Gastro23-GIBleedingCases
advertisement

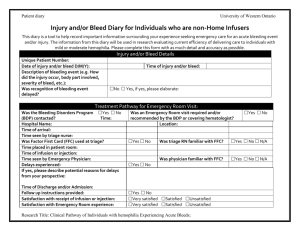
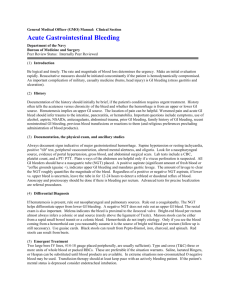
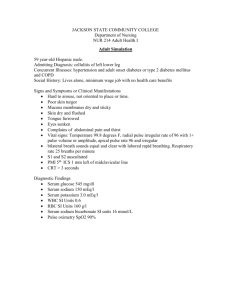
GI #22; Friday, 27th, 2004 10am Dr. Hoang Scott Emerson page1 Lower GI Bleed I. Case Presentation: 62 yo males presents to ER with bright red blood/rectum of one day duration. No abd pain, no nausea nor emesis. ~Initial steps? ~Additional info needed? ~DDX? ~Management of this patient? PMH: Coronary artery dz (ischemic bowel dz), HTN, DM, Prostate CA (radiation tx; radiation proctitis is a common cause of bleeding in this age group) PSH: TURP, Cholecystectomy FmHxt: Father died of colon CA @70yo (has this guy been screened) SoHxt: 20 pack year tobacco, quit 10 yrs ago Meds: ASA 81mg qd, insulin, lisinopril (ask if taking advil, etc. pain meds) Allergy: NKDA ROS: Weakness, dizziness, chest pain (R/O MI) VS: 98.4F, BP 90/50, HR 115, RR 20, O2 sat: 98% on room air HEENT: no epistaxis (nose bleeds can contribute) Hrt: tachy but regular Lungs: clear Abd: +bowel sounds, soft non-tender, non-distended, no peritoneal sign Extremities: cool feet, no cyanosis Neuro: AO3, CN 2-12 intact Rectal: hemorrhoids, +hematochezia (bleeding from lower), 500cc of blood pooled on bed sheets Labs: 1. CBC: ~WBC: 10.2 ~Hb: 9.8 (normaocytic) (actute GI bleed can look normal; takes a day to see changes in Hb; still consider transfusion when <10) ~Hct: 30.1 ~Plt: 255 2. CMP: ~BUN: 22 (pre-renal 20:1 ratio; signs of upper GI bleed, but also from diuretic use or dehydration) ~Cr: 1.1 ~HCO2: 22 3. Coagulation profile: ~PT: 12.3 ~INR:1.2 ~PTT: 32 GI #22; Friday, 27th, 2004 10am Dr. Hoang Scott Emerson page1 *always get coag studies to R/O coagulopathy 4. CK:270 5. Troponin: 0.3 6. EKG> no acute ST-T wave changes Acute abd series: negative Colonoscopy findings: 1. pan-diverticular dz 2. old and small amnt of fresh blood throughout colon, but no obvious sourse of bleeding (tough to see bleed unless streaming out of one area) 3. hemorrhoids 12 hours later, pt. rebleeds with bright red blood. Hemodynamically stable. Repeat Hb: 10.2 (due to receiving 2 units of pRBC/s earlier). Run a nuclear scan or angiography next. His scan was negative (therefore watch/supportive tx; 90% of lower GI bleeds will stop); no recurrent bleeding; Hb stable; diet advanced. Finally discharged home. Had his scan been positive, would have gone to surgery and removed the whole colon (sub-total colectomy) since he had pandiverticular dz. (remove right/left colon depending on if that is where the particular dz is located). Remove colon if continous bleeding and presentations to ER. A. Initial Steps: 1. Triage ~check how sick the pt. is by looking at vital signs ~see if actively bleeding ~tachycardic, hypotensive, alert/awake/obtunded/coma 2. Resuscitate/Stabilize ~if tachycardic and hypotensive: in shock so give them volume, blood ~make sure don't have EKG changes ~give oxygen if not breathing (intubate if needed) ~stabilize first if acute bleeding ~don't do extensive Hxt and PE (only after triaged and stabilized) 3. Determine site of bleeding ~is it upper/lower? ~if someone comes in with bright red blood/rectume and blood all over the sheets (ie. diffuse) and they are tachy and hypotensive; make sure not an upper GI by NG tube and lavage the stomach: if negative then SB source or lower GI bleed. ~Lower GI bleed defined as bleeding below the ligament of Treitz; NG tube and no blood could be a lower GI from right colon GI #22; Friday, 27th, 2004 10am Dr. Hoang Scott Emerson page1 ~Melena usually upper GI but still could be loser B. Additional Info 1. Detailed Hxt and PE 2. Lab data 3. X-ray studies C. Management 1. Dx? Lower GI (could be upper b/c of hemodynamic changes; put in NG tube and if clear (negative) than more than likely a lower (doesn't R/O upper or small bowel b/c could have a pyloric stricture [lesion is post-pyloric but above ligament of Treitz]) 2. Txt options? not answered D. DDX 1. Chart (slide 9) listing the "Common Causes of Lower GI Bleeding" ~Elderly pt most likely is a left diverticular dz ~Most common reason of bleeding is right sided colon dz (thinner mucosa) ~Watershed areas for ischemic colitis are the splenic flexure and recto-sigmoid junction ~Hemorrhoids rare cuase of hemodynamtic changes ~Colon ulcers from CMV, NSAIDs ~Find out if had recent biopsy; invasive proceedure could cause E. Colonoscopy pictures 1. Our guy has diverticular dz with painless lower GI bleeding 2. Thin mucosa with vessel protruding into lumen and spontaneously bleeds F. Slide 14 omited G. Diagnostic Imaging "Procedures Used for Localization of Diverticular Bleeding" 1. After colonoscopy (don't repeat) but do a nuclear scan ~take sample of pt's blood and lable it →put back in →wait →look for accumulation of blood** in an area (if bleeding than see accumulation nuclear activity in that particualr area) 2. Angiography ~in through IMA to look at lower Gi blood distibution to see bleed ~usually don't do unless have a poitive tagRBC scan (b/c detects bleeding at a rate of 0.5cc/min; radionuclide detects at 0.1cc/min GI #22; Friday, 27th, 2004 10am Dr. Hoang Scott Emerson page1 3. Colonoscopy is low yield H. Technetium labled red blood cell scan ~tagged RBC scan to see accumulation of radioactive blood in a particular area; see active GI bleed here ~splenic flexure to localize II. Images A. Angiodysplasia 1. arterio-venous malformation 2. pretty yet dangerous........ 3. abnormal collection of blood vessel B. Ischemic Colitis 1. Left pic's pt. needs surgery 2. Right pic's pt needs supportive care 3. Remember "thumb-printing": mucosal edema of bowel wall C. IBD 1. Difficult to differentiate between IBD and Ischemic Colitis (IC) ~need biopsy ~watershed and other parts of colon fine then IC ~Ulcerative colitis affects rectum ~Crohn's has skip leasions D. Colon CA 1. circumferential and polyploid masses Upper GI Bleed Obscure/Occult GI Bleed Dr. Hoang flew through this last lecture in the last 15 minutes of class…which will explain why some of the blanks aren’t filled in… I. Classification UGI Bleed A. Non-Variceal Bleed (Most Common) 1. Helicobacter pylori 2. NSAIDS B. Variceal Bleed 1. Esophageal 2. Gastric GI #22; Friday, 27th, 2004 10am Dr. Hoang Scott Emerson page1 II. Differential Diagnosis (see slide 3) No need to memorize. III. Most common UGI bleeds are peptic ulcers followed by esophageal/gastric