Adenosine
advertisement

Useful Reference - Antiarrhythmic Meds* S e e
a ls o t e xt 8 3 2 - Ta b 3 6 - 9; 80 5 - t a b 3 5 -8 ; p . 7 4 8 -7 5 1
t a b 3 3 - 8; en t i re c h a rt p ro vi d es s u mm ar y o f fr e que n t l y u se d c a rd i ac m ed s * * N o t n ec es sa r y t o p r in t ,
Class
Action
Drugs: Generic (Trade)
Names
Monitor-Side Effects
Nursing Actions
quinidine (Quinaglute,
Quinidex, Cardioquin)
procainamide
(Pronestyl)
disopyramide
(Norpace)
Decreased
cardiac
contractility
Prolonged QRS,
QT
Proarrhythmic
Hypotension
with IV
administration
Lupus-like
syndrome with
Pronestyl
Anticholinergic
effects: dry
mouth,
decreased urine
output
Observe for HF
Monitor BP with
IV
administration
Monitor QRS
duration for
increase >50%
from baseline
Monitor for
prolonged QT
Monitor N-acetyl
procainamide
(NAPA)
laboratory
values during
procainamide
therapy
IA
Moderate
depression of
depolarization;
prolongs
repolarization
Treats and
prevents atrial and
ventricular
dysrhythmias
Class I-SodiumChannel blockers
IB
Minimal
depression of
depolarization;
shortened
repolarization
Treats ventricular
dysrhythmias
lidocaine (Xylocaine)
mexiletine (Mexitil)
tocainide (Tonocard)
CNS changes
(eg, confusion,
lethargy)
Discuss with
physician
decreasing the
dose in elderly
patients and
patients with
cardiac/liver
dysfunction
IC
Marked
depression of
depolarization;
little effect on
repolarization
Treats atrial and
ventricular
dysrhythmias
flecainide (Tambocor)
propafenone
(Rythmol)
Proarrhythmic
HF
Bradycardia
AV blocks
Discuss
patient's left
ventricular
function with
physician
RNSG 2432 1
II
Decreases
automaticity and
conduction
Treats atrial and
ventricular
dysrhythmias
Class II-B-Adrenergic
blockers (beta blockers)
III
Prolongs
repolarization
Treats and
prevents
ventricular and
atrial
dysrhythmias,
especially in
patients with
ventricular
dysfunction
atenolol (Tenormin)
bisoprolol/HCTZ(Ziac,
Zebeta)
esmolol (Brevibloc)
labetalol (Trandate)
metoprolol (Lopressor,
Toprol)
propranolol (Inderal,
Innopran)
sotalol (Betapace;
Sorine; also has class
III actions)
Bradycardia, AV
block
Decreased
contractility
Bronchospasm
Hypotension
with IV
administration
Masks
hypoglycemia
and
thyrotoxicosis
CNS
disturbances
Monitor heart
rate, PR
interval, signs
and symptoms
of HF
Monitor blood
glucose level in
patients with
type 2 diabetes
mellitus
amiodarone
(Cordarone,
Pacerone)
dofetilide (Tikosyn)
ibutilide (Corvert)
Pulmonary
toxicity
(amiodarone)
Corneal
microdeposits
(amiodarone)
Photosensitivity
(amiodarone)
Hypotension
with IV
administration
Polymorphic
ventricular
dysrhythmias
Nausea and
vomiting
See betablockers
(sotalol)
Make sure
patient is sent
for baseline
pulmonary
function tests
(amiodarone)
Closely monitor
patient
Bradycardia, AV
blocks
Hypotension
with IV
administration
HF, peripheral
edema
Monitor heart
rate, PR interval
Monitor blood
pressure closely
with IV
administration
Monitor for
signs and
symptoms of HF
Class III- Potassium-channel
blockers
IV
Blocks calcium
channel
Treats atrial
dysrhythmias
Class IV Calcium Channel Blockers
Other antidysrhythmic drugs
See text p. 856
2 RNSG 2432
verapamil (Calan,
Isoptin)
diltiazem (Cardizem,
Dilacor, Tiazac, Diltia,
Cartia)
bepridil (Vascor)
Common Cardiac Drugs and Drips (frequently used)
Antiarrhythmics:
-Definition: Drugs that promote normal sinus rhythm; divided into Classes I-V
-Indications: arrhythmias
-Side Effects: QT lengthening, arrhythmias, hypotension, neuro status changes
-Examples:
Adenocard/adenosine: IV
Betapace/sotalol: PO
Cordarone/amiodarone: PO or IV
Corvert/ibutilide: IV
Lanoxin/digoxin: PO, IM, or IV
Pronestyl/procainamide: PO, IM, or IV
Rythmol/propafenone: PO
Xylocaine/lidocaine: IM or IV
Tikosyn: PO
Catecholamines:
-Definition: Stress chemicals, vasopressors; cause increased cardiac output and vasoconstriction
-Indications: shock, hypotension, and increased perfusion
-Side Effects: arrhythmias, tachycardia, nausea, vomiting
-Examples: **BOTH ARE HIGH ALERT MEDICATIONS
Intropin/dopamine: IV
Adrenalin/epinephrine: IV
Chronotropes:
-Definition: Drugs that change the heart rate; positive chronotropes increase the heart rate; negative
chronotropes decrease the heart rate.
