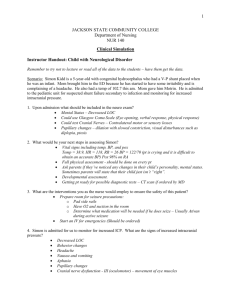
Neuro Med- Surg Practice Questions
advertisement

--Hi all! I hope these help all of you that were looking out for these. I just finished them tonight. There are like 180 flippin questions, but since there were 182 sides, I thought this sounded about right. I went straight off the notes and book. –Enjoy!-Elizabeth Neuro Med- Surg Practice Questions 1. What are the three components of the cranial vault? Brain tissue, blood, CSF. The Monro-Kellie Hypothesis states that an increase in any of these components causes a change in the volume of others by displacing or shifting CSF, CSF absorption increases and blood volume decreases. 2. What is the normal ICP? 10- 15mmHg 3. What is increased ICP commonly associated with? head injury 4. Give some examples of secondary conditions that could cause increased ICP? brain tumors, subarachnoid hemorrhage, encephalopathies 5. How long would it take for irreversible brain damage to occur r/t ischemia? >3-5 min. 6. What changes pertaining to vital signs might you see in the first stage of cerebral ischemia? Slow bounding pulse, respiratory irregularities 7. Define the Cushing’s Response to increased ICP. the brain’s attempt to restore blood flow by increasing arterial pressure to overcome increased ICP. Remember that pressure is increasing because the body detects ischemia to the brain (decreased blood flow). This is considered to be the decompensation phase 8. What are the triad of symptoms seen in the Cushing’s Response? Widening pulse pressure (HTN), respiratory changes and bradycardia. She also mentions that the temp. increases 9. Cheyne- Stokes respirations may be seen during the decompensation stage of increased ICP. Describe Cheyne- Stokes respirations A breathing pattern marked by a period of apnea lasting 10-60sec, followed by hyperventilation. –Taber’s Dictionary 10. What is the most important indicator of increased ICP and what are the other s/s? Change in LOC; restlessness without a cause, increased drowsiness and confusion. These changes warrant immediate intervention including notifying CN and Dr. 11. What is the goal of mgmt for increased ICP? Decrease cerebral edema and decreasing blood volume while maintaining cerebral perfusion 12. What are 2 osmotic diuretics given to dehydrate brain and reduce cerebral edema? Mannitol and glycerol 13. What could cause the risk for infection in increased ICP? An ICP sensor insertion 14. What are the nsg interventions appropriate for increased ICP? insert foley catheter to monitor output, serum osmolality to assess hydration, give corticosteroids to reduce edema, maintain cerebral infusion with IV fluids and inotropic agents, give stool softeners to avoid straining, maintain a calm environment, control fever with anti- pyretics to decrease rate of cerebral edema 15. What are primary examples of head injuries? contusions, lacerations, torn blood vessels, foreign object penetrations 16. When does an acceleration injury occur? when the head is in motion 17. When does a deceleration injury occur? when the head is stopped 18. Skull fractures can be open or closed. What is difference between these two? A tear in the dura is seen in an open fracture, and the dura is intact ina closed fracture 19. What are the types of skull fractures? simple (simple clean break) comminuted (splintered fracture), depressed (bone depression that are depressed into the brain), basilar ( fracture at the base of the skull). X rays are needed for diagnosis 20. What are manifestations are commonly seen in basilar skull fractures? hemorrhage, CSF leakage, Battle’ s sign seen (bruising to lower skull behind ear) 21. What might bloody CSF suggest? brain laceration or contusion 22. Where could CSF leak from? from ears (otorrhea) from nose (rhinorrhea). I f CSF leaking, pressure should not be put in these sites to block leakage (this might increase cerebral pressure). Instead we could catch a sterile CSF sample for the lab, then get sterile gauze strip and tape it lightly over the leakage site. Teach pt not to blow nose. 23. What are some nsg interventions seen in skull fractures? HOB 30 degrees, 24. IV abx (if depressed fracture has imbedded in the brain), monitor for CSF leakage, observe closely if pt not surgical 25. What is the main difference between a concussion and contusion? In concussion, you may or may not lose consciousness, and