Posterior Cruciate-Retaining Modular Total Knee Arthroplasty
advertisement

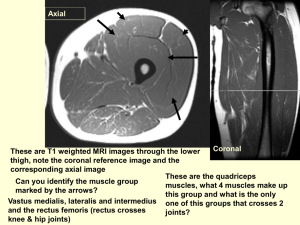
Posterior Cruciate-Retaining Modular Total Knee Arthroplasty: A Nine to Twelve-year Follow-up Investigation Investigation performed at Iowa Methodist Hospital, Des Moines, and the University of Iowa, Iowa City, Iowa. BY GARY B. FETZER, B.S.* JOHN J. CALLAGHAN, M.D.* JESSE E. TEMPLETON, B.S.* DEVON D. GOETZ, M.D.** PATRICK M. SULLIVAN M.D.** SCOTT S. KELLEY M.D.*** *Department of Orthopaedic Surgery, University of Iowa, 200 Hawkins Drive, Iowa City, Iowa 52242. **Des Moines Orthopaedic Surgeons P.C., 6001 Westown Parkway, West Des Moines, Iowa 50266. ***Department of Orthopaedic Surgery, University of North Carolina, Chapel Hill, North Carolina 27599. ABSTRACT Background: There are few intermediate to long-term follow-up investigations of total knee replacements using modular tibial components. This study evaluates the nine to twelve year results of a prospectively followed consecutive series of posterior cruciate-retaining knee replacements with a modular tibial component. Methods: Between November 1988 and January 1991, one author performed 101 total knee arthroplasties in seventy-five patients with the posterior cruciate-retaining press-fit condylar (PFC, Johnson & Johnson, Raynham , Massachusetts) modular total knee arthroplasty. The modular tibial component was metalbacked and the polyethylene tibial insert was the relatively flat, non-conforming posterior-lipped design. The patella was resurfaced with an all-polyethylene three-peg component. All components were fixed with cement. Seventy-eight knees (77%) were performed with an 8.0 millimeter polyethylene insert. The average age at the time of surgery was 71.2 years (range, 52.2 to 88.8 years). There were thirty-one males (forty-two knees) and forty-four females (fifty-nine knees). The patients were evaluated at an average 10.5 years (range, 9.5 to 11.8 years) following the primary total knee arthroplasty. Results: At the time of the final follow-up evaluation, fifty-six patients (seventy-eight knees) were living and nineteen patients (twenty-three knees) were deceased. No patients were lost to follow-up. For the patients who were followed both clinically and radiographically at a minimum of nine years, the average clinical and functional Knee Society ratings were 33 points (range, 3 to 69 points) and 56 points (range, 20 to 80 points) pre-operatively, and 92 points (range, 46 to 100 points) and 79 points (range, 50 to 100 points) at final followup. The average range of motion was from 8 degrees (range, 0 to 30 degrees) to 109 degrees (range, 75 to 125 degrees) pre-operatively, and 1 degree (range, 0 to 10 degrees) to 110 degrees (range, 87 to 130 degrees) at final follow-up. At final follow-up the femoral-tibial angle in the coronal plane was 5 degrees valgus (range, 5 degrees of varus to 10 degrees of valgus). In the deceased patients, no revisions were performed prior to death, and none demonstrated any evidence of radiographic loosening or osteolysis at the most recent followup. In the living patients, the only revision was for aseptic femoral loosening associated with tibial and patellar component polyethylene wear. This revision was performed at 11.1 years following the index 2 procedure when recognized during the patient recall for the present study. There was also one knee with a radiographically loose tibial component (subsided), identified 10.8 years after the index arthroplasty. There were three knees (5%) with proximal tibial osteolysis under the metal-backed tibial tray. There were six knees (10%) with radiographic asymmetric polyethylene wear of at least two millimeters. All six cases with wear were in knees with 8.0 millimeter polyethylene inserts. We found no significant statistical association between the presence of tibial polyethylene wear and gender (p = 1.0), age at time of surgery (p = 0.273), or polyethylene thickness (p = 0.161). Conclusion: At nine to twelve years of follow-up, this cruciate-retaining total knee prosthesis has performed well with excellent clinical and radiographic durability, even with a relatively flat tibial polyethylene articulating geometry. There was a non-significant trend toward increased polyethylene wear with thinner polyethylene inserts. The change to an all-polyethylene patella has also reduced patellofemoral complications in this knee prosthesis. 3 INTRODUCTION Posterior cruciate-retaining total knee replacement has been performed for over twenty years. Modular tibial components were introduced into total knee arthroplasty systems in the mid 1980’s. In order to accommodate the kinematics of the posterior cruciate ligament, most cruciate-retaining designs had relatively flat tibial articulating surfaces with little conformity between the femoral and tibial components. The press-fit condylar (PFC, Johnson & Johnson, Raynham, Massachusetts) posterior cruciate-retaining design followed this approach1,2. In addition, in order to maintain joint line position and preserve proximal tibial bone, relatively thin polyethylene inserts were utilized3,4. The purpose of this study was to evaluate the intermediate to long-term follow-up of the press-fit condylar posterior cruciate-retaining total knee device where this approach was utilized. The authors attempted to answer the following question: What is the durability of a posterior cruciate-retaining device when modular tibial components with relatively flat polyethylene articulating