-Side Effects: tachycardia, badycardia, palpitations
-Examples:
Atro-Pen/atropine: IV (positive chronotrope)
Dobutrex/dobutamine: IV (mild positive chronotrope)
Lanoxin/digoxin: PO, IM, or IV (negative chronotrope)
Inotropes:
-Definition: Drugs that change power (contractility); positive inotropes increase contractility and increase
cardiac output; negative inotropes decrease ontractility.
-Side Effects: VENTRICULAR ARRYTHMIAS, hypotension
-Examples:
Dobutrex/dobutamine: IV (positive inotrope)
Intropin/dopamine: IV (positive inotrope)
Lanoxin/digoxin: PO, IM, or IV (positive inotrope)
Primacor/milrinone: IV (positive inotrope)
*Most antiarrhythmics are negative inotropes
Beta-Adrenergic Blockers:
-Definition: Drugs that put the heart on bedrest by decreasing heart rate, decreasing contractility, and
decreasing blood pressure; end in “lol.” They competitively block β1-receptors and β2-receptors. β1blockade slows heart rate and decreases cardiac output and contractility. β 2-blockade produces
bronchoconstriction and increased airway resistance (the reason that drugs producing β 2-blockade
should not be used with asthma patients).
-Indications: hypertension, angina pectoris, arrhythmias, migraine headaches, and myocardial infarction (Q
wave)
-Side Effects: bradycardia, hypotension, CHF, pulmonary edema, wheezing
-Examples:
Inderal/propranolol: PO or IV
Lopressor/Toprol XL/metoprolol: PO or IV
Coreg/carvedilol: PO (**also has α-blocking properties—often used with heart failure patients)
Tenormin/atenolol: PO or IV
Calcium Channel Blockers:
-Definition: Drugs that put heart on bedrest by dilating coronary arteries to reduce frequency of angina, dec.
afterload, and suppressing arrhythmias. Relaxes arterial smooth muscle; depresses rate of sinus
node pacemaker slowing AV node conduction and dec. heart rate; produces a neg. inotropic effect.
-Indications: hypertension, angina pectoris, supraventricular tachyarrhythmias
-Side Effects: bradycardia, hypotension, CHF, arrhythmias
-Examples:
Procardia/nifedipine: PO or SL; Calan/verapamil: PO or IV; Cardizem/diltiazem: PO or IV;
Norvasc/Amlodipine: PO
RNSG 2432 3
Ace Inhibitors:
-Definition: Drugs that relax blood vessels throughout the body to lower blood pressure by suppressing the
renin-angiotensin-aldosterone system; decrease afterload in congestive heart failure patients; and
decrease the development of overt heart failure; end in “pril”
-Indications: hypertension, congestive heart failure
-Side Effects: orthostatic hypotension, tachycardia, cough, headache, dizziness
-Examples:
Capoten/captopril: PO; Vasotec/enalapril: PO or IV; Prinivil/Zestril/lisinopril: PO
Accupril/quinapril: PO; Altace/ramipril: PO
Angiotensin II receptor blockers (ARB’s):
-Definition: Drugs that relax blood vessels throughout the body to lower blood pressure by blocking the action of
angiotensin II, an enzyme that is responsible for causing the blood vessels to narrow; end in “sartan”
-Indications: hypertension, congestive heart failure (used in heart failure patients who cannot tolerate ACE
inhibitors due to intractable cough)
-Side effects: headache, dizziness, cough, upset stomach, chills
-Examples:
Cozaar/losartan: PO; Avapro/irbesartan: PO; Diovan/valsartan: PO
Atacand/candesartan: PO
Diuretics:
-Definition: Drugs that enhance the selective excretion of various electrolytes and water to decrease blood
pressure and decrease excess fluid. Decreases peripheral vascular resistance and reduces plasma
volume.
