INFECTION CONTROL ROUNDS SURVEY – 2000-2001
advertisement

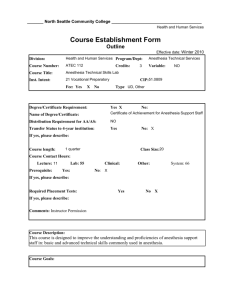
ANESTHESIA INFECTION PREVENTION ASSESSMENT TOOL Area Surveyed: Surveyed by: Date: Name ______________________________________________ Survey Items Policies and Procedures A policy/procedure (P&P) for Infection Prevention and Control (IPC) exists for anesthesia practices. Staff are trained upon hire/appointment and annually on IPC P&Ps. Anesthesia staff are able to articulate and practice per the anesthesia P&P, or hospital policies should a focused anesthesia one not exist. Hand Hygiene/Glove use Approved hand hygiene products are readily available and easy to access. Staff verbalizes understanding of when waterless products may not be used (e.g. visibly soiled hands). No jewelry on fingers, hands, wrists. Nails. Adherence to facility P&P. Hand Hygiene (HH) consistently used during movement from dirty to clean. Gloves in various sizes are available and easy to access. Clean gloves are worn for dirty procedures (intubation, suctioning) Gloves are then removed and HH performed prior to contact w/ clean environment (meds, keyboard). HH is performed before donning sterile gloves (e.g. central line placement). Personal Protective Equipment (PPE)/Attire Staff adhere to surgical attire P&P. Staff properly uses PPE for self protection (gown, mask covering nose and mouth, eye protection, gloves). In addition to Standard Precautions, staff adheres to requirements for isolation per P&P. Mechanism in place for anesthesia to know which patients are on precautions. Environment (clean vs. dirty) Clean and dirty spaces are clearly defined and treated as such. Staff responsible for room turnover are trained on steps involved in the process. What to discard and where, surface cleaning & disinfection. Method is in place that indicates that the room turnover is complete for the environment and medications and room is ready for the next patient. (A technician may be responsible for room turnover and the anesthesia staff for the medications). Sharps containers and trash bins are easy to access, not over filled and are located away from clean areas. Laryngoscope blades are bagged in storage until use. Workflow Efforts are made where feasible to limit staff turnover during the implant phase of a surgical procedure. Staff does not eat or drink in room. Clear separation of workflow between dirty and clean activities/spaces. No expired medications or supplies. Anesthesia workroom is clean and orderly and items are at least 6” off floor. Solid bottom shelves on any storage carts. Nonessential personal equipment is not brought into work area/room. (e.g. backpacks, computers). If visitors (e.g. parents) are allowed into Operating Room (OR), a consistent plan is in place for what they wear (scrubs or covering apparel) and when and where in the room they should and should not be. Frequently used supplies are easily accessible within the OR suite to ↓ traffic. Needed supplies are pulled prior to the case so as to limit need to go into the clean cart after case has started. If need to get more supplies from the cart, HH is to be performed prior to accessing the supplies. If products used to obscure inhalation mask odors are used (e.g. scented lip balm, scented extracts) a process is in place to keep product hygienic. Safe Injection Practices and Medications Single dose vials/syringes are used whenever possible. Sharps safety devices are in use and being used accordingly. Syringes are not used between patients (even if the needle has been changed). Changing the needle for such a purpose is unacceptable. Multi-dose vials are avoided when possible but when used between patients are not stored in the “immediate patient care” environment. After penetration of the rubber stopper, multi-dose vials require a beyond use date of 28 days unless the manufacturer’s expiration date will be reached before 28 days or 6-24-13 C = compliant NC = Not compliant N/A = not applicable C NC N/A Comments the product labeling (package insert) states otherwise. Yes Inspect vials and