Millennium and JCI Anesthesia and Surgical Care
Accreditation Standards
September 1, 2008
Introduction
The purpose of this white paper is to present Cerner’s opinions concerning how it believes
Millennium and associated solutions can potentially support the efforts of clients to comply with
many of the standards contained in the Anesthesia and Surgical Care (ASC) section (pp.107-115)
of the 2007 Joint Commission International (JCI) Accreditation Standards for Hospitals, 3rd
Edition (effective January 2008).
The white paper and the information and opinions it contains have not been reviewed or
endorsed in any way by JCI. While every effort was made to ensure the accuracy and
completeness of information in the white paper when it was published, it should be used only for
reference purposes. Interested parties should contact Cerner directly to obtain the most up-todate information concerning solution offerings and functionality, and to discuss how they might
be used to address specific JCI standards.
General Focus of the Standards
The general focus of the accreditation standards in this area can be summarized as follows:
- That operative or other procedures and/or use of moderate or deep sedation/anesthesia are
planned
o Patients subject to such procedures are under pre- and post-operative plans of care
o Patients subject to such procedures are closely monitored
- That care is delivered in an interdisciplinary manner including coordination internally
and externally of resources required for patient care
- Coordination of assessments, procedural care, and post-op orders is planned and executed
throughout the surgical case
- Procedures are appropriate and risks are evaluated throughout the surgical case
Millennium’s Role in Enabling Compliance
The standards found within the Anesthesia and Surgical Care requirements section of the JCI
accreditation standards are focused on the continuous management of sedation and surgical care
delivered to the patient. There are specific requirements around proper assessments being
completed at specific times during each surgical case. There are care planning and
documentation requirements around sedation and patient monitoring of patient status during
procedures which are achieved through PowerPlans and Documentation Management. The
specific requirements around surgical planning, and documentation before, during, and after the
procedure is achieved through the use of PowerPlans and SurgiNet. Post-surgical activities are
scheduled and planned through the system.
The key Millennium solutions involved include:
Cerner Corporation
Confidential Information
©Cerner Corporation. All rights reserved. This document contains confidential and/or proprietary information which
may not be reproduced or transmitted without the express written consent of Cerner.
-
Order Management
PowerPlans
CareNet Documentation Management
INet
eMAR
PowerPOC
Results review
Discern Expert
Patient Management
Patient Privacy
SurgiNet
FirstNet
ProCure
Note: The solutions, solution functionality, and services referenced in this white paper may not
be available in all markets.
At a more granular level, Millennium can assist in enabling compliance with these standards in
the ways described below. (Specific JCI accreditation standards are stated followed by the
abilities of Millennium to enable compliance.) The JCI standards that are highlighted for
comment are those that seem to most directly imply a system role in compliance.
Organization and Management
ASC.1 – Anesthesia services are available to meet patient needs, and all such services meet
applicable local and national standards, laws, and regulations and professional standards.
Anesthesia services meet applicable local and national standards, laws, and regulations.
Adequate, regular and convenient anesthesia services are available to meet patient
needs.
Anesthesia services are available for emergencies after normal hours of operation.
Outside sources are selected based on recommendations of the director, an acceptable
record of performance, compliance with applicable laws and regulations.
If the resources defined for a surgical service or invasive diagnostic imaging service include
pre- and post-op resource as well as the surgical team/package, the system can enable
scheduling of all those resources. The system can help with resource scheduling to assure the
correct equipment, personnel and facilities are available from a patient scheduling standpoint
– and maintain awareness of resource availability.
Surgical system does support documenting surgical assessments in surgical notes. For
invasive diagnostic imaging exams, this is typically limited to what can be documented as a
part of the pre-procedure checklist and is typically documented post procedure through the
Technologist comment field if done in the system at all.
Cerner Corporation
Confidential Information
©Cerner Corporation. All rights reserved. This document contains confidential and/or proprietary information which
may not be reproduced or transmitted without the express written consent of Cerner.