varices IV. Acute Management of Sever Upper GI Bleeding (Same main points as lower GI) A. Resuscitation and stabilization B. Assesment of onset and severity of bleeding C. Diagnostic Endoscopy 1. Preparation of emergent upper panendoscopy 2. Localization and identification of bleeding site 3. Stratification of the risk for rebleeding D. Theraputic Endoscopy 1.Control of active bleeding or high risk lesions 2. Minimization of treatment-related complication 3. Treatment of persistent or recurrent bleeding V. Case 1: 62 BM presents to ER with complaints of diarrhea , black stools of 2 days duration. Vague epigastric pain last 1-2 weeks. No N/V (nausea/vomiting). Initial Impression? Upper GI must still rule out lower GI Next steps? NG tube Triage-Stable? IV acess- 2 sites 18 gauge Labs X ray? Depends on Sx (acute abd n/v, risk of aspiration pneumonia) Focused H&P NGT lavage? VS: BP 130.65 HR 75 RR 16 T 98.7 97% RA Tilt negative A/O x 3 NAD PE: Pale conjunctiva No signs of an acute abdomen Rectal Exam reveals melena (real melena- thick, tar, greasy) With Fe supplements can be slate appearance, dull black Pepto use – can be black, also look at tongue EKG negative NGT Lavage- coffee grounds clear with 700cc H2O (can use normal room temperature tap water, expensive if you use normal saline- all going to stomach anyway, no need to be sterile.) Labs: Hb 7.3, Hct 26.2 Coags normal BUN 54, CR 1.2 X ray- none What next? Stabelize, IV Pepcid (H2 antagonist) [IV PPI not indicated because it will not stop the bleeding, will only help heal ulcer later] GI #22; Friday, 27th, 2004 10am Dr. Hoang Scott Emerson page1 EGD (slide 10) – reveals a duodenal ulcer (5-6 o’clock position) with a clean base, no visible clot →good prognosis EGD with Bx (Bx look for benign Duodenal ulcer- clean base (Most common site for duodenal ulcer with H. pylori, NSAID ulcer most common presentation in the stomach) CLO + (H. pylori related test -Camplobacter Like Organism) GMF vs Tele vs ICU (depends on situation. Active GI bleed →transfer to telemetry.) Risk of re-bleeding ? 3-5% Treatment? EGD Predictors of recurrent Ulcer Hemorrhage Active arterial bleeding → risk of re-bleeding 90% Non-bleeding visible vessel → risk of re-bleed 50% Adherent Clot → Risk of re-bleed 25-30% Clean Ulcer bast → 3-5% Transfusion prior to EGD PPI initially (this “initial” is after scope- IV Pepcid is before EGD) No ASA, NSAIDS Treat for H. pylori Prevpac Helidac (w/ penicillin allergies) PPI QD additional 4 wks after above regimen Consider repeat EGD after treatment – gastric ulcer not heal increase risk for gastric cancer VI. Risk Factors that increase Mortality and morbidity (not emphasized) A. Age older >60 years B. Severe Comorbid medical or surgical illness C. Inpatient Hemorrhage D. Persistent hypotension and shock E. Persistent Hematochezia; red blood emesis or NG aspirate F. Transfusion of 6 or more units RBCs for a single bleed G. rebleeding from the same lesion while hospitalized H. Severe coagulopathy VII. ICU Admit A. No consensus or criteria B. Clinical judgement C. BLEED criteria B= active GI bleed L= Low BP E= elevated coag profile GI #22; Friday, 27th, 2004 10am Dr. Hoang Scott Emerson page1 