medication syringes for any signs of contamination or tampering. A new syringe and needle is used when accessing a vial. All medication and flush syringes are appropriately labeled. Medications are securely stored (locked) when not overseen by anesthesia staff. Medication storage and preparation area is maintained as a clean space. Used medications are not stored back on the clean preparation area. Vials/syringes are not stored or transported in clothing or pockets. Diaphragms of vials are cleansed using friction and sterile 70% isopropyl alcohol, ethyl alcohol, iodophor or other approved antiseptic swab and allowed to dry prior to accessing. Ampules are disinfected and allowed to dry prior to opening. Filter needles are used when accessing contents. Aseptic technique is used when handling and administering medications. Plans for consideration for drug shortages are in place. Process to prevent medication diversion in place. N/A Comments Intravenous (IV) supplies and Intravenous Therapy Infusion supplies such as needles, syringes, flush solutions, administration sets, or IV fluids are not used on or for more than one patient. Chevroning an IV site with tape prior to application of a dressing is not recommended. Utilize securement techniques after a sterile dressing is applied. Prime IV tubing w/in one hour of administration (United States Pharmacopeia USP<797>). Staff performing this task have been educated and periodically observed to assure proper aseptic technique. Performed in a clean work space. Tubing labeled with date/time/initials. If priming IV lines >1 hour before use, should incorporate a risk assessment and process/procedure/staff education to limit contamination during the process. Priming should be performed in a clean space and product in a secure location to avoid tampering. Tubing should be labeled with expiration date/time/initials per P&P. When patients are receiving a new central line during the case, new IV solution and tubing should be used for this line. No Streamline type of IV tubing and IV dressing with hospital P&P whenever possible. Stopcocks and manifold devices are handled using aseptic technique. IV caps/hubs are disinfected with sterile 70% isopropyl alcohol, ethyl/ethanol alcohol, iodophor or other approved antiseptic and allowed to dry before accessing. Stopcocks and manifold ports are covered with a sterile cap when not in use. A prompting system is in place for anticipated surgical prophylaxis redosing. Neuraxial Procedures (Epidural, spinal, or combined spinal-epidural administration of anesthetics, analgesics, or steroids; lumbar puncture (LP) or spinal tap; epidural blood patch; epidural lysis of adhesions; intrathecal chemotherapy; epidural or spinal injection of contrast agents for imaging; lumbar or spinal drainage catheters; or spinal cord stimulation trials). Cap, mask, sterile gloves and eye protection are worn during these procedures noted above. (Glasses for vision do not constitute full eye-protection) Note: an LP in anesthesia is usually used to instill medication hence included in this PPE use. Sterile drape, skin prep w/ dry time, sterile occlusive dressings are used. Respiratory care procedures/equipment Breathing circuit – use filter with efficiency rating of 95% for particle micron sizes of 0.3micron. IV bags or bottles are not to be used as a common source (e.g. saline flushes) for multiple patients. Disinfection Proper disinfection with hospital-approved product at end of case includes but is not limited to: anesthesia med/supply cart, anesthesia machine (knobs, surfaces, cords, keyboard, monitor, Adjustable Pressure Limiting (APL) valve), IV pole, laryngoscope handle) Single patient use items are discarded at the end of each case (e.g. circuits, airway bags, suction tubing). Stethoscopes disinfected per hospital P&P.. Are anesthesia staff responsible for cleaning and high-level disinfection and/or sterilization of any reusable equipment? If yes, competencies in place and all quality control measures performed and documented? Exposure Management Staff can articulate