-Indications: hypertension, management of edema, and reduction of increased intracranial pressure
-Side Effects: hyper- and hypokalemia, hyper- and hyponatremia, hypovolemia, orthostatic hypotension, loop
diuretics can cause hypocalcemia
-Examples:
Loop Diuretics: inhibit re-absorption of Na, Cl, and water from the loop of Henle and distal renal
tubule; promote excretion of Na, Cl, K and water
Bumex/bumetanide: PO, IM, or IV
Lasix/furosemide: PO, IM, or IV
Demadex/torsemide: PO or IV
Potassium-Sparing Diuretics: Cause the loss of sodium bicarb and Ca while saving potassium and
hydrogen ions
Aldactone/spironolactone: PO
Thiazide Diuretics: increase excretion of Na, Cl, and water by inhibiting Na reabsortion in the distal
tubule
Diuril/chlorothiazide: PO or IV
HCTZ/hydrochlorothiazide: PO
Osmotic Diuretics: Increases the osmotic pressure of the glomerular filtrate, thereby
inhibiting reabsorption of H2O and electrolytes
Osmitrol/mannitol: IV
Vasodilators:
-Definition: Drugs that dilate blood vessels to decrease blood pressure
-Indications: hypertension, angina pectoris, myocardial infarction
-Side Effects: hypotension, headache, dizziness, edema, facial flushing
-Examples:
Nitrostat/Nitro-Dur/nitroglycerin: SL, PO, IV, transdermal, Buccal
Natrecor/nesiritide: IV; Imdur/isosorbide mononitrate: PO
Isorbid/Isordil/isosorbide dinitrate: SL or PO
Apresoline/hydralazine: PO, IM, or IV; Catapres/clonidine: PO, transdermal, epidural
Anti-Platelet Agents:
-Definition: Drugs that inhibit platelet aggregation to decrease occurrence of atherosclerotic events
in patients at risk
-Indications: thrombus prevention, prevention of acute cardiac ischemic complications, acute coronary
syndrome
-Side Effects: bleeding (esp. GI), edema, anemia, neutropenia
-Examples:
Plavix/clopidogrel: PO; ASA/aspirin: PO
Ticlid/ticlopidine: PO; Aggrastat/tirofiban: IV
Integrilin/eptifibatide: IV
ReoPro/abciximab: IV
Anti-Coagulants:
-Definition: Drugs that prevent thrombus formation
-Indications: thrombus formation (as in myocardial infarction, thrombotic stroke, and deep vein thrombosis),
embolus formation
-Side Effects: Bleeding, anemia, thrombocytopenia
4 RNSG 2432
-Examples:
Lovenox/enoxaprine (low-molecular weight heparin): SQ or IV
Heparin (unfractionated heparin): IV or SQ
Coumadin/warfarin: PO or IV
Fragmin/dalteparin (low-molecular weight heparin): SQ
Lipid-lowering agents:
-Definition: Drugs that affect low-density lipoproteins (LDL’s or “Bad Cholesterol”), high-density lipoproteins
(HDL’s or “Good Cholesterol”), or triglycerides (TG’s)
-Indications: high LDL’s (optimal <100 mg/dL); low HDL’s (optimal >40 mg/dL); high triglycerides (optimal <150
mg/dL)
-Types with Side Effects and Examples:
Statins: lower LDL’s (best drugs for this) and TG’s, raise HDL’s; well-tolerated overall
Side Effects: myopathy, hepatotoxicity, headache, and GI intolerance
Examples:
Lipitor/atorvastatin: PO
Lescol/fluvastatin: PO
Mevacor/lovastatin: PO
Pravachol/pravastatin: PO
Zocor/simvastatin: PO
Bile Acid Sequestrants: lower LDL’s and raise HDL’s; may raise TG’s
Side Effects: GI distress and flatulence, may decrease absorption of other medications