in a contusion, the client does lose consciousness 26. What should we observe in persons that have had a concussion? make sure no difficulty speaking, vomiting, dizziness, and to arouse LOC. This may take several days to get over. 27. A contusion is a medical emergency when the brain gets bruised. What might we see in a pt with a contusion? decreased BP and respirations, loss of bowel and bladder, may have HA or seizures. These patients are very hyperactive and this might take several months to get over 28. What type of hematoma results from arterial bleeding in the space between the dura and the inner surface of the skull Epidural hematoma. These can be caused by fractures in temporal bones 29. What are clinical manifestations seen in an epidural hematoma? Initial unconsciousness, brief period of lucidity, then decreased LOC 30. This is a medical emergency that could result in CNS failure within minutes. What are some medical interventions that can be done for this? Create burr holes through, possible craniotomy, drain blood that is causing the hematoma 31. What type of hematoma results from venous bleeding into the space beneath the dura and the arachnoid space subdural hematoma; She also says that most subdural hematomas are from venous bleeds, but they could be from arterial bleeds. If so, the condition greatly accelerates 32. What could cause subdural hematomas bleeding disorders, or ruptured aneurysms, trauma 33. There are 3 types of subdural hematomas: acute (major head traumas in 24-48hrs), subacute (less severe contusions 48hrs-2wks), and chronic (3 wks –3 months). What s/s are seen in acute and subacute: changes in LOC, pupil changes, increased BP 34. What type of hemorrhage is caused by a tear in the small arteries and veins in the white matter? Intracranial hemorrhage 35. What are some causes of intracranial hemorrhage? Direct trauma such as GSW, missile injuries, stab wounds, tumor and bleeding around tumor, HTN crisis, anti- coagulant therapy and bleeding problems 36. What is involved in the medical mgmt of brain injuries? physical and mental exams, CT & MRI scans, possible vent. Support, seizure prevention, F&E maintenance, nutritional support, mgmt of pain and anxiety 37. What are nsg responsibilities in a neurological assessment? Assess baseline and/or any changes in LOC, VS, pupil size, motor function. 38. There are 2 types of stroke, ischemic and hemorrhagic. What are the 3 sub-types of ischemic stroke? TIA, thrombotic and embolic 39. What occurs in a thrombotic stroke? A blood clot clogs vessels in the brain which leads to narrowing of the vessel lumen or ischemia 40. What occurs in an embolic stroke? A blood clot or plaque has traveled from another area in the body and has occluded a cerebral artery 41. Where do most embolic strokes originate from? the endocardial layer of the heart. These may come from a Hx of MI, endocardial disease, valve placement, A-fib 42. What occurs in a hemorrhagic stroke? Bleeding occurs in the brain tissue, ventricles or the subarachnoid space. This can be caused by HTN, or ruptured aneurysms 43. How long can a TIA last? 15min to 24hrs 44. What is the most important thing to know about a TIA? this serves as a WARNING SIGN or precursor to a CVA in the future 45. Do people that have TIAs experience a full recovery between attacks? yes 46. What are some motor deficits that may come with strokes? hemiparesis (numb on one side), hemiplegia (paralysis on one side), ataxia (defective voluntary m. coordination) 47. What are some communication deficits that may come with strokes? dysarthria (clumsiness in articulating words r/t CVA disease, no aphasia), aphasia (inability to communicate r/t to CVA), receptive aphasia (saying words that have a backward meaning). Dysphagia (difficulty or inability swallowing) may also be present. 