when and how to handle and report exposures to blood/body fluids (Human Immunodeficiency Virus (HIV), Hepatitis B, Hepatitis C) or other contagious diseases (e.g. Tuberculosis, Pertussis). Do you have any questions or concerns today about …? Miscellaneous Comments/ Observations: 6-24-13 REFERENCES Anesthesiology and Infection Control 1. Stackhouse RA, Beers R, Brown D, Brown M, Greene E., McCann ME, et al. and the ASA Committee on Occupational Health. Task Force on Infection Control. Recommendations for infection control for the practice of anesthesiology (Third Edition). Available from: http://www.asahq.org/For-Members/Standards-Guidelines-and-Statements.aspx#rec (refer to infection control section). Accessed December 7, 2011. 2. American Society of Anesthesiologists. Infection control for anesthesia professionals course. Available from: http://education.asahq.org/course/infection_control_2011. Accessed June 7, 2012. P&P 1. The Joint Commission E-dition Infection Prevention and Control Chapter. Available from: http://edition.jcrinc.com/Chapters.aspx. Accessed June 24, 2013. Hand Hygiene 1. Centers for Disease Control and Prevention. Guideline for hand hygiene in health-care settings: Recommendations of the healthcare infection control practices advisory committee and the HICPAC/SHEA/APIC/IDSA Hand Hygiene Task Force. MMWR Morb Mortal Wkly Rep 2002;51(No. RR-16):1-44. Available from: http://www.cdc.gov/handhygiene/Guidelines.html Accessed June 7, 2012. 2. World Health Organization. WHO guidelines on hand hygiene in health care. 2009. Available from: http://www.who.int/gpsc/5may/tools/9789241597906/en/index.html Accessed March 15, 2013. 3. Loftus RW, Koff MD, Burchman CC, Schwartzman JD, Throum V, Read ME, et al. Transmission of pathogenic bacterial organisms in the anesthesia work area. Anesthesiology 2008;109:399-407. http://journals.lww.com/anesthesiology/Fulltext/2008/09000/Transmission_of_Pathogenic_Bacterial_Organisms_in.9.asp x 4. Loftus RW, Muffly MK, Brown JR, Beach ML, Koff MD, Corwin HL, et al. Hand contamination of anesthesia providers is an important risk factor for intraoperative bacterial transmission. Anesth Analg 2011;112:98-105. http://www.anesthesiaanalgesia.org/content/112/1/98.full 5. Koff MD, Loftus RW, Burchman CC,et. al. Reduction in intraoperative bacterial contamination of peripheral intravenous tubing through the use of a novel device. Anesthesiology 2009;110:978-85. http://journals.lww.com/anesthesiology/Fulltext/2009/05000/Reduction_in_Intraoperative_Bacterial.10.aspx 6. Hollmann MW, Roy RC. Antisepsis in the time of antibiotics: following in the footsteps of John Snow and Joseph Lister. Anesth Analg 2011:112:1-3. http://www.anesthesia-analgesia.org/content/112/1/1 7. Roy RC, Brull SJ, Eichhorn JH. Surgical site infections and the anesthesia professionals' microbiome: We've all been slimed! Now what are we going to do about it? Anesth Analg 2011;112:4-7. http://www.anesthesiaanalgesia.org/content/112/1/4 8. Pivalizza EG, Gumbert SD, Maposa D. Is hand contamination of anesthesiologists really an "important" risk factor for intraoperative bacterial transmission?. Anesth Analg 2011;113:202; author reply 202-3. http://www.anesthesiaanalgesia.org/content/113/1/202.1.full 9. Kispert DP, Huysman BC, Petal HM, Beach ML, Loftus, RW, Reddy S. Infrequent handwashing by anesthesia providers is associated with intraoperative stopcock contamination. American Society of Anesthesiology Annual Meeting 2011. Abstract presentation. Session A118, October 17, 2011, Hall B2, 12:00-15:00. Available from: http://www.asaabstracts.com/strands/asaabstracts/abstract.htm;jsessionid=F93886FCBA76482D66C928176D6DE8D0? year=2011&index=15&absnum=6019. Accessed March 21, 2012. 10. Hopf HW, Rollings MD. Reducing perioperative infection is as simple as washing your hands. Anesthesiology 2009;110:959-60. http://journals.lww.com/anesthesiology/Fulltext/2009/05000/Reducing_Perioperative_Infection_Is_as_Simple_as.4.aspx 11. Biddle C, Shah J. Quantification of anesthesia providers’ hand hygiene in a busy metropolitan operating room: What would Semmelweis think? Am J Infect Control 2012;40:756-9. 