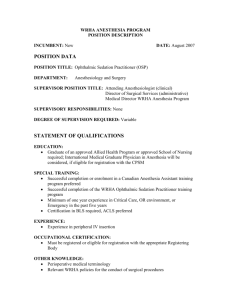
ASC.2 – A qualified individual(s) is responsible for managing the anesthesia services.
Anesthesia services are under the direction of one or more qualified individuals. (Also
see Glossary; GLD 5)
Responsibilities include developing, implementing, and maintaining policies and
procedures.
Responsibilities include administrative oversight.
Responsibilities include maintaining quality control programs.
Responsibilities include recommending outside sources of anesthesia services. (Also see
GLD.3.3, ME 1)
Responsibilities include monitoring and reviewing all anesthesia services.
Individual(s) carries out the responsibilities. (Also see GLD.5.5)
The system does not play a direct role in this requirement other than providing security by
role for who can document and order these types of services.
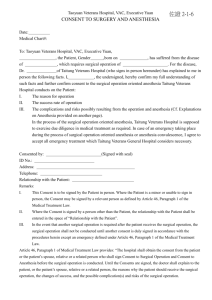
ASC.3 – Policies and procedures guide the care of patients undergoing moderate and deep
sedation.
Appropriate policies and procedures, addressing at least the elements a) through f) found
in the intent statement, guide the care of patients undergoing moderate and deep
sedation. (Also see AOP.2, ME 2 and MMU.4, ME 1)
[NOTE: The following section is from the intent statement.]
Sedation policies identify
a) how planning will occur including the identification of differences between adult
and pediatric populations, or other special considerations;
b) documentation required for the care team to work and communicate effectively;
c) special consent considerations, if appropriate;
d) patient monitoring requirements;
e) special qualifications or skills of staff involved in sedation process; and
f) availability and use of specialized equipment.
The qualified individual(s) identified in ASC.2 participates in the development of the
policies and procedures.
There is a presedation assessment, according to organization policy, to evaluate risk and
appropriateness of the sedation for the patient.
The qualified practitioner responsible for the sedation is qualified in at least elements g)
through k) in the intent statement.
[NOTE: The following section is from the intent statement.]
Sedation policies identify
g) techniques of various modes of sedation;
h) appropriate monitoring;
i) response to complications;
j) use of reversal agents; and
k) at least basic life support.
Cerner Corporation
Confidential Information
©Cerner Corporation. All rights reserved. This document contains confidential and/or proprietary information which
may not be reproduced or transmitted without the express written consent of Cerner.
A qualified individual monitors the patient during sedation and during the period of
recovery from sedation and documents the monitoring.
Moderate and deep sedation are administered according to hospital policy.
See Response to ASC.1.
Surgical system does support documenting surgical assessments in surgical notes. For
invasive diagnostic imaging exams, this is typically limited to what can be documented as a
part of the pre-procedure checklist and is typically documented post procedure through the
Technologist comment field if done in the system at all.
The system can support documentation of sedation/anesthesia administration in surgical
documentation. The system can support documentation of monitoring activities during the
procedure in the same documentation. This can be done through telemetry interfaces with
the medical devices if available, but the actual continuous posting of the telemetry is usually
outside the scope of system use. Any alarms or notifications of possible patient distress
would be a function of the medical devices themselves.
Anesthesia Care
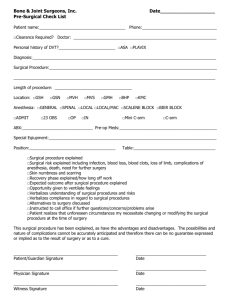
ASC.4 – A qualified individual conducts a preanesthesia assessment and preinduction
assessement.
A preanesthesia assessment is performed for each patient. (Also see AOP.1.1, ME 1)
Patients are re-evaluated immediately before the induction of anesthesia.
The two assessments are performed by individual(s) qualified to do so.
The two assessments are documented in the clinical record (also see Glossary).
Surgical system does support documenting surgical assessments in surgical notes. For
invasive diagnostic imaging exams, this is typically limited to what can be documented as a
part of the pre-procedure checklist and is typically documented post procedure through the
Technologist comment field if done in the system at all. The system can support making
documentation elements required in anesthesia documentation that is present to administer
and monitor anesthesia during the surgical procedure.