48. What cognitive impairments may come from a stroke? memory loss, decreased attention span, poor reasoning, altered judgement, apraxia (inability to perform a familiar act i.e., picking up a fork) 49. What psychological impairments may come from a stroke? loss of self control, emotional lability, depression 50. What perceptual disturbances may one experience in a stroke? homonymous hemianiopia, loss of peripheral vision, diplopia, difficulty judging distances 51. What tests could be used to diagnosis a stroke? CT without contrast, hx, assessment, neuro exam, cerebral angiogram, transcranial doppler, TEE (to check the back of the heart for any broken off clot pieces 52. If someone is diagnosed as having a hemorrhagic stroke, are clot-busters or anti-coagulants an option for treatment? NO! 53. Thrombolytic therapy should be started within 3 hours of s/s of CVA. What should be taken into consideration before starting thrombolytic therapy? Bleeding studies, Hx of GI bleed in 3 days? Surgery in past 2 wks? Results of the noncontrast CT (what type of stroke did it show?) 54. What sx interventions could prevent a CVA? carotid endarectomy, carotid stenting, aneurysm clipping or coiling, AVM resectioning. 55. What is an AVM? arteriovenous malformation (when a vein and artery mesh up and cause clots) 56. The key to CVA medical mgmt is prevention. What are some modifiable risk factors? HTN, smoking, increased lipids, sedentary lifestyle, A-fi (with coumadin), obesity, excessive alcohol consumption, DM Type 2, carotid stenosis 57. What meds could help prevent CVAs? antihypertensives, coumadin (for A-fib), Plavix, ASA, statins 58. What is focus of care when CVA pt is in an acute care setting? recovery and maintaining a calm environment 59. What is the focus of care when CVA pt is in a rehab facility? getting back to ADLs. think BOOTCAMP!!! 60. What are the nsg interventions for a CVA pt? Monitor for constipation, skin breakdown, normal bladder function, Monitor CV function, nutritional status, arrange client’s environment within perceptual field, give explanations to pt and family about situations and procedures 61. What is spasticity? a motor disorder that demonstrates velocity-dependent increased muscle tone, exaggerated tendon jerks, and clonus 62. Read the goals of care for CVA pts. Too much to type… 63. What could help achieve self- care in CVA pts? start with the affected side, encourage personal hygiene as soon as pt could sit up, use clothing that is focus, dressing in a seated balanced position. Pt’s morale is greatly improved if they are fully dressed. 64. How can we attain bladder control? offer urinal or bedpan on schedule. Upright posture and standing position for males 65. What would be helpful in when modifying the home of a CVA pt? having an OT assess it and make recommendations, using a shower stool, long handled bath brush, portable shower hose, handrails 66. Where could secondary brain tumors stem from? from structures outside the brain such as lung, breast, lower GI, pancreas, kidney, skin 67. What is the most common type of brain neoplasm? Gliomas, which spread by infiltrating into surrounding tissues 68. When attempting to remove a glioma, what should we understand? Total removal causes considerable damage to vital structures 69. What is the most common pituitary tumor? adenoma. Symptoms are caused by pressure on adjacent structures or hormonal changes 70. What are some characteristics of menigiomas? they are encapsulated, globular, and are demarcated (have boundary or limit) These also tend to recur 71. An acoustic neuroma usually occurs on the 8th cranial nerve. What are some common symptoms of this? hearing loss, tinnitus, dizziness 72. S/S of brain tumors mimic s/s of increased ICP. What are these symptoms? Headache, vomiting, papilledema, personality changes, focal deficits (motor, sensory, cranial nerve dysfunctions) 73. What is papilledema? edema and inflammation of the optic nerve at the entrance point into the retina 74. What tests could diagnose a pt with a brain tumor? CT, MRI, PET scan, cerebral angiography, EEG, steriostatic biopsy, cytologic study of CSF 75. What are the surgical intervention options for a person with a brain tumor? transphenoidal (through nose) microsurgical removal, gamma knife radiation(no incision), external beam radiation, stereotactic laser or radiation therapy, and brachytherapy. 76. What is brachytherapy? surgical implantation of radiation sources 77. What should be done for nsg mgmt of these pts whom have undergone surgical trt? Monitor for increased ICP, monitor for/prevent aspiration and check swallowing ability (may need suctioning equipment), monitor for seizures, assess speech and motor function, assess pupils, may need frequent reorientation 78. What percent of intracranial tumors are metastatic? 