12. National Fire Protection Association (NFPA) 101 Life Safety Code, 2009 edition – Note: defines volume limits for alcohol-based hand rubs in-use and in storage within smoke compartments in healthcare facilities. 13. American Society for Healthcare Engineering (ASHE). CMS and The Joint Commission define installation criteria of alcohol-based hand rub dispensers. Available from: http://www.jointcommission.org/assets/1/18/Acceptable%20Practices%20of%20Using%20Alcohol2.PDF PPE/Attire 1. Association of periOperative Registered Nurses (AORN). Recommended practices for surgical attire. AORN Perioperative Standards and Recommended Practices, 2010 Ed. pp.67-74. Available from: http://www.workingtowardzero.com/uploads/4/6/4/2/4642325/aorn_surgical_attire.pdf. Accessed May 15, 2012. 2. Braswell ML, Spruce L. AORN Recommended Practices: Implementing AORN recommended practices for surgical attire. AORN Journal, 2012;95:122-137. http://download.journals.elsevierhealth.com/pdfs/journals/00012092/PIIS0001209211011124.pdf 3. Siegel JD, Rhinehart E, Jackson M, Chiarello L, and the Healthcare Infection Control Practices Advisory Committee (HICPAC). Guideline for isolation precautions: Preventing transmission of infectious agents in healthcare settings. Am J Infect Control 2007;35:S65-164. http://www.cdc.gov/ncidod/dhqp/pdf/isolation2007.pdf 4. Occupational Safety and Health Standards, General Requirements, Personal Protective Equipment, 1910.132(a). Available from: http://www.osha.gov/pls/oshaweb/owadisp.show_document?p_table=STANDARDS&p_id=9777 . Accessed November 26, 2012. Safe Injection Practices 1. CDC Recommended Injection Practices for Patient Safety. Available from: https://www.premierinc.com/safety/topics/safe_injection_practices/Downloads/CDC-Recommended-Injection-PracticesPatient-SafetyV2.pdf. Accessed July 5, 2012 2. Dolan SA, Felizardo G, Barnes S, Cox TR, Patrick M, Ward KS, et al. APIC position paper: Safe injection, infusion, and medication vial practices in health care. Am J Infect Control 2010;38:167-172. http://www.ajicjournal.org/article/S01966553(10)00061-1/pdf 3. Steinmann E, Ciesek S, Friesland M, Erichsen TJ Pietschmann T. Correspondence: Prolonged survival of hepatitis C virus in the anesthetic propofol. Clin Infect Dis 2011;53:963-96. http://cid.oxfordjournals.org/content/53/9/963.full 6-24-13 4. Hellinger WC, Bacalis, LP, Kay RS, Thompson ND, Xia GL, Lin Y, et al. Health care-associated hepatitis C virus infections attributed to narcotic diversion. Ann Intern Med 2012;156:477-82. http://annals.org/article.aspx?articleid=1103743 5. Department of Health and Human Services. Office of Clinical Standards and Quality/Survey & Certification Group. Safe use of single dose/single use medications to prevent healthcare-associated infections. June 15, 2012. Available from: http://www.cms.gov/Medicare/Provider-Enrollment-andCertification/SurveyCertificationGenInfo/Downloads/Survey-and-Cert-Letter-12-35.pdf. Accessed June 30, 2012. 6. Greene ES, Beers RA, Stackhouse RA. Preventing healthcare-associated transmission of bloodborne pathogens secondary to unsafe injection practices. ASA Newsl 2009;73:28-31. IV’s and IV Therapy 1. O’Grady NP, Alexander M, Burns LA, Dellinger P, Garland J, Heard SO et al. and the Healthcare Infection Control Practices Advisory Committee (CDC). Guidelines for the prevention of intravascular catheter-related infections, 2011. Available from: http://www.cdc.gov/hicpac/pdf/guidelines/bsi-guidelines-2011.pdf. Accessed November 26, 2012. 2. Kaler W, Chinn R. Successful disinfection of needleless access ports: A matter of time and friction. JAVA 2007;12:140142. 3. Doit C, Loukil A, Simon M, Ferroni A, Fontan J-E, Bonacorsi S, et al. Outbreak of Burkholderia cepacia bacteremia in a pediatric hospital due to contamination of lipid emulsion stoppers. J Clin Microbiol 2004; 42: 2227–2230. 