Tube Thoracostomy - School of Medicine, Queen`s University
advertisement

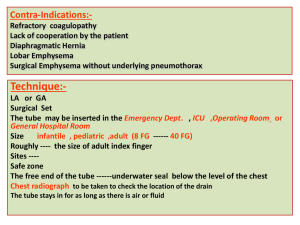
Tube Thoracostomy A Self-Directed Learning Module Technical Skills Program Queen’s University Department of Emergency Medicine Introduction Tube thoracostomy is used to evacuate an abnormal accumulation in the pleural space. The procedure may be performed under emergent or non-emergent conditions. Conditions that may require treatment with a tube thoracostomy include pneumothorax, pleural effusions, empyema or chylothorax. Trauma is a common indication due to accumulations of blood or air in the pleural space. Objectives Describe the indications for a tube thoracostomy Describe the contraindications for a tube thoracostomy Describe the equipment and preparation necessary to perform this procedure Describe the steps for the insertion of a chest tube Describe potential complications of this procedure and relevant prevention and management strategies Indications Emergency Pneumothorax In all mechanically ventilated patients Large or symptomatic pneumothorax Clinically unstable patient (hypotension, increasing O2 requirements) Tension pneumothorax after needle decompression Pneumothorax secondary to chest trauma Hemopneumothorax (e.g. post-trauma) Esophageal rupture with gastric leak into pleural space Non-Emergency Malignant pleural effusion Treatment with sclerosing agents or pleurodesis Recurrent pleural effusions Complex parapneumonic effusion or empyema Chylothorax Post-op care Contraindications Absolute: Published guidelines state there are no absolute contraindications for drainage via tube thoracostomy except when a lung is completely adherent to the chest wall throughout the hemithorax, or upon patient refusal. Relative: Risk of bleeding due to coagulopathies or anticoagulation medications. Whenever possible, coagulopathies and platelet defects should be corrected with the infusion of blood products prior to the procedure. Other relative contraindications include multiple pleural adhesions, emphysematous blebs, and scarring. Equipment These days, most hospitals have presterilized chest tube insertion kits available for use. You should be familiar with the kits at your institution before you are required to use one in an emergency situation. The key materials typically included in these kits are: CSR, wrap #10 scalpel 13x19 inch drape (2) 22-gauge needle (2) #0 suture Crile forceps (2) needle holders (2) non-absorbent towel (4) 4"x4" gauze (10) 10mL syringe (2) 25-gauge needle (1) bag (1) Rochester-Pean forcep (2) cup (2) sponge forcep (1) 18-gauge needle (1) tray (1) dressing scissors (1) tissue forcep (1) Other equipment you will need includes: equipment for universal precautions: gloves, gown, mask and cap chest tube of appropriate size a commercially available pleural drainage system should be ready for connection after the chest tube is inserted with sterile water for water seal local anesthetic adhesive tape- cloth backed hard plastic serrated connectors (only for chest tubes <24Fr, connectors for 24Fr or greater are included in the pleurevac system) The Chest Tube Chest tubes are sized according to internal diameter in the French (Fr) unit. The length of the tube is marked with numbers to indicate distance inserted into the chest wall. Note that they are numbered relative to the the chest, not to the drainage hole on the chest tube. Located at the distal end of the tube are several drainage holes. A radio-opaque stripe runs along the length of the tube and outlines the most proximal drainage hole. This is used to confirm correct placement of the tube in the pleural space on CXR postinsertion. Selecting the Chest Tube Size Generally, chest tubes are No. 24 to 36 Fr for adults and No. 16, 20 24 Fr for children. However, the size of chest tube selected may also depend on the indication for chest tube insertion. The table below provides a summary of size recommendations based on indication. Preparation Check coagulation status and obtain consent for nonurgent tubes. Patients should be started on nasal oxygen and placed on continuous pulse oximetry monitoring. Place the patient in a supine or semirecumbent position with their ipsilateral arm behind their head. Ideally, the head of the bed should be elevated 30 to 60o. This lowers the diaphragm and decreases the risk of injury to the diaphragm, spleen, or liver. The ideal insertion site is approximated by the fourth to fifth intercostal space in the anterior axillary line at the horizontal level of the nipple. This area is within the "triangle of safety" (pictured below), outlined medially by the lateral border of the pectoralis major anteriorly, laterally by the midaxillary line and the 4th to 5th intercostal space inferiorly. The apex of the triangle is located just below the axilla. Note: the nipple line may be an unreliable landmark for the interior border of the triangle in women due to the presence of breast tissue. Always avoid the breast tissue, even in prepubescent girls. Landmark this site by first locating the patient's clavicle. Move your fingers downwards counting the ribs as you go. Once you have located the 4th to 5th intercostal space, move laterally to the anterior axillary line. The INCISION will be made here. The chest tube will actually be inserted one interspace above this point. Mark the incision site. Anesthetizing the Tissues Full barrier precautions must be used during this procedure (sterile gown, gloves, protective eyewear and a face mask). 