10% 79. What are the s/s of metastatic brain tumors? HA, paralysis, seizures, aphasia (inability to communicate), focal weakness, altered mentation (mental activity), personality changes 80.Is chemotherapy use the first line of trt for brain tumors? No, because chemo does not cross the blood brain barrier. It may be given as a last effort via the CSF along with radiation ‘wafers’ that dissolve over time. 81. What is the definition of a seizure? sudden, abnormal excessive electrical activity within the brain 82. The primary cause of a seizure may not have an identifiable cause, and these account for ½ of all seizures. What secondary conditions could cause a seizure? hypoxemia, fever, head injury, CNS infections, metabolic/toxic conditions, brain tumors, drug or –ETOH withdrawal, allergies 83. What are the 6 types of seizures? tonic, clonic, tonic-clonic, myoclonic, absence, atonic or akinetic 84. Briefly describe these 6 types (I got these answers from the Taber’s dictionary) 85. Tonic- muscle tension seen 86. Clonic- alternately contracting and relaxing the muscles 87. Tonic- clonic aka ‘grand mal’-… both tonic and clonic These may last 2-5 min. and pt may lose continence. Muscle spasms seen. 88.Myoclonic- twitching or clonic spasms of a muscle or group of muscles 89. Absence aka ‘petit mal’- starring off for a few seconds 90. Atonic- loss of muscle tone may occur and pt may fall down 91. What are pts that experience seizures at risk for? hypoxia, vomiting, pulmonary aspiration, and persistent metabolic abnormalities 92. What is the goal of trt for seizure pts? controlling the seizure and cause of seizure. Mgmt must meet the individual’s needs, and drug therapy should be used to achieve seizure control (not cure) with minimal side effects 93. What is status epilepticus? a major medical emergency involving acute prolonged seizure activity. This is a seizure that either lasts for 30min. or longer, or, series of seizures lasting 510min. 94. If untreated, what could status epilepticus lead to? cerebral anoxia and edema. This could cause irreversible and fatal brain damage 95. What is the goal of mgmt for this condition? stop seizure ASAP, ensure adequate cerebral oxygenation (Remember ABCs), maintain seizure free state, ensure safety (apply seizure pads, keep pillow available 96. What are some nsg interventions for this? Maintain and assess for adequate ABC (may need oral airway if mouth not closed and suctioning at the bedside), Apply O2, position patient to maintain the airway, position them gently to the floor if standing, don’t insert anything in their mouth, don’t restrain them, loosen restrictive clothing, keep head protected, call for help (and if @ home- call 911), monitor for bleeding or s/s of infection if tongue or mouth damaged, reorient pt after seizure is over, stay with patient and observe all characteristics of the seizure 97. What are the characteristics of seizures that we observe for and document? Identify activities that occurred immediately before the onset of seizure, was the client aware a seizure was going to occur? If so, how did the client know? Describe the type of mvmts, presence of incontinence? Presence of apnea or cyanosis? Duration and time of seizure? Changes in LOC? Condition of client after seizure (oriented, level of activity, weakness?) 98. Vagal nerve stimulation may be used for seizure treatment of intractable simple or complex partial seizures. Does this involve surgery? Yes, a device is surgically implanted into the chest wall to deliver intermittent stimulation to vagal nerve 99. Are vessels usually dilated or constricted to cause a HA? DILATED. They may be caused by stress or skeletal muscle tension 100. What are the examples of the primary type of HA? migraine, tension, cluster, cranial arteritis 101. What are types of secondary HA? HA from brain tumor or aneurysm 102. What are migraines? recurring vascular HA that have either unilateral or bilateral throbbing pain 103. What are the 2 types of migraines? With aura (visual disturbances, paresthesias or motor deficits) or without aura 104. What are the 4 phases of a migraine? prodrome (approaching), aura, HA, and recovery. Just look over the s/s of each phase..too much to write 105. What is used for the medical mgmt of migraines? serotonin receptor agonists, anti- migraine agents. We want to cause vasoconstriction and decrease inflammation 106. What classifications of medications may be used to prevent migraines? anti-epileptics, antihypertensives, anti-depressants. Botox