4. Dolan SA, Felizardo G, Barnes S, Cox TR, Patrick M, Ward KS, et al. APIC position paper: Safe injection, infusion, and medication vial practices in health care. Am J Infect Control 2010;38:167-172. http://www.ajicjournal.org/article/S01966553(10)00061-1/pdf 5. Cady M, Gross L, Lee N. Letter to the Editor - IV tape: A potential vector for infection. APSF Newsletter. Winter 2011.61-62. http://www.apsf.org/newsletters/pdf/winter_2011.pdf 6. US Pharmacopeial Convention, Inc. General Chapter <797> Pharmaceutical Compounding-Sterile Preparations. The United States Pharmacopeia, 32nd Edition and The National Formulary. 27th Edition Rockville, MD: United States Pharmacopeial convention; 2009. P.318-54. http://www.usp.org/ (Note: check with your pharmacy department to see if they have this document) Neuraxial Procedures 1. Practice Advisory for the Prevention, Diagnosis, and Management of Infectious Complications Associated with Neuraxial Techniques: A report by the American Society of Anesthesiologists task force on infectious complications associated with neuraxial techniques. Anesthesiology 2010;112:530-545. http://journals.lww.com/anesthesiology/Fulltext/2010/03000/Practice_Advisory_for_the_Prevention,_Diagnosis,.12.aspx 2. Hebl JR. The importance and implications of aseptic techniques during regional anesthesia. Region Anesth Pain M 2006;31:311-323. 3. de Fijter S, DiOrio M, Carmean J, Schaffzin J, Quinn M, Musser K, et. al. Bacterial meningitis after intrapartum spinal anesthesia --- New York and Ohio, 2008—2009.MMW R 2010;59:65-69. http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5903a1.htm 4. Kainer M, Wiese AD, Benedict K, Braden C, Brandt K, Harris J, et al. Multistate outbreak of fungal infection associated with injection of methylprednisolone acetate solution from a single compounding pharmacy – United States 2012. MMWR 2012;61(41):839-842. Respiratory Care Procedures/Equipment 1. Tablan OC, Anderson LJ, Besser R, Bridges C, Hajjeh R. CDC Healthcare Infection Control Practices Advisory Committee. Guidelines for preventing healthcare-associated pneumonia. 2003:1-179. http://www.cdc.gov/hicpac/pdf/guidelines/HApneu2003guidelines.pdf 2. Langevin PB, Rand KH, Layon J. The potential for dissemination of mycobacterium tuberculosis through the anesthesia breathing circuit. Chest 1999;115:1107-1114. http://chestjournal.chestpubs.org/content/115/4/1107.full.pdf+html 3. ASA Committee on Quality Management and Departmental Administration. Statement on standard practice for infection prevention and control instruments for tracheal intubation. Approved by ASA House of Delegates, October 20, 2010. Available from: www.asahq.org/.../Standards%20Guidelines%20Stmts/Infection%20Prevention%20Tracheal%20Intubation.ashx. Accessed March 28, 2012. 4. The Joint Commission. Standards FAQ Details: Laryngoscope blades. October 24, 2011. Avaiable from: http://www.jointcommission.org/mobile/standards_information/jcfaqdetails.aspx?StandardsFAQId=386&StandardsFAQC hapterId=69. Accessed June 24, 2013. Environment/Disinfection 1. Rutala WA, Weber DJ and the Healthcare Infection Control Practices Advisory Committee (HICPAC). Guideline for disinfection and sterilization in healthcare facilities, 2008. Available from: http://www.cdc.gov/hicpac/Disinfection_Sterilization/acknowledg.html. Accessed April 12, 2012. 2. Rutala WA, White MS, Gergen MF, Weber DJ. Bacterial contamination of keyboards: Efficacy and functional impact of disinfectants. Infect Control Hosp Epidemiol 2006;27:372. 3. Loftus RW, Koff MD, Burchman CC, Schwartzman JD, Thorum V, Read M, et. al. Transmission of Pathogenic Bacterial Organisms in the Anesthesia Work Area. Anesthesiology 2008;109:399-407. http://journals.lww.com/anesthesiology/Fulltext/2008/09000/Transmission_of_Pathogenic_Bacterial_Organisms_in.9.asp x 4. Huang S, Datta R, Platt R. Risk of acquiring antibiotic-resistant bacteria from prior room occupants. Ach Intern Med. 2006;166:1945-51. 5. Drees M, Snydman D, Schmid CH, Barefoot L, Hansjosten K, Vue PM, et al. Prior environmental contamination increases the risk of acquisition of vancomycin-resistant enterocci. Clin Infect Dis 2008;46:678-685. 