E= encephalopathy D= Comorbid diseases VIII. AVM (anywhere in GI tract –slide 16) IX. Mallory-Weiss Tear (Erosin below the gastroesophogeal junction, associated with alcoholics or individuals with a large amount of retching) X. Watermelon Stomach (GAVE – Gastric Antro Vasculas Ectasia) Unknown etiology (slide 18) XI. Dieulafoy’s Lesion (rare)- Visible BV without ulceration, BV sticks out and bleeds→inject with epinephrine and cauterize. (slide 19) XII. Case 2: 45 CM Hep C cirrhosis presents to ER with mental status change and bright red emesis. Onset 4 hrs earlier. Unable to obtain hx from patient. What is your impression? Variceal Bleed Next Steps? Triage Hemodynamically stable? Active Bleeding” NGT? Labs/X rays? Blood Products? IV access Airway secured? Elective intubation if in profile to prevent aspiration Focused H&P PMH: Hep C cirrhosis, PUD PSH: EGD 5ya, Appendectomy SoHx: 6 pack/wk, 2 pack year, prior IVDU FmHx: neg Meds: MVI, Folate, Aldactone, Lasix VS: BP 78/35 HR 120 RR 18 94% RA Obtunded NGT Lavage + unable to clear HEENT: Icteric Abd: Distention, ascites Ext: 2mm edema Neuro: obtunded Rectal: Hematochezia Skin: Spider angiomas chest Labs: WBC 4.0, Hb 8.0, Hct 30, Plt 100 BUN 22, CR 1.0, Na 130, AST 210, ALT 102, Tbil 2.0 PT 18, INR 2.0, NH4 95 What next? Stabelize patient Transfuse pRBC’s FFP GI #22; Friday, 27th, 2004 10am Dr. Hoang Scott Emerson page1 Octreotide (variceal bleed) Somatostatin analog 50 mcg IV bolus followed by 50 mcg/hr drip ICU admit Vitamin K 10 mg SQ/IV SBP prophylaxis Emergent EGD EGD – Esophageal Varices (dialated vein ruptures depending upon size) (slide 25-26) EGD with sclerotherapy Actively bleeding esophageal varix Gastric varices- injection Portal HTN gastropathy What is his prognosis? Poor (↑ risk of death) (slide 28) Further treatment needed? Medical therapy Non-selective β-blocker Nitrates (not for mono therapy) Avoid ASA, NSAIDS PPI Endoscopic Therapy EVL- Endoscopic variceal ligation (banding) Sclerotherapy Other TIPS (transjugular intrahepatic portosystemic shunt) Stop ETOH!!! XIII. Case 3: 67 CF with ESRD on HD presents to ER with c/o increasing weakness, fatigue, SOB, intermittent black stool, but on FeSO4 supplements. This is her 4th admission in last 6 mts. Multiple transfusions in past and now has developed a rare blood antibody. It takes 24 hrs to obtain blood for her. PMH: HTN, CAD DM, CRF on HD PSH: Cholecystectomy, EGD x2 negaive, coonoscopy x2 tubular adenoma SoHx: neg FmHx: Non-contributory Meds: ASA, Lisinopril, Glucotrol XL, Amphogel, Calcium, Fe SO4 Occult Bleeding (read through, did not go into any detail) VS: BP 112/73, HR 94, RR 18, 97% RA A/O x3 NAD HEENT- pale conjuctiva HRRR II/VI SEM LSB LCTAB Abd: beingn Ext: 2mm edema LE Rectal: dark brown stool, Heme +++ Labs: GI #22; Friday, 27th, 2004 10am Dr. Hoang Scott Emerson page1 CBC- Hb 7.2, Hct 28, MCV 68, MCH 25 Fe 10, TIBC 247, ferritin 439 CMP- BUN 36, Cr 8.0 Coags normal NGT lavage negative What is your impression? Occult bleeding DDX? (slide 34) did not go over What next? (slide 35) did not go over XIV. Capsule Endoscopy- M2A (mouth to anus pill) Takes picture of small bowel lesions Capsule endoscopy revealed 2 jejunal ulcers.