may also be used 107. What are some common migraine triggers? fatigue, nitrites, sleep deprivation, depression, processed foods, MSG, high tyramine foods (wine, chocolate, aged cheese), dairy products, overuse of certain meds (Excedrin because of high caffeine content), menstrual cycle 108. What nsg interventions could help relieve migraine pain? providing and dark quiet room, administer abortive med ASAP, elevate HOB 30 degrees, give antiemetics as needed 109. What is a cluster HA? Severe vascular HA that may occur 1-8 times daily. Mostly occur in men 110. What are some characteristics of a cluster HA? penetrating and steady. May have watering of eyes and nose (rhinorrhea) and attacks may last for 15min to 3 hours 111. What are the s/s of cluster HA? may have excruciating, orbital, or supraorbital pain, tenderness of temporal artery, facial flushing with elevated skin temp on affected side, very restless behavior 112. What could precipitate cluster HA? -ETOH, nitrites, vasodilators, and histamines 113. Should we apply O2 to pts with cluster HA? Yes. 7-9L for 15min. 114. What medications could be given to prevent cluster HA? Calcium Channel Blockers and corticosteroids 115. In cranial arteritis, inflammation along the temporal arteries occurs and we may be able to see the inflamed artery. How could we get a definitive diagnosis of this? from subjective/objective manifestations or even a biopsy of the artery 116. What are the s/s of cranial arteritis? fatigue, weight loss, malaise, fever, inflammation over artery, visual problems from ischemia 117. What is the trt for cranial arteritis? give corticosteroids, analgesics prn. Teach the patient not to abruptly stop medication trt (may relapse) and complete their course of medication 118. Tension HA are probably the most common type of HA. What occurs in a tension HA? contractions of muscles in neck and scalp. Most likely caused by stress 119. What might tension HA be described as? band-like weight on top of head, steady constant pressure 120. What could we teach pt to help avoid tension HA? exercise, meditation, application of heat to site, massage, pain meds, anti-depressants and m. relaxers may help 121. What are 3 types of neurologic infections? meningitis, encephalitis, brain abscess 122. The 2 types of meningitis are bacterial and viral. Which type of meningitis is more fatal? Bacterial 123. What are the s/s of menigitis? fever, nuchal rigidity (stiff neck), HA, Positive Kernig’s sign, positive Brudzinski’s sign, photophobia 124. What is Kernig’s sign? when hamstrings contract while attempting to extend the leg after flexing the hip 125. What is Brudzinki’s sign? flexion of hips when the neck is flexed from a supine position 126. What is the definition of MS? a progressive degenerative disorder characterized by the demyelination of nerve fibers of the brain and spinal cord. Most likely in women from 20-40 and is characterized by periods of remission and exacerbation 127. What are the 4 types of MS? Relapsing remitting- exacerbation followed by complete or partial remission Primary progressive- shows progression from onset with occasional plateau and temporary minor improvements Secondary progressing- no real periods of remission, only small breaks in attacks Progressive relapsing- gradual decline usually seen in men. No real periods of remission 128. What are the early signs of MS? parasthesias, blurry or double vision (usually the first sign), loss of balance, weakness in one or more limbs 129. As this progresses, how would this effect the motor system? fatigue, stiffness, positive Babinski’s, visual difficulties, intention tremor, unsteady gait, hyperactive DTR’s, high spasticity, dysmetria and nystagmus may be seen 130. What is dysmetria? Inability to control R.O.M. 131. How could MS effect our sensory system? parathesias, facial pain, burning, problems with bowel and bladder function, and sexual dysfunction may be seen 132. How could MS effect our cognition? inattentativeness, impaired judgement, decreased concentration-short term memory and ability to perform calculations may be seen 133. How can we diagnose MS? MRI (MS plaques may be seen), CFS analysis, neuropsychological testing, sexual history, and evoked potential studies 134. Is there a cure for MS? no 135. What is the goal of trt? To delay the progression, manage symptoms, and treat acute symptoms. Medications may be given to modify the disease, decrease spasticity, help with urinary problems and for CNS stimulation( for fatigue) 136. Should an MS pt do strenuous exercise? No. This could exacerbate their MS. Walking, swimming, and stretching are best for these pts. Activity should be individualized. 