Steroids, Osteoporosis, and Prevention
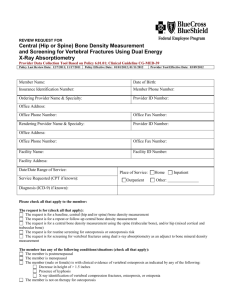
advertisement

Oral Corticosteroids and Osteoporosis Prophylaxis Case: Margaret is a 46-year-old woman with undifferentiated connective tissue disease. She was diagnosed at the age of 44 after having 1 year of polyarticular arthritis, tenosynovitis, and chronic abdominal pain. She had a negative laboratory work-up except a weakly positive SSA titer that was negative on repeat testing. She was started on prednisone 20mg a day with good relief of her symptoms. Over the course of the next year, attempts to wean the prednisone were unsuccessful, despite the addition of low-dose methotrexate. She presents to establish care with her primary care physician on a prednisone dose of 10mg po qd. Margaret, like most patients on long-term oral corticosteroid treatment is at increased risk for osteoporosis. Bone loss in the lumbar spine on high dose therapies can be as high as 27% in the first year of therapy (Reid et al, 1990), although bone loss after this slows to approximately 2-3 times normal bone loss. The pathogenesis of bone loss in corticosteroid-induced osteoporosis is multifactorial. In post-menopausal women, osteoporosis is primarily secondary to increased bone resorption. However, systemic corticosteroids can cause loss of bone density via both reduction in bone formation and increase in bone resorption. Some studies have found that trabecular bone is lost to a greater degree than cortical bone, but this is still in dispute. Factors Contributing to Bone Loss With Corticosteroid Use Reduced Bone Formation Inhibition of osteoblasts Inhibition of IGF-1 production Inhibition of testosterone production Increased apoptosis of osteoblasts and osteocytes Increased Bone Resorption Decrease in intestinal calcium absorption Increased urinary calcium excretion Reduced secretion of sex hormones via inhibition of gonadotropins Possible direct effect on PTH secretion The underlying disease (requiring treatment with corticosteroids) can itself contribute to osteoporosis. For example, persons with diseases as varied as COPD, RA and inflammatory bowel disease have been shown to have lower bone density independent of their exposure to corticosteroids. Interestingly, individuals with RA with well-controlled disease, even those on corticosteroids, will lose less bone than patients with poorly controlled disease (Verhoeven et al., 1997). The most serious consequence of corticosteroid-induced osteoporosis is fracture. Vertebral fractures can cause serious morbidity, including both pain and loss of function. Moreover, hip fractures in postmenopausal women have been associated with significant mortality in the year after fracture. In a retrospective cohort study, 244,235 patients were followed from the initiation of oral corticosteroid therapy to 3 months after cessation of treatment or to initial fracture. Their rates of non-vertebral, vertebral and hip fractures rose along with the daily dose (low dose, <2.5mg a day; medium dose, 2.5-7.5mg a day; high dose, >7.5mg a day): a 20% percent increased risk for those in the low dose group and a 60% greater risk in the high dose group was observed compared to the control group. Interestingly, rate of fracture was much more highly associated with daily dose than cumulative dose of steroids. Also, the rate of fracture approached baseline within 2 years after cessation of corticosteroid treatment (van Staa et al., 2000). Additional history reveals that Margaret has had a hysterectomy but not oophorectomy. She has had no subjective symptoms of menopause to date. She has no family history of osteoporosis. She smokes ½ pack per day, but does not drink alcohol. Should any further work-up be done? Osteoporisis and steroids have been much less extensively studied in premenopausal women. It is known that premenopausal women (and men) lose bone mass while on corticosteroid therapy. In a large study of risedronate vs. placebo in patients taking greater than 7.5 mg of corticosteroid per day, the premenopausal placebo group’s T score dropped 1.2 points in 12 months (Wallach et al., 2000). However, studies to date have not shown fracture in the premenopausal population. A DEXA scan can help to assess a woman’s baseline bone density prior to long-term corticosteroid therapy. The American College of Rheumatology (2001) has recommended getting a baseline DEXA scan in any person in whom corticosteroid treatment duration is anticipated to be greater than 6 months. They suggest follow-up scans as often as 6-12 months. WHO criteria define osteopenia as a T score between –1 to –2.5 and osteoporosis as –2.5. A bone mineral density drop of one standard deviation is generally thought to double the risk of fracture, but this is based on studies of postmenopausal women not on corticosteroids. A few studies have shown that for a similar change in bone mineral density, patients on corticosteroids may have a higher risk of