(best to separate from other medication administration)
Examples:
Questran/cholestyramine: PO
Colestid/colestipol: PO
WelChol/colesevelam: PO
Nicotinic Acid: lower LDL’s and TG’s; raise HDL’s (best at this)
Side Effects: rash, flushing, pruritis (best to take with food to prevent or decrease these
very common side effects); hepatotoxicity
Examples:
Niacor/Nicolar (immediate release nicotinic acid): PO
lower risk of hepatotoxicity with this form
Niaspan (extended release nicotinic acid): PO
lower risk of flushing and pruritis with this form
Fibric Acids: lower TG’s (very good at this); lower LDL’s (if TG’s are normal); may raise LDL’s (if TG’s
are elevated)
Side Effects: dyspepsia, myopathy, gall stones
Examples:
Lopid/gemfibrozil: PO
Tricor/fenofibrate: PO
Cardiac Emergency Drugs
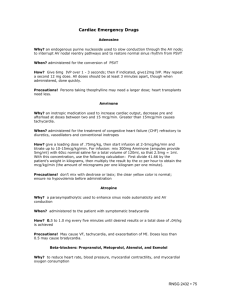
Adenosine (Adenocard)
Why? an endogenous purine nucleoside used to slow conduction through the AV node; to interrupt AV nodal reentry
pathways and to restore normal sinus rhythm from PSVT
When? administered for the conversion of PSVT
How? Give 6mg IVP over 1 - 3 seconds; then if indicated, give12 mg IVP. May repeat a second 12 mg dose. All doses
should be at least 3 minutes apart, though when administered, done quickly.
Precautions! Persons taking theophylline may need a larger dose; heart transplants need less.
Amrinone (Inocor)
Why? an inotropic medication used to increase cardiac output, decrease pre and afterload at doses between two and 15
mcg/min. Greater than 15mcg/min causes tachycardia.
When? administered for the treatment of congestive heart failure (CHF) refractory to diuretics, vasodilators and
conventional inotropes
RNSG 2432 5
How? give a loading dose of .75mg/kg, then start infusion at 2-5mcg/kg/min and titrate up to 10-15mcg/kg/min. For
infusion: mix 300mg Amrinone (ampules provide 5mg/ml) with 60cc normal saline for a total volume of 120ml, so that
2.5mg = 1ml. With this concentration, use the following calculation: First divide 41.66 by the patient's weight in kilograms,
then multiply the result by the cc per hour to obtain the mcg/kg/min (the amount of micrograms per one kilogram per one
minute).
Precautions! don’t mix with dextrose or lasix; the clear yellow color is normal; ensure no hypovolemia before
administration
Atropine
Why? a parasympatholytic used to enhance sinus node automaticity and AV conduction
When? administered to the patient with symptomatic bradycardia
How? 0.5 to 1.0 mg every five minutes until desired results or a total dose of .04/kg is achieved
Precautions! May cause VF, tachycardia, and exacerbation of MI. Doses less than 0.5 may cause bradycardia.
Beta-blockers: Propranolol, Metoprolol, Atenolol, and Esmolol
Why? to reduce heart rate, blood pressure, myocardial contractility, and myocardial oxygen consumption
When? for control of recurrent VT/VF, or rapid supraventricular arrhythmias refractory to other meds
How? Atenolol - 5mg over 5minutes, then repeat in ten minutes. Metoprolol - 5mg over 5 minutes, repeat q 5 minutes to a
total of 15 mg.
Propranolol - 2mg over 2 minutes, q 2 minutes, to a total of 0.1mg/kg.