137. What could we teach our MS pts? About their meds, how to use a cane, walker or wheelchair, bowel and bladder training if needed, and to avoid temperature extremes to prevent exacerbation 138. What ids the definition of myasthenia gravis (MG)? an autoimmune disease that involves a decrease in the number and effectiveness of acetlycholine receptors at the neuromuscular junction 139. What does research strongly suggest is the cause of the decrease in acetlycholine receptors? it suggests that antibodies found in the thymus gland damage or block the ACh muscle receptors. It is also associated with thymic tumors. This inhibits muscle contractions. 140. What are the s/s of MG? Fatigue, extreme muscle weakness (patients stronger in the morning and weak in the evening), ptosis, diplopia, dysphonia, and Bulbar signs 141. What are Bulbar signs? combination of chewing, swallowing, and speaking difficulties 142. How could we diagnose MG? Tensilon test (given IV and must have Atropine @ BS for cardiac arrest)H&P, check for ACh antibodies (found in 80-90% of MG pts), EMG, CT, MRI 143. Name some medications given for MG Mestinon, prednisone, Imuran, Cytoxin etc. 144. What is the could the medical mgmt be for MG? plasmapheresis ( anti-bodies removed; used to trt exacerbations), IV immune globulin, Thymectomy (may have full or partial remission) 145. There are 2 types of crisis in MG, myasthenic(too little anti-cholinergic med, stress, infection or surgery) and cholinergic(too much cholinergic med). How can we determine which type of crisis pt is having? Tensilon test (remember to have atropine readily available) 146. What can we teach our pts with MG? med mgmt, energy conservation techniques(handicap sticker for car), minimize risks of aspiration(plan meals around time when feeling strong, eat soft foods, may need suctioning equipment), prevent ocular manifestations (put tape or patch on eye at night) 147. Can ptosis be corrected with medication? no 148. What is the definition of Guillian-Barre Syndrome (GBS)? acute inflammatory process characterized by varying degrees of motor weakness and paralysis. This usually starts at the bottom of extremities and works its way up 149. What could cause GBS? autoimmune but may come from virus, trauma, or infection 150. What are the s/s of GBS? Ascending weakness, paresthesia, hypotonia, areflexia, bulbar weakness, paralysis of ocular muscles; eventually respiratory paralysis 151. How can GBS be diagnosed? H&P, CFS shows elevated protein, EMG 152. What is the med mgmt for GBS? May need ventilation, IV immunoglobulin, plasmapheresis, ROM, prevent pulmonary emboli (TEDs, SCDs, medication etc.) encourage independence with ADLs 153. Recovery time for GBS is usually several months to a year, but can GBS reoccur? yes 154. What could cause peripheral neuropathies? Vitamin deficiencies, systemic diseases, drug toxicity, infections, trauma, heavy metals, exogenous substances 155. Will analgesics and narcotics help with nerve pain? usually not, tri-cyclic antidepressants are sometimes used for this 156. What medications can be used for RLS? anti-parkinson meds and some antiseizure meds 157. What nerve if affected in trigeminal neuralgia (Tic Douloureux)? the 5th cranial nerve 158. What could cause this? compression of nerve by vein or atrery, herpes, injury to the trigeminal nerve 159. What do pts with this disease try to avoid? temperature extremes, brushing hair & teeth, or touching face 160. Trt for this depends on the amount of pain that is experienced and can be surgical or nonsurgical. What should we teach pts who want to undergo an RFPE (radiofreq. Percutaneous electrocoagulation)? this may cause facial paralysis 161. What nerve is affected in Bell’s Palsy? cranial nerve 7 162. What could be used in the mgmt of Bell’s? predinsone, analgesics, anti-virals, use eye ointments, patches or tape to protect eye, use straws to diminish drooling, use warm compresses to face and facial exercises may help 163. What is Parkinson’s disease? slowly progressing neurologic movement disability eventually