6. Otter JA, Yezli S, French GL. The role played by contaminated surfaces in the transmission of nosocomial pathogens. Infect Control Hosp Epidemiol 2011;32:687-699. Bloodborne Pathogen Exposure Management 1. Updated U.S. Public Health Service Guidelines for the management of occupational exposures to HBV, HCV, and HIV and recommendations for postexposure prophylaxis. MMWR Morb Mortal Wkly Rep 2001;54 (RR-11):1-43. Available from: http://www.cdc.gov/mmwr/PDF/rr/rr5011.pdf. Accessed May 15, 2012. 6-24-13 2. Centers for Disease Control (CDC). Updated U.S. Public Health Service Guidelines for the management of occupational exposures to HIV and recommendations for postexposure prophylaxis. MMWR 2005;54 (RR-9):1-24. http://www.cdc.gov/mmwr/PDF/rr/rr5409.pdf 3. Mountain Plains AID Education and Training Center (in consultation with National Clinicians’ Postexposure Prophylaxis (PEP) Hotline. PEP Steps, A Quick Guide to Postexposure Prophylaxis in the Health Care Setting (April 2006) http://www.mpaetc.org/downloads/PEP%20final%20(2006).pdf Infection Prevention in Anesthesia Practice: A Tool to Assess Risk and Compliance Abstract Transmission of bacterial and viral infections to patients from improper anesthesia infection prevention and control practices continues to be reported. Recommendations for Infection Control for the Practice of Anesthesiology were recently revised. The process used to develop an anesthesia infection prevention assessment tool is described. The tool is intended to encourage collaboration between infection preventionists and anesthesia providers in an effort to assess infection prevention and control practices in various healthcare settings. Transmission of bacterial and viral infections to patients from improper anesthesia infection prevention and control practices continues to be reported1. Historically, reports of Propofol bacterial contamination causing patient infections2-4 resulted in increased awareness and changes in handling practices but issues still remain, especially related to viral bloodborne infections. 5 Publications highlighting infection prevention concerns have addressed several processes utilized in the practice of administering anesthesia including safe injection practices6, hand hygiene7-10, narcotic diversion11, environmental contamination12 and equipment use/reprocessing.12 In 2011, the American Society of Anesthesiologist (ASA) revised its “Recommendations for Infection Control for the Practice of Anesthesiology”.13 With the publication of these recommendations, infection preventionists (IPs) have a prime opportunity to initiate an infection prevention risk and needs assessment of anesthesia practices within their organizations. It is essential that IPs partner with anesthesia colleagues to improve their understanding of anesthesia practices and to determine how to best implement safe practices to prevent infections in patients utilizing anesthesia services. The development of an evidence-based tool that could be utilized as both an educational component as well as a vehicle to assess risk and monitor compliance in any type of anesthesia setting was the impetus for a group of pediatric IPs to develop an anesthesia infection prevention assessment tool. The pediatric IPs are members of the Infection Prevention Directors (IPD) Forum at Children’s Hospital Association (CHA), a group of hospital epidemiologists and IPs from children’s hospitals across the United States. The group’s primary mission is to provide national leadership and content expertise in pediatric infection prevention and control and to identify priorities for infection prevention issues that impact children and the healthcare facilities that serve them. In 2012, an opportunity to foster and improve partnerships between IPs and their anesthesia teams was introduced and subsequently endorsed as a project by the group. The goal was to develop an anesthesia infection prevention assessment tool and an accompanying evidence-based reference list (Figure 1) that could be used in conjunction with current ASA recommendations to begin or expand conversations with anesthesia teams on key infection