surfaces are utilized? MATERIALS AND METHODS Between November 1988 and January 1991 one author (S. S. Kelley) performed one hundred and one consecutive cemented primary knee arthroplasties with the posterior cruciate-retaining press-fit condylar (PFC, Johnson & Johnson, Raynham, Massachusetts) knee prosthesis (Figure 1). During this time period the surgeon performed seven other total knee arthroplasty procedures. Two posterior-stabilized Insall-Burstein II (Zimmer, Warsaw, Indiana) and four posterior-stabilized press-fit condylar (PFC, Johnson & Johnson, Raynham, Massachusetts) knee prostheses were placed when an insufficient posterior cruciate ligament was identified intraoperatively. One hybrid press-fit condylar (PFC, Johnson & Johnson, Raynham, Massachusetts) arthroplasty, with an in-growth femoral component and a cemented tibial component, was also performed in a young patient. The total study population consisted of one hundred and one knees in seventy-five patients. There were thirty-one males (forty-two knees) and forty-four females (fifty-nine knees). There were fifty-two right knees (51%) and forty-nine left knees (49%). Twenty-six patients (35%) required bilateral knee arthroplasties. The average age at the time of surgery was 71.2 years (range, 52.2 to 88.8 years). The knee diagnosis at the time of surgery was: primary osteoarthritis in eighty-six knees (85%), rheumatoid arthritis in thirteen knees (13%), avascular necrosis in one knee (1%), post-traumatic osteoarthritis in one knee (1%). A previous knee procedure was performed in eleven 4 knees (11%) prior to the index primary total knee arthroplasty. These operations included: six arthroscopies, three meniscectomies, and two patellectomies. The press-fit condylar (PFC, Johnson & Johnson, Raynham, Massachusetts) femoral component was manufactured with a cobalt-chrome alloy and the modular metal-backed tibial tray was titanium. An oval allpolyethylene (ultra-high molecular weight) patellar component with three fixation pegs was utilized in all procedures. The patella was resurfaced in all knees except for two knees in which previous patellectomies had been performed. All components were fixed with cement. The modular posterior-lipped polyethylene tibial insert with minimally raised anterior and posterior borders and a large radius of curvature was utilized in all procedures (Figure 2). During the time interval of these procedures, a more-conforming curved polyethylene tibial insert became available, but was not utilized in these patients. The thickness of the polyethylene tibial insert was 8.0 millimeters (minimum thickness: 5.3 millimeters) in seventy-eight knees (77%), 10.0 millimeters (minimum thickness: 8.0 millimeters) in seventeen knees (17%), 12.5 millimeters (minimum thickness: 10.0 millimeters) in five knees (5%), and 15.0 millimeters (minimum thickness: 13.0 millimeters) in one knee (1%). Beginning in 1991, the manufacturer increased the minimum thickness of the 8.0 millimeter polyethylene tibial inserts from 5.3 to 6.0 millimeters. No knees were performed with this increased minimal polyethylene thickness. The minimum thickness of the other tibial inserts was not changed. The procedure included a long, midline, anterior skin incision, with a medial parapatellar approach into the joint. The anterior cruciate ligament and both menisci were excised. The proximal tibial osteotomy was made at a ninety degree angle to the anatomic axis of the tibia in the anteroposterior plane and was sloped 5 to 10 degrees posteriorly. The distal part of the femur was resected with an attempt to achieve femoral-tibial alignment of 5 to 7 degrees valgus in the coronal plane. Patellar resurfacing was performed after the femoral and tibial osteotomies. Two patients (two knees) required a fifteen degree hemi-wedge prosthesis to be placed beneath the medial aspect of the tibial tray. Both knees had proximal tibial bone defects too large to be simply filled with cement. All components were cemented and cutaneous tissue was closed over J-drains. Operating rooms with vertical laminar airflow were used. Perioperative prophylactic antibiotics were used during all procedures. Post-operatively, patients were immobilized in a bulky dressing. Continuous passive motion was implemented on post-operative day two, and crutch walking with full-weight bearing began on day three. Patients 5 walked with crutches for the first four weeks, and then were allowed to walk with cane support for the next two to four months until they could ambulate unsupported. At the current follow-up, fifty-six patients (seventy-eight knees) were living and nineteen patients (twentythree knees) were deceased. A standardized questionnaire was obtained from patients who returned for clinical and radiographic evaluation. Two authors not associated with the surgery contacted all the living patients to complete a standardized clinical outcome knee questionnaire. Clinical outcomes were calculated based on the Knee Society rating system5. Clinical records were reviewed by one author for documentation of the post-operative course and complications. Radiographic evaluation was performed with standing anteroposterior, lateral, and Merchant view6 radiographs by two authors according to the method described by the Knee Society 7. Radiographs were evaluated for evidence of radiolucencies and osteolysis (at least a five square millimeter area of non-linear bone loss) at the prosthesis-bone interface circumferentially around the three components. Serial