Safe Injection Practices to Prevent Transmission of Infections to
advertisement

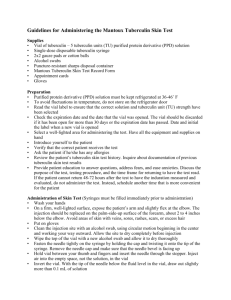
SUBJECT: Infection Control Policy: Safe Practices for Injections, Infusions and Use of Multi-dose Containers REFERENCE NUMBER: K.21-HSM-8370-1010 ORIGIN DATE: 10/10 REVISION NUMBER: REVISION DATES: 1/11, 7/12 MOST RECENT REVIEW DATE: 7/12 PURPOSE: To provide standard guidelines for practicing safe preparation, use and administration of substances that are injected, infused, poured, or topically applied. RESPONSIBILITY: Patient Care Managers CONTACT/CONTENT EXPERT: Director, Infection Prevention & Control Service POLICY: Unsafe and improper injection, infusion and multi-dose vial practices in the healthcare setting result in transmission of bloodborne viruses and other microbial pathogens to patients during routine health care procedures. To prevent microbial contamination of products administered to patients, standard safe practices must be followed. Safe practices are also necessary for administration of topical products, so are included in this policy. DEFINITIONS: PROCESS: The following practices are used during injection, infusion and handling of medication vials: A. Aseptic Technique 1. Perform hand hygiene prior to accessing supplies, handling vials and IV solutions, and preparing or administering medications. 2. Disinfect a. IV ports using friction and 70% alcohol, an iodophor or an approved antiseptic agent. Allow to air dry prior to accessing port. b. Access diaphragm of vials using friction and 70% alcohol. Allow to air dry before inserting a device into the vial. 3. Store and prepare medications and supplies in a designated clean area on a clean surface. 4. Discard all opened vials, IV solutions and prepared or opened syringes that were used in an emergency situation. B. Syringes 1. Remove sterile needle/cannula and/or syringe from package just prior to use. 2. Never store needles and syringes unwrapped as sterility cannot be assured. 2 3. Syringes not pre-filled in an Iso Class 5 Clean Room must be labeled and used within 1 hour of preparation. After 1 hour they must be discarded. 4. Syringes pre-filled inside of the Iso Class 5 Clean Room will have an outdate that must be followed. 5. Never use medication in a syringe for more than one patient even if the needle is changed between patients. 6. Never use a needle for more than one patient. 7. Utilize sharps safety devices whenever possible. Exceptions: a. When teaching patients to give injections for home use. b. When performing a procedure using a fine gauge needle, where the safety feature on the needle/syringe would compromise the technique / quality (e.g. ENT, Dermatology, Podiatry). c. When performing “assembly line” injections where a rigid sharps container is within arm’s reach (e.g. flu clinic, yearly Tuberculin Skin Test). 8. Dispose of used syringes, needles and cannulas at the point of use in an approved sharps container immediately after use. a. Never hand-off a sharp to another person to discard. b. Never lay down a sharp to be picked up and discarded by another person. c. Never put used sharp in your pocket, in the trash, or linen. d. Blunt sutures and needle/syringe systems that retract the needle into the barrel of the syringe are still considered a risk and must be discarded in sharps container. e. It is acceptable to discard needleless syringes in regular waste. 9. Recapping of needles is highly discouraged. When there is no way to avoid it, the one-handed recapping method must be used. a. Tape cap to a horizontal surface. b. Place non-dominant hand behind back. c. Scoop needle into cap. d. Carefully remove from taped surface. 10. For safe disposal of non-safety needle, cover needle with a safety device (e.g. Point Loc) before discarding in sharps container. 11. Do not prepare medication in one syringe to transfer to another syringe, i.e., nurse draws up solution into syringe then transfers the solution to a syringe with plunger removed or injected into the bevel of the syringe to then be injected into the patient. Do not draw solution out of another syringe through a rubber stopper. C. IV Solutions 1. Never use infusion supplies such as needles, syringes, flush solutions, administration sets or intravenous fluids on more than one patient. 2. Once IV solution bags have been spiked, administration must begin within 1 hour. If administration is not begun within 1 hour of spiking the bag, the IV and tubing shall be promptly discarded. For unspiked IV solution bags, follow the pharmacy-prepared or manufacturer- prepared IV solution expiration date. 3. Never use intravenous solution bags to obtain flush solutions, etc. for more than one patient. 4. Use a USP 797 pharmacy clean room (ISO 5) to prepare admixtures of IV solutions. Exception: Administered emergent admixtures (those that cannot 3 be routinely premade or are not anticipated for a case) in Patient Care Units (e.g., ICU), Anesthesia, UCs, and during codes. 