Stages of viral infection
advertisement
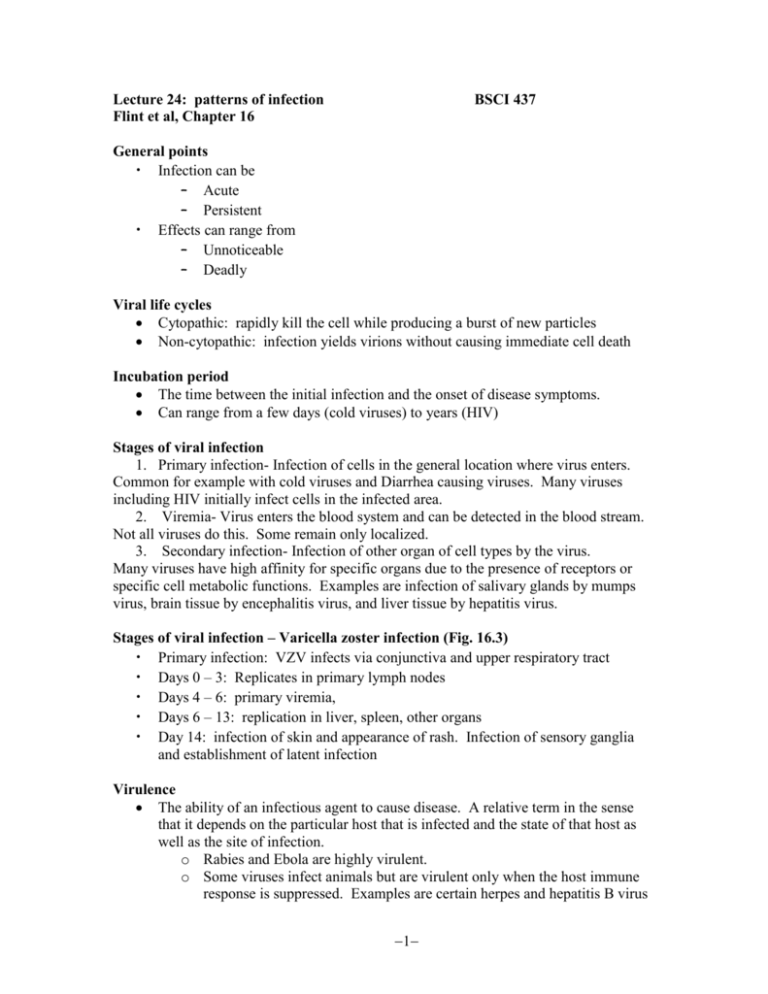
Lecture 24: patterns of infection Flint et al, Chapter 16 BSCI 437 General points • Infection can be – Acute – Persistent • Effects can range from – Unnoticeable – Deadly Viral life cycles Cytopathic: rapidly kill the cell while producing a burst of new particles Non-cytopathic: infection yields virions without causing immediate cell death Incubation period The time between the initial infection and the onset of disease symptoms. Can range from a few days (cold viruses) to years (HIV) Stages of viral infection 1. Primary infection- Infection of cells in the general location where virus enters. Common for example with cold viruses and Diarrhea causing viruses. Many viruses including HIV initially infect cells in the infected area. 2. Viremia- Virus enters the blood system and can be detected in the blood stream. Not all viruses do this. Some remain only localized. 3. Secondary infection- Infection of other organ of cell types by the virus. Many viruses have high affinity for specific organs due to the presence of receptors or specific cell metabolic functions. Examples are infection of salivary glands by mumps virus, brain tissue by encephalitis virus, and liver tissue by hepatitis virus. Stages of viral infection – Varicella zoster infection (Fig. 16.3) • Primary infection: VZV infects via conjunctiva and upper respiratory tract • Days 0 – 3: Replicates in primary lymph nodes • Days 4 – 6: primary viremia, • Days 6 – 13: replication in liver, spleen, other organs • Day 14: infection of skin and appearance of rash. Infection of sensory ganglia and establishment of latent infection Virulence The ability of an infectious agent to cause disease. A relative term in the sense that it depends on the particular host that is infected and the state of that host as well as the site of infection. o Rabies and Ebola are highly virulent. o Some viruses infect animals but are virulent only when the host immune response is suppressed. Examples are certain herpes and hepatitis B virus 1 that become virulent when human hosts are treated with immunosuppressant drugs after organ transplant. General patterns of infection (Fig. 16.1) Acute Persistent Latent, reactivating Slow Acute Infections • Acute infections only detected by clinical symptoms. • Can be acutely infected but assymptomatic…subclincal. • Viruses usually produce large amounts of progeny • Rapid onset of symptoms • Rapid resolution of infection either by – Immune clearance or – Death Defense against acute infections Most acute infections are rapidly resolved Limited by the intrinsic and innate immune responses Localization to the immediate site of infection, Clearance by macrophages, NK cells, polymorphonuclear cells, complement. Adaptive immune response provides memory against subsequent infection. Virus-specific humoral and cellular responses If not quickly limited, acute infections are resolved by host death e.g. many haemorragic viruses, severely immunocompromised patients Antigenic variation – the viral response • Survival of acute infection lifelong immunity to that specific virus • How is it that we get sick from other acute viruses over and over? o e.g. common cold, influenza • Answer: viruses capitalize on high rates of mutation to evolve around immune response • Structural plasticity: virions that can tolerate many amino acid substitutions yet remain infections. o Rhinoviruses and Influenzaviruses are incredibly structurally plastic. o Limits ability to make effective vaccines • Many viruses are not structurally plastic: e.g. poliovirus. One vaccination can confer lifelong immunity Structural plasticity: Antigenic variation The immune system detects “epitopes” on “antigens”: structural features of molecules • Antigenic variation: 2 o Changes in the epitopes of viral proteins that are presented to the immune system. • Antigenic drift: o Appearance of virions with slightly altered surface proteins following passage in the natural host. o An evolutionary process where natural selection is driven by the host immune response • Antigenic shift: o A major change in a surface protein as a gene encoding a completely new surface protein is acquired. o Results from coinfection of one host with two different viral serotypes. o Due to reassortment of genes among two or more viruses. o Very commonly seen with viruses having segmented genomes. o Reassortment and recombination of blocks of genetic information result in viral hybrids that are immunologically new to the host. Acute infections and Public Health Acute infections are commonly associated with epidemics e.g. polio, influenza, measles, common cold Main problem: by the time symptoms emerge, the patient has passed on the infection Difficult to control in large populations and crowded environments e.g. work, daycare, dorms Effective antiviral drug therapy requires early intervention, safe drugs with few side effects…..not really practical for acute infections. Cost: 90% of outpatient visits due to self-limiting acute viral infections. Persistant Infections. Four general classes. 