radiographs were evaluated for evidence of tibial (asymmetry of tibial thickness greater than two millimeters) and patellar polyethylene wear. The association between gender and tibial polyethylene wear was evaluated by the Fischer’s exact test. A two-sample t-test was performed to evaluate for an association between age at the time of surgery and tibial polyethylene wear. A Wilcoxon rank-sum test was performed to evaluate for an association between polyethylene thickness and the presence of polyethylene wear. A p-value of 0.05 was determined as the level of significance for all statistical outcomes. Kaplan-Meier survivorship analysis was used to determine the probability of component retention 8. Analysis was performed with the clinical endpoint of revision of any component for any reason. Survivorship outcomes were reported with 95% confidence intervals. RESULTS At nine to twelve years following the index procedure, fifty-six patients (seventy-eight knees) were living and nineteen patients (twenty-three knees) were deceased. No patients were lost to follow-up over this time interval. Eleven living patients (fifteen knees) declined radiographic follow-up evaluation because they were medically unable or because they believed they did not need examination. The average age of this patient cohort at this follow-up evaluation was 87.1 years (range, 70.2 to 97.8 years). None of these knees were painful, and the average 6 clinical and functional Knee Society ratings in this cohort was 90 points (range, 62 to 99 points) and 59 points (range, 5 to 85 points), respectively. None of these patients had required a revision for any reason. Of the patients who declined follow-up radiographic evaluation, the average duration of radiographic follow-up was 2.4 years (range, 0.2 to 7.5 years). Radiographs from this cohort revealed very rare radiolucencies, and none had radiographic evidence of component loosening, osteolysis, or polyethylene wear. The nineteen deceased patients (twenty-three knees) had an average clinical follow-up (death) of 7.1 years (range, 2.4 to 10.5 years). All of these patients died of causes unrelated to the index procedure. None of these knees required a prosthesis revision before their death. The average radiographic follow-up in this patient cohort was 2.7 years (range, 0.2 to 7.6 years). Radiolucencies were very rare in this cohort, and there was no radiographic evidence of component loosening, osteolysis, or polyethylene wear. Clinical outcomes of all fifty-six living patients (seventy-eight knees) were evaluated at an average 10.5 years (range, 9.5 to 11.8 years). Forty-five (eighty percent) of the living patients (sixty-three knees, eighty-one percent) were followed clinically and radiographically for an average 10.5 years (range, 9.0 to 11.8 years) following the index procedure. The average age (of the cohort followed clinically and radiographically) at the time of surgery was 67.5 years (range, 52.2 to 83.6 years). The remainder of this report will focus on these patients. The average pre-operative clinical and functional Knee Society ratings in the patients who were followed clinically and radiographically for a minimum of nine years were 33 points (range, 3 to 69 points) and 56 points (range, 20 to 80 points), respectively. The pre-operative femoral-tibial angle in the coronal plane averaged 2 degrees valgus (range, 5 degrees varus to 20 degrees valgus). The pre-operative average range of motion was from 8 degrees (range, 0 to 30 degrees) to 109 degrees (range, 75 to 125 degrees). Clinical examination. For cohort of living patients who were followed clinically and radiographically for a minimum of nine years, the average clinical and functional Knee Society ratings were 92 points (range, 46 to 100 points) and 79 points (range, 50 to 100 points), respectively. The average range of motion was from 1 degree (range, 0 to 10 degrees) to 110 degrees (range, 87 to 130 degrees). All but two knees have maintained maximum flexion of at least ninety degrees. A comparison of the pre-operative and post-operative maximum flexion is summarized in Table 1. The femoral-tibial angle in the coronal plate was 5 degrees valgus (range, 5 degrees of varus to 10 degrees of valgus). 7 At this follow-up evaluation, forty-one knees were not painful, eighteen knees were mildly painful, four were moderately painful, and none were severely painful. Of the patients with knee pain (twenty-two knees), five were start-up pain, fifteen were only painful with long walks, one was painful with short walks, and one knee was painful all the time. In these same twenty-two painful knees, four localized pain to the medial joint line, six to the lateral joint line, one localized pain anteriorly (patellofemoral), and eleven characterized general knee pain. Twenty-nine patients (64%) were taking no medications, while sixteen patients (36%) were using non-steroidal antiinflammatories (NSAIDs). Three patients were taking steroids in addition to non-steroidal anti-inflammatories. No patients were taking narcotics for pain relief. No patients could perform strenuous labor, three could perform moderate strenuous labor, seventeen patients could perform light labor, and twenty-five described themselves as sedentary. Twenty-three patients could walk unlimited distances, thirteen patients could walk for ten to thirty minutes, and nine patients could walk for two to ten minutes before the onset of significant knee pain. Twenty-nine patients required no gait support, nine patients required