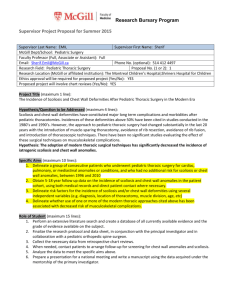
Review of the Literature: Non-operative Scoliosis Treatment
advertisement

Review of the Literature: Non-operative Scoliosis Treatment By Marc Lamantia M.S. D.C.,DACNB Progression and Protocols : Without intervention, Adolescent idiopathic scoliosis (AIS) is a condition which is likely to progress between the time of detection and the time of skeletal maturity.1 This makes early detection, with the intent of early intervention of paramount importance to the success of a non-surgical treatment regiment.2 Unfortunately, the current medical standards recommend observation until a curvature has shown progression of five (5) degrees or more, and the measurement exceeds thirty (30) degrees. This leaves a very small window where brace treatment is suggested, and more importantly lessens the patients’ chances of successful non-surgical treatment. Studies confirm, as the curvature increases, the likelihood of further progression increases as well. 3 Therefore, the current standards are not congruent with the scientific observations reported in these studies. Early intervention should be coupled with early detection. Nachemson et al 4 reported both girls and boys between the ages of ten (10) and twelve (12), who had at least a thirty (30) degree curvature at the time of detection, have the highest risk of progression before skeletal maturity, approaching 100%. If this is in fact accurate, recommendations of early screening and early intervention until the patient reaches skeletal maturity make the most sense. Unfortunately, the pediatric orthopedic community continues to recommend watchful waiting, often waiting until surgery is the only option. Although the highest risk of progression is clearly between the time of detection and skeletal maturity, a second significant progression has been reported to occur between skeletal maturity and a thirty (30) year follow-up.5 In a longitudinal study, Weinstein et al (1981) followed one hundred and twenty (120) patients over forty (40) years. The authors reported a high likelihood of adult progression in those patients with thirty (30) degree lumbar and thoracolumbar curvatures at the time of skeletal maturity. Thoracic curvatures of fifty (50) degrees or more were also reported to have a high likelihood of progression during this same time frame. This is an important study because it highlights the necessity to treat lumbar curvatures which are thirty (30) degrees or more, even when progression is not suspected. Although bracing alone has been the only accepted medical standard since 1951, as of 1984, there had not been any prospective or randomized clinically controlled studies to demonstrate its efficacy. In 1984, Miller et al demonstrated insignificant differences between bracing and observation in regards to the natural progression of AIS. 6 Researchers such as Focarile et al (1991) and Goldberg et al (1993) corroborated these findings, and went as far as to recommend discontinuance of screening programs and challenged the usefulness of bracing at all.78 In a 1997 article printed in the Journal of Bone and Joint Surgery, a meta-analysis was performed to evaluate the efficacy of Non- Operative treatment of AIS. Nineteen studies were included in the analysis, with over 1900 participants. Although the findings clearly showed full time bracing (23 hours per day) did in fact significantly alter the natural progression of the disease, current trends continue towards reduced bracing hours and in some cases, no recommendation of bracing at all.9 Furthermore, the type of brace being prescribed was also a significant variable. The Charleston brace was significantly less successful than the Milwaukee brace (64%), however the authors admit difficulties in comparing the cases due to reporting parameter and classifications amongst patient groups. In general, rigid bracing uses three point pressure systems to reduce the lateral deviation of the spine. More recently, the Spinecor Brace has been gaining popularity among non-surgical providers (we have been providing Spinecor in our offices for the past 5 years). Invented in 1992, the brace consists of a fabric bolero designed to help control rib cage positioning, four fabric elastic band and a pelvic belt. The brace is fitted to induce a corrective posture as first described by Dr. Christine Collaird Collaird16. Depending upon curvature location the brace is fitted accordingly. Spinecor is the first dynamic elastic tension brace designed to provide neuromuscular rehabilitation through de-rotation of the rib cage in relation to the shoulder and pelvic girdle. In a study published in the Journal of Pediatric Orthopedics, patients fitted with the Spinecor brace were monitored continuously for two years beyond the weaning period. Of the 172 participants with a definitive outcome, thirty-nine required surgery prior to skeletal maturity and twelve dropped out; 14 patients were weaned out due to positive outcomes and stability prior to skeletal maturity. So the remaining one hundred and one patients observed had a 59.4% success rate, with an additional 10.6% who had progression of more than 6 degrees but did not require surgery. Of the 59.4% who achieved curvature reduction or stabilization, 95.7% maintained the corrections achieved two years prior. Five (5) of the patients continued to improve despite being out of brace for two years. Interestingly, the