fracture (Luengo et al., 1991, Peel et al., 1995). Thus, the recommended threshold for intervention is also quite low: a T score of –1.5 at the spine or hip from the UK Consensus Group (Eastell et al., 1998) and an even lower T score of –1.0 from the American College of Rhematology (2001). Margaret undergoes a DEXA scan on a Hologic machine. Her bone mineral density at the spine (L1-L4) was 1.0 grams/cm squared. T score at the spine was –0.43 with a Z score of -0.32 (97% of age matched controls). The total hip bone mineral density was 0.794 grams/cm squared with a T score of –1.21 with a Z score of -1.11 (85% of age matched controls). Using the T score at the hip and the Fracture Risk Calculator (Ott, 2003) her estimated lifetime risk of hip fracture is 1.8 times higher than the average woman and her risk of osteoporotic fracture in the next 10 years is 5%. However, given her history of prednisone use and cigarette smoking, her risk increases slightly. She still has a <0.4% chance of a hip fracture in the next 5 years and <8% chance of a non-vertebral fracture. What is the appropriate intervention in Margaret? General measures that reduce risk for osteoporosis or fracture risk include smoking cessation, limiting alcohol consumption, increasing bone-building exercise and limiting fall risk (Yeap et al, 1992, ACR 2001). While these measures have not been specifically addressed in the corticosteroid population, they are low-cost and likely to provide additional health benefits. Calcium is a simple and inexpensive choice for prevention of osteoporosis. There is limited data that calcium alone can help to prevent bone loss, but the majority of studies have demonsrated that calcium plus vitamin D is more effective. Many studies of bisphosphonates and corticosteroids have demonstrated that the “placebo” calcium plus vitamin D maintained bone density (Saag et al., 1998, Reid et al., 2000). A meta-analysis of randomized control trials of long-term oral corticosteroids and bone loss showed that lumbar spine mineral density was 2.0% greater in patients treated vitamin D than with calcium alone or no treatment (Amin et al., 2002). Calcitriol and Vitamin D have both been shown to be effective, but the former can have the side effect of hypercalcemia. Calcitonin is an agent that may increase bone density in patients on extended courses of glucocorticoids, but the evidence is mixed. Some studies have shown little effect on bone density (Sambrook et al, 1993, Healy et al., 1996), but others have shown increased bone density at the lumbar spine but not at the hip (Montemurro et al., 1991, Luengo et al, 1994, and Adachi et al., 1997). A meta-analysis showed that calcitonin increased bone mineral density at the lumbar spine 2.3 percent compared to calcium or therapy in patients on corticosteroids (Amin et al., 2002). However, it has not yet been shown to decrease vertebral fracture risk. Fluoride has been shown to increase bone mineral density in the lumbar spine in persons treated with chronic steroids, but in at least one study it did not prevent loss at the hip (Guaydier-Souquieres et al., 1996, Lems et al., 1997). However, there is some evidence that fluoride can actually increase the risk of fracture in postmenopausal women in spite of the increased bone density (Gutterige et al., 2002). Thus, it is not currently recommended for osteoporosis prevention. Parathyroid hormone has been used successfully in the treatment of refractory osteoporosis and corticosteroid-induced osteoporosis. However, it is extremely expensive, and its role in prophylaxis for corticosteroid-induced osteoporosis is unclear. Replacement of sex hormones has recently become much more controversial. The Women’s Health Initiative Trial showed a significant increase in the risk of stroke, heart disease and breasts cancer in women on hormone replacement therapy (HRT), specifically with estrogen and progesterone (Rossouw et al, 2002). The risk of hip fracture in this postmenopausal population was also reduced. The relative risk of hip fracture was 0.66 (0.45-0.98) and there were 5 fewer hip fractures per 10,000 person years. What is still unclear is how the risks and benefits of HRT might play out in a patient population with a higher risk of hip fracture, such as patients on chronic corticosteroids, and whether or not SERM’s might play a role in older women on steroids. At this point, the best advice is to discuss the risks and benefits with patients. In pre-menopausal women who have oligomenorrhea or amenorrhea, the ACR (2001) recommended considering oral contraceptive pills, based on observational studies of bone loss in young women with menstrual irregularities. In men, hypogonadism can also lead to bone loss, and the ACR (2001) also recommended checking a testosterone level and initiating replacement therapy for levels <300mg/dl in men without contraindications. Bisphosphonates are commonly used in the U.S. for prevention of