1. Using antiseptic solution and gauze, create a large sterile field over the marked incision site 2. Cover the field with sterile drapes, leaving the procedure site exposed 3. The skin, subcutaneous tissues, parietal pleura, and periosteum of the rib below the intended insertion site (ie. the rib above the marked incision site) must be adequately anesthetized. Up to 7mg/kg of locally injected 1% lidocaine with epinephrine (1:100,000) can be used (up to 5mg/kg if not using epinephrine). Using a small gauge needle (i.e. >25 gauge), create a wheal of anesthetic in the skin overlying the landmarked spot where the incision will be made. 4. Using the larger gauge needle (i.e. 20-22 gauge), anesthetize the subcutaneous tissues through the wheal, aspirating as the needle moves deeper. 5. Anesthetize the periosteum of the rib that lies below the intercostal space where the tube will be inserted 6. Once you have reached the parietal pleura, a flash of pleural fluid will fill the syringe if a pleural collection is being evacuated. If a pneumothorax is being drained, the syringe may only fill with air. Withdraw the needle, aspirating along the entire path. If air or fluid are not found, the insertion site should be changed. Note: Insertion of a chest tube can be extremely painful, a common error is inadequate local anesthesia; another error is to forget that additional anesthetic may be required throughout the procedure. Incision and Dissection 1. With the scalpel, create a 1.5 to 2cm incision through the skin at the marked incision site 2. With a curved blunt dissecting instrument (e.g. Kelly clamp), dissect the subcutaneous tissues until the intercostal muscle layer is reached 3. Staying on top of the rib to avoid the neurovascular bundle running along the inferior rib margin, guide the blunt dissecting instrument upwards, towards the insertion site. This will create a diagonal path for the chest tube which is thought to provide a better seal against air leaks 4. If using a larger caliber chest tube (24-Fr or greater), use your index finger to explore the tract created by the instrument, this will ensure that the tract will be large enough to accommodate the larger tube 5. Once you have reached the parietal pleura, push the clamp gently through the parietal pleura, you should feel a "give", or a release of resistance. Ensure that adequate local anesthesia is attained prior to proceeding with this step. Alternatively, you may use your finger to advance into the parietal space. Often, pleural fluid may trickle out through the tract 6. Once you have gained access to the pleural space, use your index finger to make sure the lung is not adherent to the pleural wall as this would impede the passage of the tube. If possible, leave your finger in the tract as a guide for the tube 7. Clamp the free end of the tube 8. Using your finger as a guide, pass the tube into the pleural space. This allows you to feel the tube entering the pleural space and avoid subcutaneous dissection with the tube. Some clinicians prefer to pass the tube alone, others recommend that the tube be held in a large curved clamp, with the tube tip protruding from the jaws. Whichever way you choose, it is important to remember that you should NEVER force a tube into the pleural space! 9. If the tube is meant to evacuate a pneumothorax, aim it apically. If the tube is meant to evacuate fluid, aim it basally 10. Make note of the depth of tube insertion via the numbers marked on the tube Securing the Tube 1. Secure the tube to the patient's skin with the heavy sutures using simple interrupted or mattress sutures. Purse string sutures are not recommended due to poor cosmetic results and increased risk of skin necrosis 2. The free ends of the sutures are wrapped around the tube and tied multiple times to secure it in place. It must be tied tight enough so that the tube is slightly kinked, but not so tight as to snap the thread. 3. After securing the tube, wrap the tube with a petroleum based gauze dressing 4. Apply several pieces of sterile gauze cut in a "Ycut" fashion around the tube with the Y-cuts at 90o angles to each other 5. Secure the site with multiple pressure dressings 6. A CXR must be done to ensure the correct placement of the tube. On x-ray: The radiopaque stripe should be visible, with an interruption indicating the placement of the proximal drainage hole, this hole must be within the pleural space If the interruption lies outside the pleural space, the tube is not draining effectively. In this instance, the tube must be removed and replaced altogether. DO NOT ADVANCE THE TUBE INTO THE CHEST! This will introduce nonsterile tubing into the chest cavity Pleural Drainage System Most