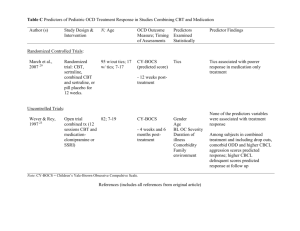
Table 1 Predictors of Pediatric OCD Treatment Response in CBT
advertisement

Table A Predictors of Pediatric OCD Treatment Response in CBT Only Studies Author (s) Study Design & Intervention N; Age OCD Outcome Measure; Timing of Assessments Predictors Examined Statistically Predictor Findings ADIS-P CY-BOCS NIMH GOCS Child Age Age was not related to treatment response Randomized Controlled Trials: Barrett et al., 2004 12 Randomized trial: 77; 7-17 individual cognitivebehavioral family therapy (CBFT), group CBFT or waitlist control. 14 weekly sessions and 2 booster sessions - Post-treatment, 3 and 6 month followup Uncontrolled Trials: Bolton et al., 1995 13 Long term follow up study of adolescents treated 9 – 14 years prior (see Bolton et al., 1983) *5 patients were treated with clomipramine in addition to behavior therapy Benazon et al., 2002 26 Open trial: E/RP, 12 weekly sessions 14; 23-31 Medical records PSE Youth PHS were 1218 at - 9 to 14 years posttime of treatment treatment Duration of illness Severity Parental psychopathology No variable (duration of illness, severity, or parental psychopathology) was associated with treatment response 16; 8-17 Gender Comorbid anxiety disorder Neither gender nor comorbid anxiety disorder were associated with treatment response CY-BOCS NIMH GOCS CGI-I - Post-treatment Table A Continued Author (s) Study Design & Intervention N; Age OCD Outcome Measure; Timing of Assessments Predictors Examined Statistically Predictor Findings Piacentini et al., 2002 Open trial: E/RP, weekly sessions, mean of 12.5 sessions attended 42; 5-17 CY-BOCS NIMH GOCS CGI-I Child age Gender Duration of OCD BL OCD severity Comorbidity Age, gender, duration of OCD, and comorbid tics were not associated with treatment response Tic disorder Comorbid tic disorder was not associated with treatment response BL OCD severity Comorbid depression, anxiety Family functioning More severe obsessions/compulsions, and higher level of family dysfunction at pretreatment predicted poorer outcome at 18 month follow-up 16 - Post-treatment Himle et al., 2003 28 Open trial: group E/RP, 7 weekly sessions 19; 1217 CY-BOCS BL CY-BOCS Obsessions score, greater OCDrelated academic impairment, higher level of anxiety symptoms were associated with poorer outcome - Post-treatment Barrett et al., 2005 17 Long-term follow-up study using subsample from Barrett et al. (2004) study 48; 8-19 ADIS-P CY-BOCS NIMH GOCS - 12 and 18 month follow-up Comorbid depression and anxiety were not associated with treatment response Note: LOI-CV = ADIS-P = Anxiety Disorders Interview Schedule – Parent Version, CY-BOCS = Children’s Yale-Brown Obsessive Compulsive Scale, NIMH GOCS = NIMH Global Scale for OCD, PSE = Present State Examination, PHS = Past History Schedule, CGI-I = Clinical Global Impression of Improvement. References (includes all references from original article) 1. Heyman I, Fombonne E, Simmons H, Ford T, Meltzer H, Goodman R. Prevalence of obsessive-compulsive disorder in the British nationwide survey of child mental health. Br J Psychiatry. 2001; 179:324-329. 2. Zohar AH. The epidemiology of obsessive-compulsive disorder in children and adolescents. Child Adolesc Psychiatr Clin N Am. 1999; 8:445-460. 3. POTS. Cognitive-behavior therapy, sertraline, and their combination for children and adolescents with obsessive-compulsive disorder: the Pediatric OCD Treatment Study (POTS) randomized controlled trial. JAMA. 2004; 292:1969-1976 4. Kraemer HC, Stice E, Kazdin A, Offord D, Kupfer D. How do risk factors work together? Mediators, moderators, and independent, overlapping, and proxy risk factors. Am J Psychiatry. 2001; 158:848-856. 5. O'Kearney RT, Anstey KJ, von Sanden C. Behavioural and cognitive behavioural therapy for obsessive compulsive disorder in children and adolescents. Cochrane Database Syst Rev. 2006; CD004856. 