Precautions! may cause hypotension, CHF and bronchospasm
Calcium Chloride
Why? an element used to increase the force of myocardial contraction
When? administered for treatment of hypocalcemia, hyperkalemia, or calcium channel blocker toxicity
How? Calcium Chloride 10% solution contains 13.6 mEqs (1ml=100mg) of calcium - give 2 to 4mg/kg and repeat as
necessary at ten minute intervals
Precautions! may precipitate digitalis toxicity; precipitates with sodium bicarbonate
Digitalis
Why? a cardiac glycoside used to slow and strengthen myocardial contraction
When? administered for treatment of CHF, PSVT, atrial fibrillation and flutter.
How? a loading dose of 1 mg is divided into several doses and given over a 24 hour period
Precautions! Hypokalemia, hypomagnesemia, and hypercalcemia potentiate digoxin.
Diltiazem (Cardizem)
Why? a calcium channel blocker used to slow conduction and prolong refractoriness in AV node; and to slow the
ventricular response to atrial fibrillation and flutter
6 RNSG 2432
When? administered to patients with PSVT and supraventricular arrhythmias
How? give initial IV push loading dose of 25mg/kg over 2minutes.
IV infusion: mix 125 mg diltiazem (25 ml) into 100cc to yield 1mg/ml, and infuse at 5 - 15mg/hr.
Precautions! Avoid concurrent IV usage with IV betablocker; incompatible with lasix
Dobutamine
Why? to increase myocardial contractility and stroke volume; to decrease peripheral vascular resistance and reduce
ventricular filling pressure.
When? administered for treatment of low cardiac output and hypotension with pulmonary congestion, and left ventricular
dysfunction that can't tolerate vasodilators; for treatment of right ventricular infarction, in addition to moderate volume
loading, to lower preload and afterload.
How? Always dilute before infusion. Mix 500mg into 250cc D5W; with this concentration, calculate using this formula:
First divide 33.3 by the patient’s weight in kilograms, then multiply the result by the cc per hour to obtain the mcg/kg/min.
Dosage range is 2.5 to 10 mcg/kg/min.
Precautions! may cause tachycardias; contains sulfites; greater than 10mcg may cause vasodilation; don’t mix with
heparin, antibiotics, or sodium bicarbonate.
Dopamine
Why? Dopamine is a dose dependent adrenergic (sympathomimetic). Dopaminergic effects: 1-2 mcg/kg/min produce
cerebral, renal and mesoteric vasodilation, increased urine output and no change in heart rate and blood pressure.
Inotropic effects: 2-10mcg/kg/min increases cardiac output and vasoconstriction. Adrenergic effects: more than
10mcg/kg/min increases systemic vascular resistance, heart rate, blood pressure and generalized vasoconstriction.
When? administered for treatment of significant hypotension in the absence of hypovolemia; for treatment of significant
hypotension accompanied with bradycardia; to improve cerebral perfusion immediately post resuscitation; may be
administered in dopaminergic dosages to treat acute renal failure
How? Use the lowest dose which produces adequate perfusion. Always dilute before infusion. Mix 400mg into 250cc
D5W; with this concentration, calculate using this formula: First divide 26.6 by the patient’s weight in kilograms, then
multiply the result by the cc per hour to obtain the mcg/kg/min. Dosage range is 5 - 20 mcg/kg/min.
Precautions! increases heart rate; can exacerbate pulmonary congestion; may induce arrhythmias, nausea/vomiting,
extravasation; is inactivated in alkaline solutions; correct hypovolemia before use
Electricity
Why? Defibrillate to produce temporary asystole, in order to completely depolarize the myocardium, to provide an
opportunity for the natural pacemaker to kick in.
When? administered as soon as possible for pulseless VT and VF; synchronized cardioversion for SVT (supraventricular
tachycardia), atrial fibrillation and flutter
How? Defibrillate up to three times if needed for persistent VT/VF (200J, 200-300J, 360J) with the paddles placed over
the anterior-apex, or anterior-posterior position. Fifty to one hundred joules are administered for synchronized
cardioversion of atrial fib/flutter. Don’t lean on the paddles (they may slide)--apply 25 pounds of pressure. Use the
appropriate conductive material between paddles and person to maximize current flow, and to reduce the potential for
burns and sparking.