a cane for long walks, and seven patients required the use of a cane full-time. Sixty knees required no knee brace support, while three knees required use of a knee brace for stability and support. Seven patients could reciprocate stairs without use of the railing, twenty-one could reciprocate stairs with the railing for support, and seventeen patients needed to place both feet on each step. Twenty-one patients could stand from a sitting position without the use of their arms and twenty-four patients could stand with the support of their arms. Thirty-five patients could carry at least ten pounds without difficulty and ten patients could not carry ten pounds. At this final follow-up, forty-five patients (sixty-two knees) reported increased knee function since the index procedure and one patient (one knee) denied increased post-operative function. Forty-five patients (sixtythree knees) reported decreased knee pain since the index procedure. Forty-five patients (sixty-two knees) were satisfied with the results of the index operation, and one patient (one knee) was dissatisfied with the post-operative result. The only patient who reported no increase in function and who was dissatisfied with the post-operative result had suffered a quadriceps muscle rupture secondary to a traumatic fall post-operatively (L3-L4 disc herniation). Radiographic examination. The evaluation of sixty-three knees with a minimum of nine years of radiographic follow-up is summarized in Figure 3. There were no knees with fully circumferential radiolucencies around any of the three components (Figures 4 and 5). In the lateral view of the femoral component, there were thirty-two knees 8 (51%) without any radiolucencies and thirty-one knees (49%) with radiolucent lines in a total of forty-three zones. Twelve knees (19%) had radiolucent lines in two zones. Four of these twelve knees had radiolucent lines in two contiguous zones. No knees had radiolucencies in three or more zones. There were three knees with radiolucent lines greater than or equal to 1 millimeter. Two of these three knees had radiolucent lines in two contiguous zones. There were no knees with radiolucencies around the femoral fixation lugs. No femoral components were loose by radiographic criteria. In the lateral view of the tibial component, there were forty knees (63%) without any radiolucencies and twenty-three knees (37%) with radiolucent lines in a total of twenty-five zones. Two knees had radiolucent lines in two zones. No knees had radiolucencies in contiguous zones. There were two knees with radiolucent lines greater than or equal to 1 millimeter. There were no radiolucencies around the tibial fixation stem. In the anteroposterior view of the tibial component, there were thirty-seven knees (59%) without radiolucencies and twenty-six knees (41%) with radiolucent lines in a total of thirty-four zones. Eight knees had radiolucent lines in two zones. Of the knees with radiolucencies in two zones, five knees had radiolucencies in two contiguous zones. No knees had radiolucencies in three or more zones. There were five knees with radiolucent lines greater than or equal to 1 millimeter. Two of these five knees had radiolucencies in two contiguous zones. There were no radiolucencies observed around the tibial fixation stem. One tibial component was radiographically loose (subsided). There were fifty-eight knees (92%) without patellar radiolucencies and five knees (8%) with a total of six radiolucencies observed in the patellar component. There was one knee with radiolucencies in two non-contiguous zones. All patellar radiolucencies were less than 1 millimeter. No patellar components were loose by radiographic criteria. Patellar subluxation was observed in one knee in Merchant view radiographs. Clinically, the patient had moderate knee pain without effusion, was able to perform stairs by placing both feet on each step without difficulty, and had range of motion from 0 degrees to 120 degrees. The patient was unaware of any patellar instability. There were five patients (six knees, 10%) with at least two millimeters of radiographic evidence of unicompartmental tibial insert polyethylene wear. There were five knees with medial compartment and one knee with lateral compartment wear. In the five knees with medial compartment wear, knee alignment returned to the primary degenerative alignment observed pre-operatively (varus alignment). In the knee with lateral compartment wear, the current valgus alignment was different than the pre-operative degenerative varus alignment. There was 9 one patient with bilateral medial compartment polyethylene wear. Clinical evaluation in four of the six knees demonstrated excellent Knee Society ratings ( 92 points), no apparent effusions or other clinical findings suggestive of polyethylene debris reaction, and maximum knee flexion to at least 110 degrees. One knee (medial compartment wear) was mildly painful, with a significant effusion and a five centimeter cyst on the medial aspect of the knee. Aspiration of the knee was negative for polyethylene or metallic debris. This knee was revised for tibial component polyethylene wear complications. There was also one knee with medial compartment tibial polyethylene wear and evidence of osteolysis under the lateral tibial tray, with tibial component subsidence (discussed later). The primary diagnosis in five of these knees was primary osteoarthritis and rheumatoid arthritis in one knee. The average age (standard deviation) of those with