5. Routine IV admixtures are compounded in the Pharmacy. For emergent preparation of IV admixture by RN, see: Intravenous Compounding and Admixture in the Patient Care Area. 6. See Addendum A: When to Change or Discard IV Solutions and Tubing. D. Vials 1. Multidose vials a. Use for a single patient whenever possible. b. Date opened multidose vials to reflect discard date. c. Dispose of opened vials 28 days after opening, unless specified otherwise by the manufacturer, or sooner if sterility is questioned or compromised. Exception: Vaccines do not follow 28 date discard. Vaccines follow manufacturer’s outdate. d. Follow manufacturer’s instructions for refrigeration. e. Open vials brought in from patient’s home are strongly discouraged. May be used only in emergency circumstances with Pharmacy’s approval. 2. Single dose vials: use whenever possible and discard immediately after use on a single patient. 3. Ampules: use filter needles to withdraw solution. 4. Before use, a. Check manufacturer’s expiration date. b. Inspect vials for particulate matter, discoloration or turbidity. If present, do not use and discard immediately in Black Box (hazardous waste). 5. Be sure to follow manufacturer’s package insert regarding proper storage and handling of medication. 6. Always use a sterile syringe and needle/cannula when entering a vial. Never one that has been used on another patient. 7. Never store vials in clothing or pockets. 8. Never combine leftover contents of vials for later use. 9. Never leave a needle, cannula, or spike device inserted into a medication vial rubber stopper because it leaves the vial vulnerable to contamination. Exception: Chemotherapy meds because removing spike would cause aerosolization. E. Flushing 1. Each entry into the multidose vial must be with a new unused sterile needle and syringe even if the vial is dedicated to a single patient. 2. Use single-dose containers for flush solutions whenever possible. If a multidose vial must be used, it should be used for only one patient and then discarded. 3. Do not use large volume IV bags to flush solution on multiple patients. F. Multi-use containers/bottles of topical creams, lubricating gels, solutions 1. Use the smallest manufacturer’s container/bottle of cream, gel, topical solution as available, then discard when empty. 2. For topical liquid preparations, use a clean applicator for each entry into the multi-use container. 3. Preservative-free pour bottles of solution (e.g. sterile saline) must be dated and timed upon opening and discarded after 24 hours. 4 4. Never pour from larger container into small container to be used multiple times. 5. It is acceptable to pour solution into small container for immediate use, then discard remainder. 6. Never top off original solution container. Never refill container, as it cannot be adequately cleaned between refills. 7. Remove substance from multi-use tube by squeezing out a small portion and discarding it. Then squeeze out needed amount and recap tube. 8. Remove cream from multi-use container by scooping out desired amount using a clean tongue blade, not fingers, even if gloved. 9. Eye drops in multidose containers are discarded per manufacturer expiration date or sooner if bottle or dropper has contact with a patients eye or becomes contaminated in any manner RELATED DOCUMENTS: Infection Control - Pharmacy KK.01.MH-7080-0900 Methodist Hospital Intravenous Compounding and Admixture in the Patient Care Area Procedure. • Methodist Hospital Intravenous Medication and Syringe Pump Procedure. • USP Chapter 797 standards – Clean room, medium risk level. REFERENCE MATERIALS: 1. Centers for Disease Control. Hepatitis B outbreak in a state correctional facility; MMWR 2001; 50(25):529-523. 2. Massari M, Petrosillo N, Ippolito G et al. Transmission of hepatitis C virus in a gynecological surgery setting. J Clin Micro 2001;39:2860-2863. 3. Centers for Disease Control. Transmission of hepatitis B and C viruses in outpatient settings – New York, Oklahoma, and Nebraska, 2000-2002. MMWR 2003;52(38):901-906. 4. Krause G, Trepka MJ, Whisenhunt RS, et al. Nosocomial transmission of hepatitis C virus associated with the use of multidose saline vials. Infect Control Hosp Epidemiol 2003;24:122-7. 5. Tallis GF, Ryan GM, Lambert SB, et al. Evidence of patient-to-patient transmission of hepatitis C virus through contaminated intravenous anaesthetic ampoules. J Viral Hepat 2003;10:234-9. 6. Comstock RD, Mallonee S, Fox J.L, et. al. A large nosocomial outbreak of hepatitis C and hepatitis B among patients receiving pain remediation treatments. Infect Control Hosp Epidemiol 2004;25(7):576-83. 7. Williams IT, Perz JF, Bell BP. Viral hepatitis transmission in ambulatory health care settings. Clin Infect Dis 2004;38(11):1592-8. 8. Centers for Disease Control. Transmission of hepatitis B Virus among persons undergoing blood glucose monitoring in long-term-care facilities: Mississippi, North Carolina and Los Angeles County, California, 2003-2004. MMWR 2005; 54(09):220-223. 9. Macedo de Oliveira A, et. al. An outbreak of hepatitis C virus infections among outpatients at a hematology/oncology clinic. Anns of Interl Med.2005;142:898-902. 