corticosteroid-induced bone loss. Not only is there data showing increased bone density (compared to calcium and vitamin D) but there is also evidence demonstrating reduced rate of fracture, even in short term studies of bisphosphonate use with corticosteroids. Markers of bone turnover are also consistently lower in the bisphosphonate groups in these trials. A two-year extension study of alendronate use in patients taking 7.5mg prednisone or greater (in addition to vitamin D and calcium) showed a 3.9% (+/-0.7%) increase in bone mineral density at the lumbar spine in the 5mg daily alendronate group. Vertebral fracture rate over the two-year study was only 0.7% in the combined alendronate groups and 6.8% in the calcium plus vitamin D group (p=0.26). There was no significant difference in the number of non-vertebral fractures between groups. There were no premenopausal fractures (Adachi et al., 2001). . Similarly, a randomized trial of risedronate vs. calcium and vitamin D in patients taking 7.5 mg of prednisone or greater showed an increase in vertebral bone density in the risedronate group (1.9 +/- 0.38%) and a loss of bone density in the calcium/vitamin D group over 12 months. Bone mass in the hip was maintained on risedronate. Risk of vertebral fracture was reduced by 70% in the patients taking risedronate 5mg (vs. 2.5mg or placebo, p=0.01). In the group of patients who had started on tcorticosteroid herapy less than 3 months prior to risedronate, there was a trend towards vertebral fracture reduction, 71% (p=0.07). The overall number of fractures was small though. Subgroup analysis did show a significant reduction in fracture in post-menopausal women. Again, no pre-menopausal fractures were observed (Wallach et al., 2000). Cyclical etidrodate has also been shown to be effective in osteoporosis prophylaxis. In a study of patients initiating high dose corticosteroids, bone mineral density of the lumbar spine increased only 0.61% ( +/0.54)over 12 months with q 3 month etidronate infusion , but this was compared to a loss of 3.23% (+/0.60) in the placebo group. Vertebral fractures were significantly reduced by 85% in the postmenopausal subgroup on etidronate (p= 0.5) (Adachi et al., 1997 (2)). A meta-analysis of pooled studies on bisphosphonates calculated a 4.9% increase in bone density versus no therapy or calcium (Amin et al., 2002). Summary of ACR Recommendations for Prevention of Glucocorticoid-induced Ostoeoporosis (Duration of corticosteroid therapy >6months, dose >5mg a day) Smoking cessation Weight bearing exercise Reduction of alcohol consumption Calcium supplementation Vitamin D supplementation Sex hormone replacement if deficient Obtain DEXA scan If T score is less than one: first-line bisphosponate, second-line calcitonin If BMD normal, repeat DEXA in 6 months to 1 year. Adapted from ACR 2001, Table 2 p.1501 A single cost-effectiveness study of corticosteroid-induced osteoporosis has been performed to date. Comparisons were made between no therapy, calcium and vitamin D, etidronate and alendronate (efficacy and cost assumed equal to risedronate) for 4 different age cohorts. Alendronate was more efficacious than etidronate, which was more effective than calcium vitamin D, in reducing fracture number in the 50,60 and 70 year old groups in the 10 year analysis and in the 30,50,60 and 70 year old cohorts in the lifetime analysis. However, the cost was significant. Costs of treatment were balanced against cost of vertebral fracture in disability and actual cost. No treatment was most cost effective for the 30-year-old woman with a T score of 0. Calcium plus vitamin D was most cost-effective in women with T scores of –1 to –2, at a cost of $115 per fracture avoided. Notably, the cost per fracture avoided with alendronate therapy in 50year-old women with a T score of –1 was $121,125. Etidronate was most cost effective in the 70-year-old age group with an estimated T score of –2, at a cost of $838 per fracture avoided. The 70-year-old women treated with alendronate versus etidronate had 5 versus 11 vertebral fractures. However, the cost per fracture avoided rose to over $7,000 (Buckley et al., 2003). Margaret acknowledges her risk of osteoporosis. She agrees to continue calcium and vitamin D supplementation and work on quitting smoking. However, feels she is on a number of medications at present and does not feel compelled to start taking another medication, especially one that has been understudied in pre-menopausal women. She agrees to return in 6 months to 1 year for a DEXA scan. In addition, she has no family history of breast cancer or heart disease, and she may consider at least shortterm estrogen replacement if she becomes symptomatic at menopause. References Adachi JD, Bensen WG, Bell MJ et al. Salmon calcitonin spray in the prevention of corticosteroid-induced osteoporosis. British Journal of Rheumatology 1997; 36:255-259.