Cherry haemangiomas are generally smaller than strawberry haemangiomas, and tend to be round and bright red. They begin to appear during childhood, and continue to develop throughout adult life. The tendency to develop cherry haemangiomas appears to be transmitted within families as an autosomal dominant trait. Cherry haemangiomas seldom require treatment other than for cosmetic reasons: they are easily excised with a scalpel or biopsy punch. Occasionally, cherry haemangiomas thrombose, changing in colour from bright red to purplish black. This colour change may alarm patient and physician alike, since the apparent sudden appearance of a black papule raises the spectre of nodular malignant melanoma. Biopsy is indicated in such cases. Cavernous haemangiomas, like strawberry haemangiomas, may be present at birth and grow rapidly during the first few months of life. They also involute spontaneously. Cavernous haemangiomas are primarily situated beneath the skin, and clinically appear as soft, bluish masses that distend the surrounding features. A typical strawberry haemangioma may form the cutaneous component of a cavernous haemangioma. Both strawberry and cavernous haemangiomas, when multiple, may be the presenting sign of diffuse neonatal haemangiomatosis, in which multiple haemangiomas occur not only in the skin and subcutaneous tissue, but also in the liver and other organs. Port wine stains, unlike haemangiomas, do not represent the proliferation of excessive numbers of vascular elements, but are caused by ectasia of normal numbers of vessels within the skin. The dermal vessels that comprise port wine stains are capillary size or slightly larger. Port wine stains are generally present at birth, and occur in 0.3 %of neonates. Early in life, port wine stains are generally pink or purplish-pink in colour, and macular. With time, the vascular channels become more and more ectatic, imparting a lumpy appearance to the skin. Mature port wine stains are frequently dark purple. Port wine stains are most commonly found on the head and neck, but may also be seen on the trunk, particularly in the pectoral area, and on the extremities, usually the arms. Port wine stains of the orbital region may be associated with unilateral glaucoma. 216 The Sturge-Weber syndrome is characterized by the presence of a port wine stain in the distribution of the first branch of the trigeminal nerve, associated with a similar vascular malformation of the underlying cerebral cortex and meninges. Seizures, mental retardation, and motor cortical deficits are seen in many patients. The Klippel-Trenaunay-Weber syndrome is an association of port wine stain of an extremity or the trunk with arteriovenous malformations and hemihypertrophy. Treatment for port wine stains was unsatisfactory and produced unacceptable scarring: cryosurgery, carbon dioxide and argon laser surgery, excision and grafting, and tattooing with skincoloured pigments were all used with variable degrees of success. The development of tuneable dye lasers has revolutionized the treatment of port wine stains, making it possible to remove these lesions partially or completely without excessive scarring. Pyogenic granuloma is a common vascular lesion that presents as a rapidly-growing papule or nodule which is friable and bleeds easily after minor trauma. Pyogenic granuloma is a misnomer: it is actually an eruptive capillary haemangioma. Treatment with electrofulguration, carbon dioxide laser ablation, or simple excision is usually curative, although lesions may recur. Since the differential diagnosis of a rapidly growing and bleeding nodule also includes nodular malignant melanoma, biopsy should be performed if there is any doubt about the diagnosis. LYMPHANGIOMAS Lymphangiomas may be composed of capillary sized lymphatic vessels, or they may consist of larger cavernous spaces. Lymphangioma circumscriptum is a common type of lymphangioma. Lesions consist of a superficial proliferation of capillary sized lymphatic vessels, which produces the appearance of multiple vesicles on the cutaneous surface, and a deeper component consisting of large cisternae within adjacent muscle tissue. The appearance of the superficial portion of lymphangioma circumscriptum has been likened to frog eggs. Small precipitates of red blood cells can often be seen at the bottom of the lymphatic vesicles. Treatment of lymphangioma circumscriptum may be attempted for cosmetic reasons. Both excision and carbon dioxide laser ablation have been successfully employed, but the connection of the skin to the deeper cisternae means that recurrences are common. Cavernous lymphangiomas and cystic hygromas are proliferations of lymphatic vascular tissue consisting of larger vascular spaces than those seen in lymphangioma circumscriptum. Cystic hygroma is the more common of the two; it most frequently occurs in the neck, although it may be seen on the head or inguinal regions. Cystic hygroma behaves like a benign tumour and grows slowly in size. Large lesions may cause functional impairment, particularly in the neck. Surgical excision is difficult, but highly successful in cystic hygroma. Excision of cavernous lymphangiomas is less likely to be curative; recurrence is common. 217