polyethylene wear was 64.8 years (7.0) and those without wear was 68.1 years (7.0). There was no statistically significant association between tibial polyethylene wear and the age of the patient at the time of surgery (two-sample t-test, p = 0.273). Of the six knees with wear, three knees (50%) were in female patients and three knees (50%) were in male patients, while the gender distribution of the fifty-seven knees without wear was very similar, 30 knees (53%) in female patients and 27 knees (47%) in male patients. There was no statistically significant association between the presence of tibial polyethylene wear and gender (Fischer’s exact test, p = 1.0). All of the six knees with wear had tibial polyethylene thickness of 8.0 millimeters. In those without wear, there were forty-two knees (74%) with polyethylene thickness of 8.0 millimeters, ten knees (17%) with 10.0 millimeter, four knees (7%) with 12.5 millimeters, and one knee (2%) with 15.0 millimeters. There was no statistically significant association between the presence of tibial polyethylene wear and the thickness of the tibial insert (Wilcoxon rank-sum test, p = 0.161). There were no knees with radiographic evidence of patellar polyethylene wear. Although, in the only knee that was revised, patellar wear was observed intra-operatively and subsequently revised. There were no knees with evidence of femoral or patellar osteolysis at the final radiographic evaluation. Minimal tibial osteolysis was found in two patients (three knees, 5%). In one patient (two knees), bilateral osteolysis was localized under the medial tibial plateau. In this patient, one knee was asymptomatic with no abnormal clinical findings, and an excellent clinical Knee Society rating (95 points). The contralateral knee was symptomatic and was revised for tibial polyethylene wear complications. Both of these knees these showed radiographic evidence of asymmetric medial compartment polyethylene wear. The other patient had osteolysis under the lateral tibial tray. The tibial component of this knee was radiographically loose and also showed 10 radiographic evidence of medial compartment tibial polyethylene wear. This patient was symptomatic and tibial component revision was recommended (discussed later). Complications. Complications in this series were rare. Manipulation under general anesthesia was performed on three of the one hundred and one knees for stiffness and failure of adequate range of motion in the immediate postoperative period. At the current follow-up, these three knees had excellent Knee Society ratings (91 points) and at least 110 degrees of maximum flexion. One knee suffered a quadriceps muscle rupture secondary to a fall caused by muscle weakness from an L3-L4 disc herniation (4.5 months post-operatively). This was the only knee that required re-operation other than the revision for femoral loosening that was recognized during the patient recall for this study. At this follow-up evaluation, the patient had no knee pain and an excellent clinical Knee Society rating (95 points), but had residual muscle quadriceps weakness. There were two knees with early post-operative patellar instability believed to be secondary to quadriceps muscle atrophy. This instability resolved without intervention, and these knees did not have patellar subluxation at the current follow-up. There was one patient with a post-operative deep venous thrombosis which was successfully treated with anticoagulation. There were no post-operative infections. There have been no patellar fractures in these prostheses. Up until the patient recall for this investigation, no prostheses have been revised for any reason. However, during the current patient recall, two knees were recommended for surgical intervention. The only revision in this series was for complications related to tibial insert polyethylene wear at 11.1 years following the index arthroplasty (Figure 6). At the revision procedure, an aseptically loose femoral component and patellar component polyethylene wear were identified, in addition to the centromedially worn 8.0 millimeter polyethylene tibial insert. The tibial component was mechanically stable and was not revised. There was no radiographic evidence of femoral or tibial component loosening prior to this revision. A new all-polyethylene three-peg patellar component, a 15.0 millimeter tibial polyethylene insert, and a Genesis II revision prosthesis were inserted and cemented. One knee demonstrated probable loosening with medial subsidence of the tibial prosthesis at the time of the patient’s 10.8 year follow-up evaluation. This knee was moderately painful with a poor clinical Knee Society rating (47 points), a tibial-femoral alignment angle of 5 degrees varus, and maximum knee flexion to 110 degrees (as compared to 130 degrees of maximum flexion with an identical contralateral press-fit condylar prosthesis) 11 The survivorship analysis for this series showed excellent results (Figure 7). With revision of any component for any reason as the clinical endpoint, the probability of prosthesis survival was 100% at ten years and 93.3% (95% confidence interval, 0.80-1.00) at twelve years of follow-up, with only one knee revised during the follow-up interval. DISCUSSION The present evaluation of this prospectively followed cohort of modular posterior cruciate-retaining pressfit condylar (PFC, Johnson & Johnson, Raynham, Massachusetts) knee replacements was prompted by the recent concern for backside modular tibial insert wear and the potential