Precautions! Ensure all coworkers are clear, or you may have a second patient. Use the chant, "I am going to shock on
three; One, I am clear; Two, you are clear; Three, everybody is clear," to avoid shocking the code team.
Epinephrine
RNSG 2432 7
Why? a catecholamine (sympathomimetic) given to increase heart rate, blood pressure, coronary and cerebral blood flow,
and myocardial electrical activity
When? administered to patients with cardiac arrest from VF, pulseless VT, asystole, PEA (pulseless electrical activity),
and profoundly symptomatic bradycardia
How? IV push : 1mg (10ml of a 1:10,000 solution) every 3-5 minutes during resuscitation.
IV infusion (for symptomatic bradycardia or septic shock) : 1mg (1mL of a 1:1000 solution) in 500cc D5W, so that 1cc =
2mcg, and 1mcg/min is 30cc/hour. Start infusion at 1mcg/minute; titrate from 2 to 10 mcg/minute per hemodynamic
needs.
Precautions! Epinephrine may cause exacerbation of MI (myocardial infarction), ventricular ectopy, hypertension, altered
LOC (level of consciousness) and nausea/vomiting. This drug will cause sloughing of skin and necrosis if infiltrated. Don’t
mix with alkaline solutions.
Furosemide
Why? a potent diuretic that inhibits reabsorption of sodium chloride
When? for treatment of pulmonary congestion associated with left ventricular dysfunction
How? may give 20 to 40 mg IV push over 1 to 2 minutes, up to 2mg/kg total dosage
Precautions! dehydration, deplete calcium, potassium, magnesium, sodium.
Isoproterenol (Isuprel)
Why? Synthetic sympathomimetic amine with potent inotropic (pump) and chronotropic (rate) properties; used to increase
cardiac output, despite its tendency to cause a reduction in mean blood pressure due to venous pooling and peripheral
vasodilation; used to relax bronchial smooth muscle
When? administered for treatment of bradycardia in the denervated heart
How? Always dilute before infusion. Mix 1 mg in 250 cc D5W; so that 4mcg = 1 cc. Dosage: 2 to 10mcg/minute
Precautions! markedly increases myocardial O2 consumption
Lidocaine (Xylocaine)
Why? an antiarrhythmic agent used to decrease automaticity; to suppress ventricular arrhythmias
When? administered as the first antiarrhythmic choice for VT and VF
How? First IV push load with 1 to 1.5 mg/kg. If lidocaine successfully stops the arrhythmia, then start an IV infusion of 2 to
4mg/minute Mix 2 Gms Lidocaine in 250cc, so that 2mg/min = 15cc hour.
Precautions! May cause neurological changes, myocardial and circulatory depression.
Magnesium
Why? an element required for multiple enzymatic reactions
When? administered in the treatment of torsades de pointes; and to reduce postinfarction ventricular arrhythmias
How? for treatment of VT mix 1 to 2 Gms (2-4ml of 50% sol.) in 10cc D5W to run over 1 to 2 minutes; for treatment of VF
give 1 to 2 Gms IV push.
8 RNSG 2432
Precautions! Flushing, sweating, hypotension, mild bradycardia may result from rapid administration. Hypermagnesemia
may produce depressed reflexes, and respiratory paralysis.
Morphine
Why? a narcotic analgesic used to reduce pain and anxiety, to increase venous capacitance and to decrease SVR
(systemic vascular resistance)
When? administered for treatment of pain and anxiety; for treatment of pulmonary edema and MI pain
How? Give 1 to 3mg slow IV push over 1 to 5 minutes
Precautions! Morphine is a respiratory depressant. It may cause hypotension, particularly in hypovolemic persons. Effects
can be reversed with IV naloxone (0.4 to 0.8mg).
Nitroglycerine
Why? a potent vasodilator used to increase blood flow to the myocardium
When? for treatment of unstable angina, myocardial infarction, or CHF.
How? Always dilute before infusion. Mix 50mg NTG in 250cc D5W; with this concentration, use the following formula: { 3.3
multiplied by the cc per hour = mcg/minute}; may titrate by 3.3 mcg (or 1cc) every five minutes, or as indicated by
hemodynamic needs.