authors report lumbar curvatures to respond most favorably (83.3%), then thoracolumbar curvatures (69.4%), Thoracic (56.8%) and double curvatures of equal magnitudes being least favorable (42.8%). Furthermore, when initial curvatures measured between 25 and 29 degrees the rate of success was 70.1% as compared to 50.2% success when the curvatures measured from 30-40 degrees. These findings are consistent with findings of others who report early detection and intervention as necessary for the most successful outcomes. Furthermore, these findings are suggestive that Spinecor is more successful than any other brace when the patient begins treatment with curvatures measuring between 25 and 29 degrees. In May 2007, Dr. Gary Deutchman and I presented the first study on the use of Spinecor in adults entitled, A retrospective study of twenty-three adults treated for scoliosis using the Spinecor Orthosis. 10Although adult treatment has been relegated to pain relief, it was our belief that neuromuscular rehabilitation would be a successful approach to reducing spinal deformities in adults as well as children. The patients were separated into three groups based on curvature location. The patients in the "thoracic" group (n = 20) had a mean average change of -5.27 degrees. This is considered by the Scoliosis Research Society to be a borderline significant reduction. The "thoracolumbar" group (n = 3) had a mean average change of -6.0 degrees, and the Lumbar group (n = 15) had a mean average change of -4.40 degrees. A questionnaire survey revealed the adult group to be “extremely satisfied” and would recommend Spinecor to other adults. I should also add, due to the comorbid nature of scoliosis, chronic pain and degenerative joint disease, alterations were made to the brace configurations on a case by case basis. Many of the adults treated were fitted in an extension-type set-up, (often used to treat kyphosis), irrespective of curvature location. After the patients were tolerant of brace wearing, we then switched many to a more conventional “Spinecor” set-up as described by Collaird. Although pain reduction was the most significant finding, this study highlighted the possibility of adult curvatures responding to non-surgical management. In my experience, adults with scoliosis are unaware that anything can be done to help them in regards to curvature or pain reduction. Of course, cosmesis is another consideration, improving posture and outward appearance is oftentimes the motivating factor for adults who seek treatment. Studies performed by Griffet et al indicated gibbosity reduction as a significant outcome of treatment with the spinecor brace.11 Neuromuscular Influences in Idiopathic Cases: Neuromuscular rehabilitation of the posture in both adults and children should include a thorough neurological evaluation of the vestibular system. Studies confirm the presence of vestibular disturbances in scoliosis patients12 which may not resolve without specific rehabilitation techniques. In an article published in the Scoliosis Journal 2007, I reported on my findings of vestibular dysfunction in a population of scoliosis patients.13 Vestibular dysfunction left untreated influences postural tone, in particular extensor musculature activity during dynamic balance. This includes ambulation as well as specific balancing tasks. Studies confirm abnormal activation of extensor musculature during walking in scoliosis patients.14 The authors of this particular study were concerned with post operative changes, but failed to explore possible non-surgical approaches to influencing muscle recruitment patterns. It is my belief, from a clinical standpoint, following a comprehensive evaluation of vestibular function, movement analysis, gait evaluation and the like, patients can be trained to optimize postural muscle synergies through repetitive movement therapy and vestibular rehabilitation. Although vestibular rehabilitation is well accepted, scoliosis care providers rarely offer evaluations and treatment along these lines. Interestingly, the adolescent population with vestibular pathology, are often without symptoms, much in the same way they are typically without pain. On the other hand, the adult population often suffers from dizziness, imbalance, anxiety and vestibular headaches as a direct result of their vestibular disorder, and experience chronic pain syndromes as well. For those who embark on a course of postural rehabilitation for patients, whether it be working on sagital curve restoration, or otherwise, its efficacy will be lessened in the presence of abnormal vestibulospinal function. Treatment of any movement disorder is most effective when vestibular function is robust, as would be the case in any population, adult or adolescent. To date, vestibular rehabilitation, and really any rehabilitation of movement remains controversial in the United States. Imaging for the 21st Century: Since the first spinal x-ray in 1895, the healthcare professions have championed the use of x-ray as the imaging of choice to visualize the spine. Despite its shortcomings: two dimensional rendering of a three dimensional structure and the ill effects of ionizing radiation, radiography has served us well helping to uncover the sometimes grotesque deformities and anomalies which are oftentimes effectively hidden beneath the skin. But let’s face it, using ionizing radiation repeatedly