for increased wear complications when flat, nonconforming tibial inserts are utilized9-19. The purpose of the current investigation was to report the intermediate to long-term clinical and radiographic outcomes of patients with a cemented cruciate-retaining knee device with a modular metal-backed tibial tray and a relatively flat, non-conforming tibio-femoral polyethylene articulation. Durability in terms of clinical outcomes, radiolucencies, osteolysis, polyethylene wear, and prosthesis survival were evaluated at nine to twelve years. Although similar length of follow-up has been reported with non-modular posterior cruciate-retaining designs20-23, only recently have there been intermediate to long-term follow-up of cruciate-retaining designs with modular tibial trays19,24. One of these studies evaluated modular cruciate-retaining designs which included a metal-backed patellar component that contributed to a relatively high revision prevelance19. Excellent clinical and radiographic results with a low re-operation and complication rate were obtained with this fixed-bearing, modular posterior cruciate-retaining device. Although this patient population was relatively sedentary, the average clinical Knee Society rating was 92 points and ninety-four percent of the knees had only mild or no knee pain. The average functional Knee Society rating of 79 points was similar to that reported in other series’ with an aging patient population19,24. At this length of follow-up, there was excellent maintenance of motion with an average range from 1 degrees to 109 degrees of maximum flexion. Maximum knee flexion of 90 degrees or greater was performed by all except one patient (two knees), whose flexion was 87 degrees. There were six patients (seven knees) with a flexion contracture. One patient (one knee) had a 10 degree flexion contracture and the other five patients (six knees) had a flexion contracture of less than 5 degrees. In comparing the pre-operative to the postoperative range of motion, we found that increased range of motion was mostly the result of improved knee 12 extension (i.e. correction of flexion contracture) rather than increased maximum flexion. There was excellent prosthesis survival rate with this knee device. At ten years of follow-up the probability of prosthesis survival was 100%, and at twelve years of follow-up the probability of prosthesis survival was 93.3% (endpoint defined as revision for any reason), with only one knee requiring revision. Our results with this prosthesis design are comparable to or better than other series’ involving the same modular cruciate-retaining device at a similar length of follow-up. At eight to twelve years of follow-up with the modular posterior cruciate-retaining press-fit condylar device, average Knee Society ratings were 95 to 96 points and range of motion was from 0.3 degrees to 114 degrees19,24. Schai et al. followed 235 modular cruciate-retaining press-fit condylar (PFC, Johnson & Johnson, Raynham, Massachusetts) knees for an average of 10.5 years, and although they reported nineteen component-related revisions, there were no revisions for aseptic loosening. Nine metal-backed patellar components (5% of the metal-backed prosthesis in series) and nine tibial inserts (seven 8.0 millimeter and two 10.0 millimeter, all posterior-lipped design) were revised for wear complications19. One previously unresurfaced patella was also revised. Fortunately, the change to an all-polyethylene patellar component in some of these knees resulted in excellent outcomes with no patellar revisions at follow-up. Overall, with revision as the endpoint, the probability of prosthesis survival was 92% at ten years of follow-up. Buehler et al. followed 108 modular cruciate-retaining press-fit condylar (PFC, Johnson & Johnson, Raynham, Massachusetts) knees for a minimum of eight years24. They reported no component revisions for aseptic loosening, but did report one patellar revision for recurrent dislocation, two revisions for excessive patellar and tibial polyethylene wear (tibial insert thickness not reported, all posterior-lipped design), and one radiographically loose patellar component (not revised). The probability of prosthesis survival at eight to ten years of follow-up was 93.4%. Neither of the above studies reported any osteolysis. Both of these studies involved knee devices where at least some of the procedures involved a metal-backed patella. The results from our study are also comparable or better to those reported with the non-modular posterior cruciate-retaining Kinematic I knee prosthesis25,26. Malkani et al. followed 168 Kinematic I total knee devices for an average of ten years and reported six component-related revisions25. Four revisions were for aseptic patellar component loosening (all-polyethylene, single-peg geometry) and two revisions for aseptically loose femoral and tibial components. There were also two radiographically loose patellar components that were not revised. No polyethylene wear or osteolysis was reported. The probability of prosthesis survivorship at ten years was 96% 13 (revision as the endpoint). In a more recent and much larger series, Ewald et al. followed 539 Kinematic I total knee devices for ten to fourteen years and reported eighteen component-related revisions, including ten revisions for aseptic patellar loosening and two revisions for recurrent patellar subluxation 26. They also reported three revisions for tibial tray fracture, one revision for aseptic femoral loosening, one