6. Abramowitz JS. Effectiveness of psychological and pharmacological treatments for obsessive-compulsive disorder: a quantitative review. J Consult Clin Psychol. 1997; 65:44-52. 7. Freeman JB, Choate-Summers ML, Moore PS, et al. Cognitive behavioral treatment for young children with obsessivecompulsive disorder. Biol Psychiatry. 2007; 61:337-343. 8. Geller DA, Biederman J, Stewart SE, et al. Impact of comorbidity on treatment response to paroxetine in pediatric obsessivecompulsive disorder: is the use of exclusion criteria empirically supported in randomized clinical trials? J Child Adolesc Psychopharmacol. 2003; 13 Suppl 1:S19-S29. 9. March JS, Franklin M, Nelson A, Foa E. Cognitive-behavioral psychotherapy for pediatric obsessive-compulsive disorder. J Clin Child Psychol. 2001; 30:8-18. 10. Thomsen PH. Obsessive-complusive disorder: pharmacological treatment. Eur Child Adolesc Psychiatry. 2000; 9 Suppl 1:I76I84. 11. Turner CM. Cognitive-behavioural theory and therapy for obsessive-compulsive disorder in children and adolescents: current status and future directions. Clin Psychol Rev. 2006; 26:912-938. 12. Barrett P, Healy-Farrell L, March JS. Cognitive-behavioral family treatment of childhood obsessive-compulsive disorder: a controlled trial. J Am Acad Child Adolesc Psychiatry. 2004; 43:46-62. 13. Bolton D, Luckie M, Steinberg D. Long-term course of obsessive-compulsive disorder treated in adolescence. J Am Acad Child Adolesc Psychiatry. 1995; 34:1441-1450. 14. Flament MF, Rapoport JL, Berg CJ, et al. Clomipramine treatment of childhood obsessive-compulsive disorder. A double-blind controlled study. Arch Gen Psychiatry. 1985; 42:977-983. 15. Riddle MA, Reeve EA, Yaryura-Tobias JA, et al. Fluvoxamine for children and adolescents with obsessive-compulsive disorder: a randomized, controlled, multicenter trial. J Am Acad Child Adolesc Psychiatry. 2001; 40:222-229. 16. Piacentini J, Bergman RL, Jacobs C, McCracken JT, Kretchman J. Open trial of cognitive behavior therapy for childhood obsessive-compulsive disorder. J Anxiety Disord. 2002; 16:207-219. 17. Barrett P, Farrell L, Dadds M, Boulter N. Cognitive-behavioral family treatment of childhood obsessive-compulsive disorder: long-term follow-up and predictors of outcome. J Am Acad Child Adolesc Psychiatry. 2005; 44:1005-1014. 18. Leonard HL, Swedo SE, Rapoport JL, et al. Treatment of obsessive-compulsive disorder with clomipramine and desipramine in children and adolescents. A double-blind crossover comparison. Arch Gen Psychiatry. 1989; 46:1088-1092. 19. March JS, Biederman J, Wolkow R, et al. Sertraline in children and adolescents with obsessive-compulsive disorder: a multicenter randomized controlled trial. JAMA. 1998; 280:1752-1756. 20. Thomsen PH, Ebbesen C, Persson C. Long-term experience with citalopram in the treatment of adolescent OCD. J Am Acad Child Adolesc Psychiatry. 2001; 40:895-902. 21. Geller DA, Wagner KD, Emslie G, et al. Paroxetine treatment in children and adolescents with obsessive-compulsive disorder: a randomized, multicenter, double-blind, placebo-controlled trial. J Am Acad Child Adolesc Psychiatry. 2004; 43:1387-1396. 22. Leonard HL, Swedo SE, Lenane MC, et al. A 2- to 7-year follow-up study of 54 obsessive-compulsive children and adolescents. Arch Gen Psychiatry. 1993; 50:429-439. 23. Wever C, Rey JM. Juvenile obsessive-compulsive disorder. Aust N Z J Psychiatry. 1997; 31:105-113. 24. Wagner KD, Cook EH, Chung H, Messig M. Remission status after long-term sertraline treatment of pediatric obsessivecompulsive disorder. J Child Adolesc Psychopharmacol. 2003; 13 Suppl 1:S53-S60. 25. Masi G, Millepiedi S, Mucci M, Bertini N, Milantoni L, Arcangeli F. A naturalistic study of referred children and adolescents with obsessive-compulsive disorder. J Am Acad Child Adolesc Psychiatry. 2005; 44:673-681. 26. Benazon NR, Ager J, Rosenberg DR. Cognitive behavior therapy in treatment-naive children and adolescents with obsessivecompulsive disorder: an open trial. Behav Res Ther. 2002; 40:529-539. 