ASC.5 – Each patient’s anesthesia care is planned and documented.
The anesthesia care of each patient is planned.
The plan is documented.
Anesthesia may be scheduled as a part of the scheduling of the patient’s surgical procedure,
but structured plans of care are not currently supported by SurgiNet.
Cerner Corporation
Confidential Information
©Cerner Corporation. All rights reserved. This document contains confidential and/or proprietary information which
may not be reproduced or transmitted without the express written consent of Cerner.
System does not directly provide ability to administer plan of care for plans of care in surgery
or invasive procedures – but views the invasive procedure as an order or schedulable
procedure.
For scheduled surgical or diagnostic imaging procedures, the scheduling system can assist
with sequencing of scheduled procedures to help assure that diagnostic testing
is done in the appropriate sequence relative to other activities.
ASC.5.1 – The risks, benefits, and alternatives are discussed with the patient, his or her family,
or those who make decisions for the patient.
The patient, family and decision makers are educated on the risks, benefits, and
alternatives of anesthesia.
The anesthesiologist or another qualified individual provides the education.
The system may be used to capture the documentation of the fact that education was
provided and complications/options discussed.
ASC.5.2 – The anesthesia used and anesthetic technique are written in the patient record.
The anesthesia used is written into the patient’s anesthesia record. (Also see COP.2.1,
ME 6 and MCI.19.1, ME 4)
The anesthetic technique used is written into the patient’s anesthesia record.
This information may be identified as required information for entry as part of the surgical
documentation for the patient’s record.
ASC.5.3 – Each patient’s physiological status during anesthesia administration is continuously
monitored and written in the patient’s record
Physiological status is continuously monitored during anesthesia administration. (Also
see AOP.2, ME 1)
The results of monitoring are entered into the patient’s anesthesia record. (Also see
MCI.19.1, ME 4)
The system can support documentation of sedation/anesthesia administration in surgical
documentation. The system can support documentation of monitoring activities during the
procedure in the same documentation. This can be done through telemetry interfaces with
the medical devices if available, but the actual continuous posting of the telemetry is usually
outside the scope of system use.
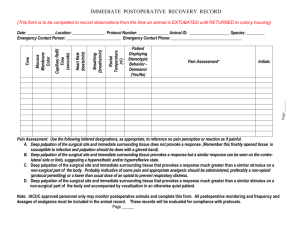
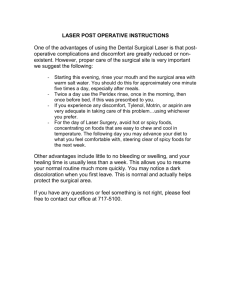
ASC.6 – Each patient’s postanethesia status is monitored and documented, and the patient is
discharged from the recovery area by a qualified individual or by using established criteria.
Cerner Corporation
Confidential Information
©Cerner Corporation. All rights reserved. This document contains confidential and/or proprietary information which
may not be reproduced or transmitted without the express written consent of Cerner.
Patients are monitored appropriate to their condition during the postanesthesia recover
period. (Also see AOP.2, ME 3)
Monitoring findings are entered into the patient’s record. (Also see MCI.19.1, ME 4)
Results of these activities can be documented in surgical documentation.
1. Patients are discharged from the postanesthesia unit in accordance with the alternatives
described in a) through c) found in the intent statement.
[NOTE: the following section is from the intent statement.]
a) The patient is discharged by a fully qualified anesthesiologist or other individual
authorized by the individual(s) responsible for managing the anesthesia services.
b) The patient is discharged by a nurse or similarly qualified individual in
accordance with postanasthesia criteria developed by the hospital’s leaders, and
the discharge is documented in the patient’s record.
c) The patient is discharged to a unit which has been designated as appropriate for
postanesthesia or postsedation care of selected patients, such as a cardiovascular
intensive care unit, neurosurgical intensive care unit, among others.