leading to disability associated with decrease levels of dopamine 164. What effect will the loss of dopamine have? this results in more excitatory neurotransmitters than inhibitory transmitters. This imbalance affects voluntary mvmt. 165. What are the s/s of PD? the classic triad are tremor, rigidity and bradykinesia. Others include: pill-rolling, mask-like face, dystonia, shuffling gait, stooped posture, excessive sweating, orthostatic hypotension, gastric and urinary retention (constipation), sex dysfunction, depression, sleep disorders 166. How can PD be diagnosed? mostly through s/s. If 2 out of 3 of the classic triad of symptoms are seen or presence of the other multiple s/s, med hx, H&P, neuro exam 167. What are med examples for PD? carbidopa- levidopa, anticholinergics, dopamine agonists, MAOIs, anti-depressants 168. What sx procedures could a PD pt have done as trt? thalamotomy, palliodotomy, deep brain stimulation 169. If pts undergo the deep brain stimulation, can they take anti-parkinson meds in the future? no 170. What is Huntington’s disease (HD)? chronic, progressive, hereditary disease of the nervous system that results in progressive involuntary choreiform mvmts and dementia 171. What does choreiform mvmt mean? dance-like 172. I f a parent has HD, what is the likelihood off their offspring acquiring this? 50% 173. What are the s/s of HD? Choreiform mvmts, intellectual decline, emotional disturbances, facial tic and grimaces, slurred, hesistant, explosive or unintelligible speech, chewing and swallowing difficulties, disorganized gait, incontinence, affected cognitive function, emotional changes 174. What is used to treat HD? antipyschotics and antidepressants 175. What are nsg interventions for HD? maintain safety, emotional-physical-nutritional (may need 4000-5000kcal/d) support, treat symptoms 176. What is Alzheimer’s disease? chronic, progressive, degenerative brain disorder accompanied by profound effects on memory, cognition, and ability of self-care Know these for Alzh 10 Warning Signs • • • • • • • • • • 1. Memory loss 2. Difficulty performing familiar tasks 3. Problems with language 4. Disorientation to time and place 5. Poor or decreased judgment 6. Problems with abstract thinking 7. Misplacing things 8. Changes in mood or behavior 9. Changes in personality 10. Loss of initiative Alzheimer’s Disease symptoms Normal age-related memory changes Forgets entire experience Forgets part of an experience Rarely remembers later Often remembers later Gradually unable to follow written/spoken direction Usually able to follow written/spoken direction Gradually unable to use notes as reminders Usually able to use notes as reminders Gradually unable to care Usually able to care for for self self 177. What are the durations for the 3 stages of Alzheimers? Stage 1 :(1-3 years) Stage 2: (2-10) years Stage 3: (8-10 years) Review what occurs at each stage..too much to type 178. What would be done in diagnosing a pt with Alzh.? 1ST, R/O Alzh. Through lab work and history, CT and MRI can be done, mini mental status exam (test memory), neuropsychologic testing 179. What meds could be given for Alzh. Pt? Aricept, Namenda, Haldol, Prozac 180. What are the nsg responsibilities for this pt? Maintain safety, help maintain functional ability and personal needs, maintain dignity, reduce anxiety, provide socialization and adequate nutrition, improve communication and educate on home and community assistance.(Try to keep environment the same, pt may need written instructions, don’t overwhelm them with visitors) 181. What occurs to cause amyotropic lateral sclerosis? (ALS or Lou Gehrig’s Disease) basically loss of motor neurons. The body deteriorates but the brain is still intact 182. ALS is characterized by atrophy of the hands, forearms, and legs, paralysis and eventually death. What are the early s/s? fatigue while talking, tongue atrophy, dysphagia, dysarthria, weakness of hands and arms, nasal quality to speech, muscle atrophy, spasticity, fasciculations(quivering) of face, eventually respiratory paralysis 183. How is ALS diagnosed? Based on s/s, MRI, EMG, muscle biopsy(only true way to diagnose this, decrease in motor units seen) 184. What can be done for the care of the ALS pt? may give Riluzole (only med for ALS), pt will need Nsg, RT, PT,OT care, palliative care, support groups and counseling, treat for spasticity.