Precautions! headache, hypotension
Nitroprusside
Why? a potent peripheral vasodilator used to relax both arterial and venous smooth muscle in order to quickly reduce
blood pressure; decreases both pre and afterload
When? administered for treatment of hypertensive emergencies; during left ventricular failure and pulmonary congestion
How? Always dilute before infusion. Mix 50mg nitroprusside in 250cc; with this concentration, use this calculation: First
divide 3.3 by the patient's weight in kilograms, then multiply the result by the cc per hour to obtain the mcg/kg/min. Wrap
in aluminum foil to reduce light exposure. May be a faint brown color
Precautions! may cause hypotension, myocardial ischemia, infarction, or stroke. Monitor for toxicity with compromised
renal or hepatic functions.
Norepinephrine
Why? a catecholamine used to exert potently positive inotropic and vasopressor control
When? administered for treatment of significant hypotension, and for septic and neurogenic shock
How? Dilute before infusion. IV infusion: Mix 2mg in 250cc to yield 8mcg/ml; so that 2mcg/min = 15cc/hr. The dosage
range is 2 to 80 mcg/minute.
Precautions! may cause severe vasoconstriction, extravasation, arrhythmias, increased myocardial O2 requirements
Oxygen
Why? a drug used to prevent hypoxia/hypoxemia
When? administered to patients with chest pain, hypoxemia and during CPR
RNSG 2432 9
How? 100% FIO2 (fraction inspired oxygen) is administered during CPR. 4L/min is given for O2 sat. (oxygen saturation) >
97% during chest pain. Switch to venturi mask for low O2 sat. Utilize pulse oximetry to monitor adequate delivery.
Precautions! Always ensure oxygen is adequately delivered (mask fits, oxygen connected and turned on, etc).
Procainamide (Pronestyl)
Why? an antiarrhythmic used to suppress ventricular ectopy, and to convert supraventricular arrhythmias or to prevent
their reoccurrence
When? administered to the patient with recurrent VT when lidocaine is ineffective; also administered for conversion and
prevention of SVT
How? The initial bolus is 20-30mg/minute until a total of 17mg/kg is achieved. If indicated, start an IV infusion at 24mg/minute. Mix 2 Gms in 250cc, to yield: 2mg/minute = 15cc/hour
Precautions! Rapid push causes hypotension; watch for widened QRS and seizures.
Sodium Bicarbonate
Why? an alkalinizer used as a buffering agent to neutralize excess acid
When? administered in the treatment of hyperkalemia, tricyclic or phenobarbital overdose, preexisting metabolic acidosis
How? IV push: initial dose 1mg/kg, then half this dosage q 10 minute as indicated; or IV infusion: mix 297.5meq in 500cc
and titrate per ABGs.
Precautions! provokes potent negative inotropic activity; hyperosmolality, and hypernatremia
Thrombolytics
Why? to activate the formation of plasmin, which digests fibrin and dissolves the clot
When? as soon as possible after onset of pain. Indicated for persons with 2 contiguous EKG leads that have ST segment
elevation of at least 0.1mV.
How? Anistreplase - gently mix 5cc sterile water into 30 Unit vial, administer over five minutes and within 30 minutes of
diluting. Streptokinase - gently dilute the 750 thousand or 1,500 thousand Units with 45ml of D5W or NS and infuse over
30 - 60 minutes.
Alteplase - give 10 mg over 2 minutes, then 50 mg over 1 hour, then 20 mg over the second hour, and 20 mg over the
third hour for a total dose of 100 mg over three hours.
Precautions! bleeding from punctures; chest pain, reperfusion arrhythmias
Verapamil (Calan)
Why? a calcium channel blocker; slow conduction and prolong refractoriness in the AV node; also slow ventricular
response to atrial fibrillation and flutter
When? administered to patient with PSVT and supraventricular arrhythmias
How? Give 2.5 to 5mg IV push over 1 to 2 minutes. If inadequate, give 5 mg every fifteen minutes until desired response
is achieved or a total of 30 mg is administered.
Precautions! may cause hypotension; avoid usage with patients demonstrating a wide QRS tachycardia, unless known to
be supraventricular.
10 RNSG 2432