revision for three-component aseptic loosening with bony resorption, and one revision for peripatellar bony overgrowth causing pain. Polyethylene wear was less of a problem in their series, as they reported only four knees with tibial wear (three were associated with tibial tray fractures). Tibial polyethylene thickness was not reported in these knees. The results are also comparable to series’ involving non-modular posterior cruciate-sacrificing and nonmodular cruciate-substituting designs. Vince et al. followed 130 knees with the non-modular posterior cruciatesacrificing Total Condylar knee device for ten to twelve years, and reported five component-related revisions22. Three revisions were performed for aseptic tibial loosening, one for aseptic femoral loosening, and one was performed for varus instability. No osteolysis or wear complications were reported. Goldberg et al. also followed 153 arthroplasties using the non-modular cruciate-sacrificing Total Condylar knee prosthesis for an average of nine years of follow-up27. Although they reported ten revisions, only seven were component-related. There were six knees revised for aseptic loosening: two knees had tibial component revisions and four knees had femoral and tibial component revisions. There was one revision for posterior instability. The authors did not report any polyethylene wear or osteolysis complications. Stern et al. followed a cohort of 289 total knee arthroplasties using a non-modular posterior-stabilized knee prosthesis for a range of nine to twelve years28. They reported a total of fourteen revisions, with only nine component-related revisions. Three revisions were performed for aseptic femoral loosening and six revisions for aseptic tibial loosening. The probability of prosthesis survival at ten years of follow-up was 95.6%. A significant complication in this series was the rather high prevalence of patellar fractures (seven reported fractures) with this single-peg patellar component. The authors reported no osteolysis or radiographic loosening. At this length of follow-up there was only one revision for wear-related complications and one indicated revision which also was probably related to wear. This was lower then the authors expected with this flat, nonconforming modular tibial insert. The low prevalence may be related to the relatively old patient population and the satisfactory alignment of the knee replacements in this series. It may also be related to the relatively secure modular tibial tray-polyethylene insert interface of this device compared to other prostheses used at the time. Additionally, 14 the extremely low prevalence of patellar problems of the press-fit condylar knee when compared to the previously mentioned series may be related to the conforming patellofemoral groove and the all-polyethylene three-peg oval dome patellar component in this design19,25,26,28. Although, the authors later switched to the more-conforming, curved tibial insert and attempted to resect more bone, thus allowing thicker tibial inserts in the mid 1990’s when the concerns for flat articulating surfaces and thin polyethylene become recognized as a clinical problem, this series further suggests that with proper alignment of the knee, relatively flat articulating surfaces and modular tray inserts can produce durable results at nine to twelve years of follow-up. However, the ten percent prevalence of polyethylene thinning and the recently revised knee prompts concern that the second decade of use in these knees may be associated with an increasing failure rate. REFERENCES 1. Scott RD, Thornhill TS. Press-fit condylar total knee replacement. Techniques Orthop. 1986;1:41. 2. Scott RD, Thornhill TS. Press-fit condylar total knee replacement. Orthop Clin North Am. 1989;20:89-95. 3. Ayers DC, Dennis DA, Johanson NA, Pellegrini VD. Instructional Course Lecture, American Academy of Orthopaedic Surgeons. Common complications of total knee arthroplasty. J Bone Joint Surg Am. 1997;79:278-311. 4. Kim W, Rand JA, Chao EY. Biomechanics of the Knee. In: Rand, JA, ed. Total knee Arthroplasty. New York: Raven Press Ltd.; 1993:9-57. 5. Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop. 1989;248:13-4. 6. Merchant AC, Mercer RL, Jacobsen RH, and Cool CR. Roentgenographic analysis of patellofemoral congruence. J Bone Joint Surg Am. 1974;56:1391-6. 15 7. Ewald FC. The knee society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop. 1989;248:9-12. 8. Kaplan EL, Meier R. Nonparametric estimation from incomplete observation. J Am Statist Assn. 1958;53:457. 9. Wright TM, Bartel DL. The problem of surface damage in polyethylene total knee components. Clin Orthop. 1986;205:67-74. 10. Bartel DL, Bicknell VL, Wright TM. The effect of conformity, thickness, and material on stresses in ultra high molecular weight components for total joint replacement. J Bone Joint Surg Am. 1986;68:1041-51. 11. Engh GA, Dwyer KA, Hanes CK. Polyethylene wear of metal-backed tibial components in total and unicompartmental knee prosthesis. J Bone Joint Surg Br. 1992;74:9-17. 12. Kilgus DJ, Moreland JR, Finerman GA, Funahashi TT, Tipton JS. Catastrophic wear of tibial polyethylene inserts. Clin Orthop. 1991;273:223-31. 13. Landy MM, Walker PS. Wear of ultra-high-molecular-weight polyethylene components of 90 retrieved knee prostheses. J Arthroplasty. 1988;3:S75-85. 14. Wright TM, Rimnac CM, Stulberg SD, Mintz L, Tsao AK, Klein RW, McCrae C. Wear of polyethylene in total joint replacements. Clin Orthop. 1992;276:126-34. 