in a female population during the time of rapid proliferation of radiation-sensitive tissues is less than ideal. This is especially concerning to me when I receive x-rays exposed in most orthopedic offices; without sufficient collimation, filtering or breast and gonadal shielding. New technology has emerged and will undoubtedly reduce our need to expose follow-up x-rays. Raster Stereography was introduced many years ago, and is now used extensively in scoliosis management in throughout Europe. Through the use of an optical light scanner and computational models, Raster Stereography software produces a 3 dimensional representation of the spine without using ionizing radiation. The software analyzes 10,000 points on the back, effectively mapping both the sagital and frontal contours of the spine. A recreation of the spinal column is formulated using sophisticated modeling programs, and the end result is for the most part, dead on accurate. In 2008, researchers confirmed it to be both reliable and sensitive to curvature progression during longitudinal studies on scoliosis patients.17 This is very important to us in the Chiropractic profession, as it will allow us in clinical practice to reduce the amount of x-rays necessary throughout a patient’s lifetime. Our offices now boast one of the first Formetric Raster Stereography scanners in the United States. Formetric also include a mechanically driven dynamic footplate which allows for further testing of balance, vestibulospinal function and podiatric function. I truly believe this technology can help to enhance our patient care, as well as our public image as being concerned with the welfare of our young people. Clearly, there is still a need for x-ray in the management of scoliosis, however, its role will diminish as newer imaging technologies like these become commonplace in Chiropractic practices. Marc Lamantia D.C.,DACNB and Gary Deutchman D.C. are co-founders of Scoliosis Systems LLP. They see patients in 14 locations in 7 states including NY, FL, IL, GA, AZ, CA, TX, NC, and CO. For more information visit www.scoliosissystems.com or call 1-800-281-5010 1 Rowe D., Bernstein S., Riddick M., et al. A meta-Analysis of the Efficacy of Non-Operative Treatments for Idiopathic Scoliosis. J Bone Joint Surg 1997: 79-A; 664-74 2 Focarile, F.;Bonaldi, A.; Giarolo, M.;Ferrari, U.; Zilioli,E.; and Ottaviani, C.: Effectiveness of nonsurgical treatment for Idiopathic Scoliosis. Overview of Available Evidence. Spine 1991; 15:395-401 3 Weinstein, S., Zavala, D., Ponseti, I.; Idiopathic Scoliosis. Long-term follow up and prognosis in untreated patients. J. Bone and Joint Surg. June 1981: 63-A:702-712 4 Nachemson, A.,: Lonstein, J. E.; and Weinstein, S. L: Prevalence and Natural History Committee report. Rea dat the Annual Meeting of the Scoliosis Research Society, Denver Colorado, Sept 25, 1982 5 Weinstein, S., Zavala, D., Ponseti, I.; Idiopathic Scoliosis. Long-term follow up and prognosis in untreated patients. J. Bone and Joint Surg. June 1981: 63-A:702-712 6 Miller, J.; Nachemson, A.; Schultz A.: Effectiveness of braces in mild idiopathic scoliosis. Spine 1984; 9:632-635. 7 Focarile, F.;Bonaldi, A.; Giarolo, M.;Ferrari, U.; Zilioli,E.; and Ottaviani, C.: Effectiveness of nonsurgical treatment for Idiopathic Scoliosis. Overview of Available Evidence. Spine 1991; 15:395-401 8 Goldberg, C.;Dowling, F.; Fogarty, E.; and Moore, D.: School Scoliosis screening and the U.S. Preventive Services Task Force. An examination of Long-term results. Orthop. Trans. 1995-1996; 19:590-591 9 Rowe D., Bernstein S., Riddick M., A meta-Analysis of the Efficacy of Non-Operative Treatments for Idiopathic Scoliosis. et al. J Bone Joint Surg 1997: 79-A; 664-74 10 Deutchman, G.; Lamantia M.,; Indelacato J.; Raykhman M.: A Retrospective Study of twenty three adults treated for scoliosis using the Spinecor Orthosis. From 4th International Conference on Conservative Management of Spinal Deformities Boston, MA, USA. 13–16 May 2007 Scoliosis 2007, 2(Suppl 1):S23doi:10.1186/1748-7161-2-S1-S23 11 Griffet et al. Relationship between gibbosity and cobb angle during treatment of idiopathic scoliosis with the spinecor brace. Eur Spine J (2000) 9:516-522 12 Manzoni D, Miele F.Dipartimento di Fisiologia e Biochimica Vestibular mechanisms involved in idiopathic scoliosis (Arch Ital Biol 2002 Jan;140(1):67-80 Universita di Pisa, Via S. Zeno 31, I-56127 Pisa, Italy) 13 Lamantia et al. A retrospective study of thirty six cases of vestibular hypofunction in adolescents with idiopathic scoliosis. Scoliosis Oct 2007. 2(suppl 1):s37. 14 Hopf C, Scheidecker M, Steffan K, Bodem F, Eysel P. Orthopaedic Department, Lubinus Klinik Kiel, Germany Gait analysis in idiopathic scoliosis before and after surgery: a comparison of the preand postoperative muscle activation pattern. Eur Spine J. 1998;7(1):6-11 15 SPINECOR: a new therapeutic approach for idiopathic scoliosis. Coillard C, Leroux MA, Badeaux J, Rivard CH. Research Center, Sainte Justine Hospital, 3175 Côte Ste Catherine, Montreal, Canada. Stud Health Technol Inform. 2002;88:215-7 16 Schulte TL, Hierholzer E, Boerke A, Lerner T, Liljenqvist U, Bullmann V, Hackenberg LRaster stereography versus radiography in the long-term follow-up of idiopathic scoliosis. Department of Orthopedics, Münster University Hospital, Albert-Schweitzer-Strasse 33, D-48149 Münster, Germany. J Spinal Disord Tech. 2008 Feb;21(1):23-8