commercially available pleural drainage systems use the three bottle model of closed drainage and suction. The most important bottle, the underwater seal, serves as a one-way valve that allows air and fluid to leave the pleural cavity without the risk of re-entry during inspiration. Bubbling in this bottle indicates an on-going air leak, either from the patient or from the system itself. The other two bottles typically contained in drainage systems are: the collection bottle, which is connected directly to the patient for accumulation of pleural fluid and/or debris, and a suction system that connects to wall suction but regulates the amount of suction actually delivered to the pleural space via a column of sterile water. The pleural drainage system must be kept approximately 40 inches (100cm) below the level of the patient in order to prevent retrograde flow of air or fluid back into the pleural space. 1. Firmly connect the free end of the chest tube to the sterile drainage system and secure with tape to prevent accidental disconnection 2. Unclamp the free end of the chest tube 3. If pleural fluid is being drained, the fluid level in the drainage system will rise 4. If a pneumothorax is being evacuated, air bubbles will appear in the underwater seal bottle. DO NOT re-clamp the chest tube while there is bubbling as this may lead to recollection of a pneumothorax and may induce a tension pneumothorax 5. Suction may be applied if there is a persistent pneumothorax despite the underwater seal or if a viscous pleural collection is not draining effectively. Usually the suction level is set to 20cmH2O at the Pleurevac 6. To avoid re-expansion pulmonary edema when evacuating chronic large pulmonary effusions, avoid collection of 1.5 L or more within a 30 minute period Complications As with all procedures, there are risks associated with the insertion of a chest tube. You should be familiar with the potential complications associated with chest tube insertion, as well as relevant preventative and management strategies. Self-Assessment Questions Question 1 Which of the following features of pleural drainage systems indicate an active air leak? a. bubbling in the water seal chamber b. bubbling in the collection chamber c. fluctuation of water in the water seal chamber with respirations Question 2 Which of the following is an absolute contraindication to chest tube placement? a. parenchymal scarring b. lung adherent to chest wall throughout the hemithorax c. patient taking anticoagulation medication for greater than 6 months d. patient has stage 4 lung cancer Question 3 Which of the following statements regarding the chest tube is correct? a. chest tubes are sized according to their external diameter in French (Fr) units b. chest tubes sized 28-36 Fr are most appropriate for children c. the radio-opaque stripe runs the length of the tube and outlines the proximal drainage hole d. the radio-opaque stripe runs the length of the tube and outlines the distal drainage hole Question 4 The incision site overlies the rib below the intended insertion site True False Question 5 Choose the INCORRECT statement a. when confirming the correct placement of a chest tube via CXR, the outline of the proximal drainage hole should lie just outside the pleural space b. when evacuating chronic large pulmonary effusions, to avoid re-expansion pulmonary edema do not collect greater than 1.5L within a 30 minute period c. when considering the removal of a chest tube initially placed for a pneumothorax; the patient must be clinically stable, bubbling must have ceased in the air-leak meter, and the lung must be re-expanded on CXR d. in order to remove a chest tube initially placed for pleural fluid drainage; there must be <200cc fluid draining in the last 24 hours and the fluid must be serous Credits Congratulations! You have now completed the Tube Thoracostomy Module. Credits This module was written and developed by Nicole Rocca for the Queen's University Faculty of Health Sciences Patient Simulation Lab. Contributors: Dr. Chris Parker and Dr. Bob McGraw The module was created using exe :eLearning XHTML editor with support from Amy Allcock and the Queen's University School of Medicine MedTech Unit. License This module is licensed under the Creative Commons Attribution Non-Commercial No Derivatives license. The module may be redistributed and used provided that credit is given to the author and it is used for noncommercial purposes only. The contents of this presentation cannot be changed or used individually. For more information on the Creative Commons license model and the specific terms of this license, please visit creativecommons.ca. References 1. Kirsch TD, Mulligan JP: Tube Thoracostomy. In Roberts JR, Hedges JR, et al (eds): Clinical Procedures in Emergency Medicine, 4th ed. Pennsylvania, Elsevier, 2004, p 187-209. 2. Dev SP, Bartolomeu N Jr, Simone C, Chien V. Videos In Clinical Medicine: Chest-Tube Insertion N Engl J Med. 2007;357:e15. 3. The content of this module was based, in part, on a learning guide developed by the Nursing Education Service at Kingston General Hospital.