27. Rosenberg DR, Stewart CM, Fitzgerald KD, Tawile V, Carroll E. Paroxetine open-label treatment of pediatric outpatients with obsessive-compulsive disorder. J Am Acad Child Adolesc Psychiatry. 1999; 38:1180-1185. 28. Himle JA, Fischer DJ, Van Etten ML, Janeck AS, Hanna GL. Group behavioral therapy for adolescents with tic-related and nontic-related obsessive-compulsive disorder. Depress Anxiety. 2003; 17:73-77. 29. March JS, Franklin ME, Leonard H, et al. Tics moderate treatment outcome with sertraline but not cognitive-behavior therapy in pediatric obsessive-compulsive disorder. Biol Psychiatry. 2007; 61:344-347. 30. Graeff FG, Parente A, Del Ben CM, Guimaraes FS. Pharmacology of human experimental anxiety. Braz J Med Biol Res. 2003; 36:421-432. 31. Andres S, Boget T, Lazaro L, et al. Neuropsychological performance in children and adolescents with obsessive-compulsive disorder and influence of clinical variables. Biol Psychiatry. 2007; 61:946-951. 32. Greisberg S, McKay D. Neuropsychology of obsessive-compulsive disorder: a review and treatment implications. Clin Psychol Rev. 2003; 23:95-117. 33. Schultz RT, Evans DW, Wolff M. Neuropsychological models of childhood obsessive-compulsive disorder. Child Adolesc Psychiatr Clin N Am. 1999; 8:513-31. 34. Andres S, Lazaro L, Salamero M, Boget T, Penades R, Castro-Fornieles J. Changes in cognitive dysfunction in children and adolescents with obsessive-compulsive disorder after treatment. J Psychiatr Res. 2008; 42:507-514. 35. Barrett PM, Dadds MR, Rapee RM. Family treatment of childhood anxiety: a controlled trial. J Consult Clin Psychol. 1996; 64:333-342. 36. Yaryura-Tobias JA, Grunes MS, Walz J, Neziroglu F. Parental obsessive-compulsive disorder as a prognostic factor in a year long fluvoxamine treatment in childhood and adolescent obsessive-compulsive disorder. Int Clin Psychopharmacol. 2000; 15:163168. 37. Silverman WK, Kurtines WM, Ginsburg GS, Weems CF, Rabian B, Serafini LT. Contingency management, self-control, and education support in the treatment of childhood phobic disorders: a randomized clinical trial. J Consult Clin Psychol. 1999; 67:675-687. 38. Treadwell KR, Flannery EC, Kendall PC. Ethnicity and gender in relation to adaptive functioning, diagnostic status, and treatment outcome in children from an anxiety clinic. J Anxiety Disord. 1995; 9:373-384. 39. Silverman WK, Kurtines WM, Ginsburg GS, Weems CF, Lumpkin PW, Carmichael DH. Treating anxiety disorders in children with group cognitive-behaviorial therapy: a randomized clinical trial. J Consult Clin Psychol. 1999; 67:995-1003. 40. Beidel DC, Turner SM, Morris TL. Behavioral treatment of childhood social phobia. J Consult Clin Psychol. 2000; 68:1072-1080. 41. Berman S, Weems CF, Silverman WK. Predictors of outcome in exposure-based cognitive and behavioral treatments for phobic and anxiety disorders in children. Behavior Therapy. 2000; 31:713-731. 42. Cobham VE, Dadds MR, Spence SH. The role of parental anxiety in the treatment of childhood anxiety. J Consult Clin Psychol. 1998; 66:893-905. 43. Mendlowitz SL, Manassis K, Bradley S, Scapillato D, Miezitis S, Shaw BF. Cognitive-behavioral group treatments in childhood anxiety disorders: the role of parental involvement. J Am Acad Child Adolesc Psychiatry. 1999; 38:1223-1229. 44. Walkup JT, Labellarte MJ, Riddle MA, et al. Searching for moderators and mediators of pharmacological treatment effects in children and adolescents with anxiety disorders. J Am Acad Child Adolesc Psychiatry. 2003; 42:13-21. 45. Geller DA, Hoog SL, Heiligenstein JH, et al. Fluoxetine treatment for obsessive-compulsive disorder in children and adolescents: a placebo-controlled clinical trial. J Am Acad Child Adolesc Psychiatry. 2001; 40:773-779. 46. Thomsen PH. Child and adolescent obsessive-compulsive disorder treated with citalopram: findings from an open trial of 23 cases. J Child Adolesc Psychopharmacol. 1997; 7:157-166.