5 10. Samandari T, Malakmadze N, Balter S, et al. A large outbreak of hepatitis B virus infections associated with frequent injections at a physician’s office. Infect Control Hosp Epidemiol 2005;26:745-50. 11. Redd JT, Baumbach J, Kohn W, et al. Patient-to-patient transmission of hepatitis B virus associated with oral surgery. The Journal of Infectious Diseases 2007;195:1311-1314. 12. Centers for Disease Control. Acute hepatitis C virus infections attributed to unsafe injection practices at an endoscopy clinic – Nevada, 2007. MMWR 2008;57(19):513-517. 13. Honoreform. Healthcare-associated outbreaks of hepatitis, 1998-2008. Available at: http://67.228.183.132/~hardtime/HONOR/occurrences.html (Accessed 4/21/2009) 14. Infusion Nursing Standards of Practice. Journal of Infusion Nursing. 2006;29(1S). 15. O'Grady NP, Alexander M, Patchen E, et al. Centers for Disease Control and Prevention. Guidelines for the Prevention of Intravascular Catheter-Related Infections. MMWR 2002;51(No.RR-10). 16. Centers for Disease Control. Guidelines for infection control in dental health-care settings— 2003. MMWR 2003; 52(RR-17):10-1. 17. Guideline for environmental infection control in health-care facilities: recommendations of CDC and the Healthcare Infection Control Practices Advisory Committee. MMWR Control Practices Advisory Committee. MMWR, 2003;52(No. RR-10):1-44. 18. US Department of Labor, Occupational Safety and Health Administration. 29 C.F.R. pt. 1910.1030. Occupational exposure to bloodborne pathogens; needlesticks and other sharp injuries; final rule. Fed. Reg. 2001; 66:5317-25. As amended from and includes 29 C.F.R. pt. 1910.1030. Occupational exposure to bloodborne pathogens; final rule. Fed. Reg. 1991; 56:64174-82. Available at: http://www.osha.gov/SLTC/dentistry/index.html. 19. DeBaun B. Transmission of infection with multi-dose vials. Infection Control Resource. 2005;3(3):1,5-7. Available from: http://www.infectioncontrolresource.org/past.html (Accessed 4/20/2009) 20. Siegel JD, Rhinehart E, Jackson M, et al. and HICPAC. Center’s for Disease Control. Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings 2007. Am J Infect Control 2007;35:S65-S164. 21. Hadaway L. Flushing vascular access catheters: Risks for infection transmission. Infection Control Resource. 4(2):1-8, 2007. http://www.infectioncontrolresource.org/Past_Issues/IC14.pdf (Accessed 4/20/2009) 22. United State Pharmacopeia (USP) 797: Guidebook to Pharmaceutical Compounding – Sterile Preparations. Second Edition, June 1, 2008. 23. Centers for Disease Control. Prevent patient-to-patient transmission of bloodborne pathogens in ambulatory care settings. Available at: http://wwwn.cdc.gov/pubs/hepa.aspx (Accessed 4/20/2009) 24. Centers for Disease Control. Prevent patient-to-patient transmission of bloodborne pathogens in long term care settings. Available at: http://wwwn.cdc.gov/pubs/hepa.aspx (Accessed 4/20/2009) 6 25. Centers for Disease Control. Vaccine storage and handling toolkit. Available at: http://www2a.cdc.gov/vaccines/ed/shtoolkit/pages/inventory_management.htm (Accessed 4/20/09) 26. Grohskopf LA, Roth VR, Feikin DR, et al. Serratia liquefaciens bloodstream infections from contamination of epoetin alfa at a hemodialysis center. N Engl J Med. 2001 May 17;344(20):1491-7. 27. Watson JT, Jones RC, Siston AM, et al. Outbreak of catheter-associated Klebsiella oxytoca and Enterobacter cloacae bloodstream infections in an oncology chemotherapy center. Arch Intern Med. 2005;165:2639-2643. 28. Thompson ND, Perz JD, Moorman AC, Holmberg SD. Nonhospital health care-associated hepatitis B and C virus transmission: United States, 1998–2008. Ann Intern Med. 2009; 150:33-39. NOTE: Combined portions of the Infection Control Practices policy K.07-HSM-8370-0298 with this new policy. COMMITTEE APPROVAL: Infection Control Committee, 10/10. 7 ADDENDUM A: When to Change or Discard IV Solution and Tubing Solution/Tubing P.P.F. (Albumin tubing) Blood tubing after 2 units or every 4 hours (whichever comes first, unless life threatening) Propofol solution & tubing TPN solution, tubing & filter Any IV tubing which is disconnected from the patient for any reason must be changed in a 24 hour period. IV filter (with solution change) Peripheral large volume IV’s when medication is added on the unit Intermittent administration of IV medications Lipid emulsion administration set when units are administered consecutively. Large volume IV’s with medication premixed in Pharmacy Large volume IV’s Peripheral IV tubing including extension set, and electronic infusion devices, running continuously, without interruption. IV medication infusion tubing Peripheral line Y-connector or small bore extension with IV site change Central line Y-connector or small bore extension CADD – pump cassettes Hemodynamic and arterial pressure monitoring (CVP / Swan Ganz), including transducer and/or dome arterial line tubing, premix flush solutions Continuous infusion with CADD – pump cassette Discard/Change Who Every 4 Hours Nurse Every 12 Hours Nurse Every 24 Hours Nurse (Clinics: End of Working Day) Every 48 Hours Nurse Nurse Every 72 Hours IV Therapy IV Therapy or ICU Nurse Every 96 Hours Nurse Every7 Days (Outpatient. & Home Care) IV Therapy or nurse