2. Recovery area arrival and discharge times are recorded.
The discharge criteria used and the arrival and discharge times may be recorded as required
elements of the surgical documentation.
Surgical Care
ASC.7 – Each patient’s surgical care is planned and documented, based on the results of the
assessment.
Each patient’s surgical care is planned.
The planning process considers all available assessment information. (Also see
AOP.1.5.1, ME 1; AOP.5.3, ME 3; and AOP.6.4, ME 3)
Prior to the procedure, a perioperative diagnosis is documented. (Also see MCI.19.1, ME
2)
Prior to the procedure, the planned surgical care is documented.
See response to ASC.5. The assessment information is available to the surgeon and surgical
team as needed, and the planned care and perioperative diagnosis may be captured as
required elements of surgical documentation.
If the resources defined for a surgical service include pre and post op resource as well as the
surgical team/package, the system can enable scheduling of all those resources. The system
can help with resource scheduling to assure the correct equipment, personnel and facilities
are available from a patient scheduling standpoint – and maintain awareness of resource
availability.
Cerner Corporation
Confidential Information
©Cerner Corporation. All rights reserved. This document contains confidential and/or proprietary information which
may not be reproduced or transmitted without the express written consent of Cerner.
ASC.7.1 – The risks, benefits, and alternatives are discussed with the patient and his or her
family or those who make decisions for the patient.
The patient, family and decision makers are educated on the risks, benefits, potential
complications and alternatives related to the planned surgical procedure. (Also see
PFR.6.4, ME 1)
The education includes the need for, risk and benefits of, and alternatives to blood and
blood product use.
The patient’s surgeon or other qualified individual provides the education. (Also see
PFR.6.1, ME 2)
See response to COP.5.1.
There is not a current capability to define consent requirements for procedures or to be aware
of consent requirements at time of scheduling of procedures that may require informed
consent. Consent administration is typically done procedurally, and the appropriate clinical
personnel verify that it has been collected prior to the time of a procedure or an examination
as a part of pre-procedure or pre-surgical checklist processes. Consent forms signed offline
can be scanned in as electronic documents or administered and signed electronically and
associated to the encounter for which the procedure is scheduled or provided. Witnessing
can also be documented through this same means.
ASC.7.2 – The surgery performed is written in the patient record.
A post operative diagnosis is documented.
A description of the surgical procedure, findings and any surgical specimens is
documented. (Also see COP.2.3, MEs 1 and 2)
The names of the surgeon and surgical assistants are documented
The written surgical report, or a brief not in the patient’s record, is available before the
patient leaves the postanesthesia recovery area.
The above elements of surgical documentation can all be defined as required elements in the
system.
ASC.7.3 – Each patient’s physiological status is continuously monitored during and immediately
after surgery and written in the patient’s record.
The patient’s physiological status is monitored continuously during surgery. (Also see
AOP.2, ME 1)
The patient’s physiological status is monitored during the immediate post surgery period.
(Also see AOP.2, ME 1)
Findings are entered into the patient’s record. (Also see MCI.19.1, ME 4)
The system can support documentation of monitoring activities during the procedure in the
same documentation. This can be done through telemetry interfaces with the medical devices
Cerner Corporation
Confidential Information
©Cerner Corporation. All rights reserved. This document contains confidential and/or proprietary information which
may not be reproduced or transmitted without the express written consent of Cerner.
if available, but the actual continuous posting of the telemetry is usually outside the scope of
system use.
ASC.7.4 – Patient care after surgery is planned and documented.
Each patient’s medical, nursing and other post surgical care is planned.
The plan(s) is documented in the patient’s record.
To the extent that the system may support the scheduling of post surgical care activities, the
system can help coordinate the scheduling of such events. The system also may be used to
document the post surgical care plan, but as stated before, the system does not provide a
structured way for surgical care plans to be assigned or ordered. Such activities may be
scheduled or ordered as appropriate, and documented as a part of the surgical documentation.
Cerner Corporation
Confidential Information
©Cerner Corporation. All rights reserved. This document contains confidential and/or proprietary information which
may not be reproduced or transmitted without the express written consent of Cerner.