1) Infection by viruses which actively produce large amounts of progeny, but which cause little cytopathology. 2) Infection by normally lytic virus but in which the extent of virus multiplication is somehow limited, so that the yield of virus is small. 3) Limitation of reinfection by various viral and cellular factors, so that the proportion of infected cells in the total cell population remains small but constant. Viral factors tend to be decreased virulence, and interference of virus production by defective interfering particles. Cellular factors include differences in permissiveness to infection/virus replication, and immune surveillance. 4) Chromosomal integration of proviral genomes Result in “silent” infections, infrequent or constant rounds of low level, and only slight production of cytopathic virus. Some persistent viral infections of humans (see Table 16.2) VIRUS SITE OF PERSISTENCE CONSEQUENCE Adenovirus Adenoids, tonsils, lymphocytes None known Epstein-Barr B-cells, nasophayngial epithelia Lynphoma, carcinoma 3 H.Cytomegalovirus Kidney, salivary gland, WBCs? Hepatitis B virus Liver, lynphocytes Hepatitis C virus Liver HIV CD4+ T-cells, macrophates, microglia HSV 1 and 2 Sensory and autonomic ganglia HTLV 1 and 2 T-cells Pneumonia, retinitis Cirrhosis, liver cancer Cirrhosis, liver cancer AIDS Papillomaviruses Skin, epithelial cells Polyomavirus BK Kidney Polyomavirus JC Kidney, CNS Papillomas, carcinomas Hemorrhagic cystitis Progressive multifocal leukoencephalopathy Subacute sclersoing panencephalitis Progressive rubella panencephalitis Shingles, postherpetic neuralgia Measoes CNS Rubella virus CNS Varicella-Zoster Sensory ganglia Cold sore, genital herpes Leukemia, brain infections Perpetuating a persistent infection by modulating the adaptive immune response: Blocking display of viral antigen in context of MHC class I (See Fig. 16.5). CTL response clears out virus infected cells Requires CD8 interaction with MHC class I molecules displaying viral peptides Blocking such display provides an advantage to a virus. Examples: o HIV Tat protein blocks transcription of MHC class I and of 2 microglobulin o hCMB US11 and US2 proteins route MHC class I protein out of ER to proteosome o HSV ICP47 blocks proteolytic processing of internal antigens by the proteosome o hCMV blocks transport of processed antigens to ER o Many viral proteins block transport of MHC class I/antigen complexes to golgi o HIV Nef protein directs MHC class I/antigen complexes from plasma membrane to the lysosome. MHC Class II modulation after infection Exogeneous antigenprocessing in the antigen-presenting cell: the pathway for MHC class II peptide presentation. (see Fig. 15.20) Antigen presenting cells – Macrophages, dendritic cells, B-cells. Gobble up antigens from outside, process them, present them to CD4 T-cells in the 4 context of MHC class II. Presentation of viral antigen in this contact activates T-helper cells, activating specific immune response. Any viral protein that can modulate the MHC class II antigen presentation pathway would therefore interfere with T-helper cell activation. Examples: HIV Nef: triggers rapid internalization of CD4 and MHC class I and II. EBV BZLF2: Physically blocks MHC class II molecules Killing activated CTLs Activated CTLs express the membrane-bound Fas receptor: related to TNF receptor Fas binds the Fas-Ligand (FasL) Binding of FasL on target cells by Fas on activated CTLs activates T-cell aptosis. Many viruses, e.g. HIV-1 increase expression of FasL on the surfaces of infected cells. Direct infection of cells of the immune system Allows viruses to suppress the immune response, e.g. HIV Mobility of immune cells allows viruses to disseminate through host – e.g. CMV Infections of tissues with reduced immune surveillance Tissues with surfaces exposed to environment Higher thresholds of immune activation, e.g. skin, glands, bile ducts, kidney tubules. o Cytomegalovirus infects cells on the surfaces of glands and ducts (kidney, salivary, mammary), ensuring constant shedding of new virus into environment. o Papillomaviruses: Productive replication of only occurs in the outer, terminally differentiated skin cells. The result is skin warts. Other compartments of the body can’t mount inflammatory responses To do so would be to severely damage them. e.g. CNS, eye, areas of lymphoid drainage. Persistent infection of these tissues by viruses is common. 5