prevention measures to improve patient safety. An initial brainstorming session to draft content was held among IPD Forum members present at a spring 2012 meeting of the group. A smaller working group continued to meet to refine the content and collect supporting references to provide added strength to the document for discussions with anesthesia teams. In addition, a few members circulated the document among anesthesia contacts at their respective hospitals for input. A final version was reviewed by the IPD Forum at its fall 2012 meeting. The initial focus of this assessment tool was anesthesia infection prevention practices in surgical and procedure suites, but many of these assessment items are relevant in other settings where anesthesia services are provided. Now that the assessment tool and references have been finalized, efforts are necessary to assure that infection prevention practices in anesthesia care are optimal. The best ideas for innovation come from clinicians who work directly with the process being addressed, but successfully implementing and sustaining improvement in anesthesia practice requires more than a new idea or tool. The support of senior leadership within an organization is critical in that it maintains a high level of transparency of results and accountability for goals14 In addition, projects that include a component of behavior change generally require intrinsically motivated and enthusiastic champions working across professions, i.e. coalitions of managers and frontline staff working together rather than a single leader.15,16 And because the organizational culture of healthcare settings is typically 6-24-13 hierarchical, leadership inclusiveness that encourages collaboration instead of a more authoritative style is essential to the function of an effective team. Such leadership behaviors include “explicitly soliciting team input, engaging in participatory decision making, and facilitating the inclusion of non-team members”.17 For example, Seattle Children’s Hospital embarked upon a quality improvement project around anesthesia infection prevention practices in 2009. The Director of Anesthesia assembled and led a team of volunteers (champions) from across disciplines in the procedural areas, including anesthesiologists and anesthetists, surgeons, nurses, anesthesia technicians, central services staff, quality improvement specialists, environmental services staff, and IPs. A rapid-cycle process improvement strategy facilitated open communication and shared decision making and a tool was used to assess practice throughout the project. Upon completion of the project, the team was able to demonstrate decreased central line-associated bloodstream infections (CLA-BSI) rates for patients traveling off an intensive care unit with anesthesia providers. 18 Each institution can initially individualize their strategy for implementation of the tool by gathering the key players, reviewing the assessment tool, setting up process observations, mimicking simulation steps, and then systematically focusing on areas in need of improvement. Furthermore, using a document such as the anesthesia assessment tool allows an organization to measure performance to a standard and provide feedback to clinicians. Measurement and feedback, in turn, are used to identify current state (baseline performance), identify problems, and develop and test strategies for improvement. Using simple, quick data collection tools such as check sheets and checklists minimizes the burden of the measurement and contributes to the sustainability of performance improvement projects.15 In summary, the anesthesia infection prevention assessment tool provides a framework to assess infection prevention practices in anesthesia care and to focus efforts to prevent harm and improve patient safety. As the tool encompasses infection prevention and control recommendations of the American Society of Anesthesiologists as well as those of other professional, regulatory and accrediting organizations, it can be used to partner with anesthesia staff to develop