15. Cameron HU. Tibial component wear in total knee replacement. Clin Orthop. 1994;309:29-32. 16. Chillag KJ, Barth E. An analysis of polyethylene thickness in modular total knee components. Clin Orthop. 1991;273:261-3. 16 17. Plante-Bordeneuve P, Freeman MA. Tibial high-density polyethylene wear in conforming tibiofemoral prosthesis. J Bone Joint Surg Br. 1993;75:630-6. 18. Wasielewski RC, Galante JO, Leighty RM, Natarajan RN, Rosenberg AG. Wear patterns on retrieved polyethylene tibial inserts and their relationship to technical considerations during total knee arthroplasty. Clin Orthop. 1994;299:31-43. 19. Schai PA, Thornhill TS, Scott RD. Total knee arthroplasty with the PFC system. J Bone Joint Surg Br. 1998;80:850-8. 20. Dennis DA, Clayton ML, O’Donnell S, Mack RP, Stringer EA. Posterior cruciate condylar total knee arthroplasty. Average 11-year follow-up evaluation. Clin Orthop. 1992;281:168-76. 21. Ritter MA, Herbst SA, Keating EM, Faris PM, Meding JB. Long-term survival analysis of a posterior cruciate retaining total condylar total knee arthroplasty. Clin Orthop. 1994;309:136-45. 22. Vince KG, Insall JN, Kelly MA. The total condylar prosthesis: 10- to 12-year results of a cemented knee replacement. J Bone Joint Surg Br. 1989;71:793-7. 23. Silverton C, Rosenberg AO, Barden RM, Sheinkop MB, Galante JO. The prosthesis-bone interface adjacent to tibial components inserted without cement. J Bone Joint Surg Am. 1996;78:340-7. 24. Buehler KO, Venn-Watson E, D’Lima DD, Colwell CW. The press-fit condylar total knee system. 8- to 10year results with a posterior cruciate-retaining design. J Arthroplasty. 2000;15:698-701. 25. Malkani AL, Rand JA, Bryan RS, Wallrichs SL. Total knee arthroplasty with the kinematic condylar prosthesis. J Bone Joint Surg Am. 1995;77:423-30. 17 26. Ewald FC, Wright RJ, Poss R, Thomas WH, Mason MD, Sledge CB. Kinematic total knee arthroplasty. A 10- to 14-year prospective follow-up review. J Arthroplasty. 1999;14:473-80. 27. Goldberg VM, Figgie MP, Figgie HE, Heiple KG, Sobel M. Use of a total condylar knee prosthesis for treatment of osteoarthritis and rheumatoid arthritis. J Bone Joint Surg Am. 1988;70:802-11. 28. Stern SH, Insall JN. Posterior stabilized prosthesis. Results after follow-up of nine to twelve years. J Bone Joint Surg Am. 1992;74:980-6. 18 Figure 1: The press-fit condylar total knee arthroplasty with the posterior-lipped polyethylene tibial insert. 19 Figure 2: Pictorial of the posterior-lipped polyethylene tibial insert utilized during these procedures. The curved, moreconforming, tibial insert is also shown for comparison. 20 Table 1: Comparison between the maximum pre-operative and post-operative flexion Pre-op Flexion (deg) No. of Knees (N) Post-op Flexion (deg) No. of knees (N) 90 2 90 90 - 110 110 0 2 0 90 - 110 37 90 90 - 110 110 1 19 17 110 24 90 90 - 110 110 1 11 12 21 Zones Femoral Component (lateral) 1 2 3 4 5 6 7 Tibial component (AP) 1 2 3 4 5 6 7 Tibial component (lateral) 1 2 3 Patellar component (Merchant) 1 2 3 4 5 No. of knees with Radiolucencies None < 1 mm 1 mm 43 58 62 46 63 63 63 18 3 1 16 - 2 2 1 - 38 58 63 59 63 63 63 20 3 4 - 5 2 - 42 59 63 20 3 - 1 1 - 62 62 61 62 62 1 1 2 1 1 - Figure 3: Summary of radiolucencies in sixty-three total knee arthroplasties and corresponding radiographic zones. Radiographic views include: lateral view of femoral component, anteroposterior and lateral views of the tibial component, and the patellar component. Adapted from Ewald et al., on behalf of the Knee Society7. 22 Figs 4-A through 4-H: Radiographs of bilateral knees of a female with severely symptomatic rheumatoid arthritis who was 59 years old at surgery. The clinical and functional Knee Society ratings were 45 and 70 points pre-operatively, and 93 and 90 points at final follow-up (11 years). Fig. 4-A: Pre-operative anteroposterior radiograph. Figs. 4-B, 4-C, 4-D: Anteroposterior and lateral view radiographs immediately post-operatively. Figs. 4-E, 4-F, 4-G, 4-H: Anteroposterior, lateral, and Merchant view radiographs at eleven years post-operatively. 23 Figs. 5-A through 5-H: Radiographs of bilateral knees of a male with severely symptomatic primary osteoarthritis who was 63 years old at surgery. The clinical and functional Knee Society ratings were 30 and 35 points pre-operatively, and 90 and 90 points at final follow-up (11 years). Fig. 5-A: Pre-operative anteroposterior radiograph. Figs. 5-B, 5-C, 5-D: Anteroposterior and lateral view radiographs immediately post-operatively. Figs. 5-E, 5-F, 5-G, 5-H: Anteroposterior, lateral, and Merchant view radiographs at eleven year post-operatively. 24 Figs. 6-A through 6-F: Radiographs of the left knee of a 74 year old male with symptomatic tibial and patellar polyethylene wear. The pre-revision clinical and functional Knee Society ratings were 95 and 75 points at 11.1 years of follow-up. An aseptically loose femoral component was identified in association with medial compartment tibial and patellar polyethylene wear at revision. Figs. 6-A, 6-B, 6-C: Anteroposterior, lateral, and Merchant view radiographs immediately post-operatively. Figs. 6-D, 6-E, 6-F: Anteroposterior, lateral, and Merchant view radiographs at eleven years post-operatively. 25 100% 90% 80% 70% 60% 50% 40% 30% 20% 10% 0% 0 2 4 6 8 10 12 Time(years) Figure 7: Kaplan-Meier survivorship curve results for the posterior cruciate-retaining press-fit condylar modular total knee prosthesis. Clinical endpoint was revision of any component for any reason. Shown above with 95% confidence intervals. 26