** Adachi JD, Bensen WG, Brown J et al. Intermittent etidronate therapy to prevent corticosteroid-induced osteoporosis. New England Journal of Medicine 1997; 337(6):382-387. Adachi JD, Saag KG, Pierre DD et al. Two-year effects of alendronate on bone mineral density and vertebral fracture in patients receiving glucocorticoids. Two-year effects of alendronate on bone mineral density and vertebral fracture in patients receiving glucocorticoids: a randomized double-blind, placebo controlled extension trial. Arthritis and Rheumatism 2001; 44(1): 202-211. America Collge of Rheumatology Ad Hoc Committee on Glucocorticoid-Induced Osteoporosis. Recommendations for the preventions and treatment of glucocorticoid-induced osteoporosis. Arthritis and Rheumatism 2001; 44(7):1496-1503. Amin S, Lavalley MP, Simms R et al. The comparative efficacy of drug therapies used for the management of corticosteroid-induced osteoporosis: A meta-regression. Journal of Bone and Mineral Research 2002; 17(8):1512-1526. Blake GM, Fogelman I. Bone densitometry, steroids and osteoporosis. Current Opinion in Nephrology and Hypertension 2002; 11:641-647. Buckley LM, Hillner BE. A cost effectiveness analysis of calcium and vitamin D supplementation, etidronate, and alendronate in the prevention of vertebral fractures in women treated with glucocorticoids. The Journal of Rheumatology 2003; 30:132-137. Eastell R, Reid DM, Compston JE et al. A UK consensus group on management of glucocorticoid-induced osteoporosis: an update. Journal of Internal Medicine 1998; 244:271-292.** Guaydier-Souquieres G, Kotzki PO, Sabatier JP et al. In corticosteroid-treated respiratory diseases, monofluorophosphate increases lumbar spine bone density: a double masked randomized study. Osteoporosis International 1996; 6:171-177. ** Gutteridge DH, Stewart GO, Prince RI et al. A randomized trial of sodium fluoride (60mg) +/- estrogen in postmenopausal osteoporotic vertebral fractures: increased vertebral fractures and peripheral bone loss with sodium fluoride; concurrent estrogen prevents peripheral loss, but not vertebral fractures. Osteoporosis International 2002; 13(2):158-170. Healy JH, Paget SA, Williams-Russo P et al. A randomized controlled trial of salmon calcitonin to prevent bone loss in corticosteroid-treated temporal arteritis and polymalgia rheumatica. Calcified Tissue International 1996; 58:73-80.** Hillel NR. Glucocorticoids and osteoporosis: Pathogenesis and clinical features. Up to Date, 2003. Lems WF, Jacobs JWG, Bijlsma JWJ et al. Is addition of sodium fluoride beneficial in the treatment of corticosteroid induced osteoporosis? Annals of Rheumatic Disease 1997; 7:357-363.** Luengo M, Pons F, Martinez de Oscaba DM. Et al. Preventin of further bone mass by nasal cacitonin in patients on long-term glucocorticoid therapy for asthma: a two year follow-up study. Thorax 1994; 49:1099-1102. ** Luengo M, Picado C, Rio LD et al. Vertebral fractures in steroid dependent asthma and involutional osteoporosis: a comparative study. Thorax 1991; 46:803-806.** Montemurro L, Schiraldi G, Fraiolo P et al. Prevention of corticosteroid-induced osteoporosis with salmon calcitonin in sarcoid patients. Calcified Tissue International 1991; 49:71-76.** Peel NFA, Moore DJ, Barrington NA et al. Risk of vertebral fracture and relationship to bone mineral density in steroid treated rheumatoid arthritis. Annals of Rhematic Disease 1995; 54:801-806.** Reid IR, Heap SW. Determinants of vertebral mineral density in patients receiving long-term glucocorticoid therapy. Archives of Internal Medicine 1990; 150:2545. ** Rosen HN. Glucocorticoids and osteoporosis: Pathogenesis and clinical features. UpToDate, 2003. Rossouw JE, Anderson GL, Prentice RL et al. Risks and benefits of estrogen plus progesterone in healthy postmenopausal women: principal results from the women’s health initiative randomized controlled trial. JAMA 2002; 288(3):321-333. Saag KG, Emkey RS, Brown JR et al. Alendronate for the treatment and prevention of glucocorticoidinduced osteoporosis. New England Journal of Medicine 1998; 39:292-299. ** Sambrook P, Birmingham J, Kempler S et al. Prevention of corticosteroid osteoporosis-- a comparison of calcium, calcitriol and calcitonin. New England Journal of Medicine 1993; 328:1747-1752. ** Van Staa TP, Leufkens HGM, Abenhaim L, et al. Oral corticosteroids and fracture risk: relationship to daily and cumulative doses. Rheumatology 2000; 39:1383-1389. Verhoeven AC, Boers M. Limited bone loss due to corticosteroids; a systemic review of prospective studies in rheumatoid arthritis and other disease. Journal of Rheumatology 1997; 24:1495-1503. ** Wallach S, Cohen S, Reid DM, et al. Effects of risedronate treatment on bone density and vertebral fracture in patients on corticosteroid therapy. Calcified Tissue International 2000; 67:277-285. Yeap SS, Hosking DJ. Management of corticosteroid-induced osteoporosis. Rheumatology 2003; 41:10881094 ** articles for which I have only read abstracts or that were referenced in other articles