infection prevention policies for anesthesia care and to define safe practices. The tool can also be used for the ongoing assessment of infection prevention practices by anesthesia teams, infection preventionists and surveyors, and to measure the impact of specific quality improvement efforts or interventions on practice. Acknowledgements: Children's Hospital Association Infection Prevention Directors Forum REFERENCES 1. Centers for Disease Control and Prevention. Outbreaks and Patient Notifications in Outpatient Settings. Available from: http://www.cdc.gov/HAI/settings/outpatient/outbreaks-patient-notifications.html. Accessed December 2, 2012. 2. Centers for Disease Control and Prevention. Postsurgical infections associated with an extrinsically contaminated intravenous anesthetic agent: California, Illinois, Maine, and Michigan, 1990. MMWR Morb Mortal Wkly Rep 1990;39:426-33. 3. Bennett SN, McNeil MM, Bland LA, Arduino MJ, Villarino ME, Perotta DM, et al. Postoperative infections traced to contamination of an intravenous anesthetic, propofol. N Engl J Med 1995;333:147-54. 4. Henry B, Plante-Jenkiins C, Ostrowska K. An outbreak of Serratia marcescens associated with the anesthetic agent Propofol. Am J Infect Control 2001;29:312-15. 5. Centers for Disease Control and Prevention. Acute hepatitis C virus infections attributed to unsafe injection practices at an endoscopy clinic: Nevada, 2007. MMWR Morb Mortal Wkly Rep 2008;57:513-17. 6. Greene ES, Beers RA, Stackhouse RA. Preventing healthcare-associated transmission of bloodborne pathogens secondary to unsafe injection practices. ASA Newsl 2009;73:28-31. 7. Loftus RW, Muffly MK, Brown JR, et. al. Hand contamination of anesthesia providers is an important risk factor for intraoperative bacterial transmission. Anesth Analg 2011;112:98-105. 6-24-13 8. Roy RC, Brull SJ, Eichhorn JH. Surgical aite infections and the anesthesia professionals' microbiome: We've all been slimed! Now what are we going to do about it? Anesth Analg 2011;112:4-7. 9. Biddle C, Shah J. Quantification of anesthesia providers’ hand hygine in a busy metropolitan operating room: What would Semmelweis think? Am J infect Control 2012;40:756-9. 10. Hopf HW, Rollings MD. Reducing perioperative infection is as simple as washing your hands. Anesthesiology 2009;110:959-60. 11. Hellinger WC, Bacalis, LP, Kay RS, Thompson ND, Xia GL, Lin Y, Khudyakov YE, et al. Health care-associated hepatitis C virus infections attributed to narcotic diversion. Ann Intern Med 2012;156:477-82. 12. Loftus RW, Koff MD, Burchman CC, et. al. Transmission of pathogenic bacterial organisms in the anesthesia work area. Anesthesiology 2008;109:399-407. 13. Stackhouse RA, Beers R, Brown D, Brown M, Greene E., McCann ME, et al. and the ASA Committee on Occupational Health. Task Force on Infection Control. Recommendations for Infection Control for the Practice of Anesthesiology (Third Edition). Available from: http://www.asahq.org/For-Members/Standards-Guidelines-and-Statements.aspx#rec (refer to infection control section). Accessed December 7, 2011 14. Mandel KE, Muething SE, Schoettker PJ, Kotagal UR. Transforming safety and effectiveness in pediatric hospital care locally and nationally. Pediatr Clin North Am 2009;56:905-18. 15. Randolph G, Esporas M, Provost L, Massie S, Bundy DG. Model for improvement – Part two: Measurement and feedback for quality improvement efforts. Pediatr Clin North Am 2009;56:779-98. 16. Damschroder L, Banaszak-Holl J, Kowalski C, Forman J, Saint S, Krein SL. The role of the “champion” in infection prevention: Results from a multisite qualitative study. Qual Safe Healthcare 2009;18:434-60. 17. Howard J, Shaw E, Felsen C, Crabtree B. Physicians as inclusive leaders: insights from a participatory quality improvement intervention. Qual Manag Health Care 2012;21:135-45. 18. Martin LD, Rampersad SE, Geiduschek JM, Zerr DM, Weiss GK. Modification of anesthesia practice reduces catheterassociated bloodstream infections: a quality improvement initiative. Paediatr Anaesth 2013:10.111/pan.12165. (Epub ahead of print). 6-24-13