Normal Tension Glaucoma
advertisement

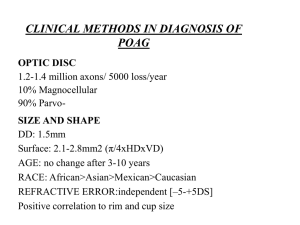
Normal Tension Glaucoma Joseph Sowka, OD, FAAO, Diplomate Normal Tension Glaucoma (NTG) IOP is within the "statistically normal" range. IOP consistently under 21 mm hg. Sometimes referred to as “low tension glaucoma”, “low pressure glaucoma” and “pressure independent” glaucoma Prevalence not truly known. Varies considerably - from 10% to > 50% (dependent upon study source). Prevalence is likely greatly over inflated NTG: The 3 Questions 1. Is the cupping physiologic or pathologic? Accurate visual fields as well as other optic nerve function and structure studies should identify truly diseased nerves. Misdiagnosis of megalopapillae 2. Is the cupping progressive? Serial or sequential optic nerve function and structure studies will identify progression. There are a host of masquerading conditions that present with field defects (e.g., tilted discs) that are non-progressive. You should not beat your head against a wall trying to treat a non-progressive anomaly. 3. If the cupping is pathologic and progressive, what is the optimal treatment? Virtually every therapy has alternately been both advocated and vilified NTG: Differential Diagnosis Congenital defects: optic nerve hypoplasia, tilted discs, optic pits and colobomas, large physiologic cup (megalopapilla), optic nerve drusen. Burnt-out POAG Hypovolemic optic neuropathy Arteritic and non-arteritic AION Diurnal variations in POAG Chronic angle closure glaucoma Compressive lesions: the neuroradiological fishing trip Non-glaucomatous optic neuropathy Previously high IOP IOP lowering systemic medications Beta blockers for HTN Other types of glaucoma (secondary) – particularly those with intermittent IOP spikes or wide diurnal IOP variations Pigmentary Exfoliative Glaucomatocyclitic crisis Steroid-induced “Masked POAG” - Abnormally thin cornea masking true ocular hypertension 1 70 um change in corneal thickness can approximate 5 mm Hg of IOP Clinical Pearl: Normal tension glaucoma is a diagnosis of exclusion. If the doctor works hard enough, most cases of “NTG” can be correctly ascribed to another disease. NTG: Risk Factors and Associated Factors: Peripheral vascular disease: if glaucoma is truly a vascular disease which is affected by elevated IOP to cause an optic neuropathy, then the patients who are severely vascularly compromised can possibly develop glaucomatous changes at “normal” pressures Age – disease mostly of elderly Probably just increased susceptibility to IOP related damage due to aging Family history of glaucoma Myopia Disc hemorrhages Raynaud’s phenomenon Vasospastic neuropathy? Migraine HA Vasospastic neuropathy? Low blood pressure Low OPP Hemodynamic crisis Hypovolemic optic neuropathy Carotid insufficiency Empty sella syndrome: DM and hypercholesterolemia Cardiovascular disease Abnormal blood coagulation and platelets Abnormal antibodies and other immune factors Most of these risk factors have a positive correlation, but unknown role. Collaborative Normal Tension Glaucoma Study (CNTGS) 1998 Randomized, controlled 5 year clinical trial (144 eyes) of the effectiveness of IOP reduction in slowing the progression of field loss in pts. with NTG. Inclusion criteria Showed documented progression, high risk field defects that threatened fixation, or appearance of new disc hemorrhage Goal: 30% reduction from IOP baseline Due to potential (theoretical) impact to optic nerve perfusion, adrenergic drugs such as beta blockers and epinephrine weren’t used. Alphagan and prostaglandins weren’t invented yet. Essentially, the only way that IOP was reduced in this study was with pilocarpine, laser trabeculoplasty, and trabeculectomy. Surprisingly, over half of the treated patients achieved the goal IOP reduction without having to undergo trabeculectomy. Results: 35% of control eyes (untreated) showed progression (glaucomatous optic disc 2 progression or visual field loss) whereas only 12% of treated eyes showed progression. Conclusion: Intraocular pressure is part of the pathogenic process of NTG. Therapy that reduces IOP and is free of side effects would be expected to be beneficial in patients who are at risk of disease progression. Problems: 1. Which patients are at risk for disease progression? 2. While 35% of untreated eyes showed progression, 65% of untreated eyes did not progress. Further Conclusions from CNTGS: Lowering IOP without producing cataracts is beneficial. Because not all untreated patients progressed, the natural history of NTG must be considered prior to embarking on IOP reduction with therapy apt to exacerbate cataract formation unless NTG threatens serious visual loss. According to the CNTGSG, those at risk of progression include: Females Those with history of migraines Those manifesting disc hemorrhage Factors that were not associated with an increased risk of progression include: Older age Higher mean IOP Field defects threatening fixation Factors associated with treatment benefit include: No disc hemorrhage Female gender Family history of glaucoma No family history of stroke No personal history of cardiovascular disease Less initial disc damage (C/D < 0.7/0.7) Factors not associated with treatment benefit include: Male gender Disc hemorrhage Severely damaged discs Migraine Clinical notes and curiosities: Asian patients have less severe disease than Caucasians Disc hemorrhage is strongly predictive of progression, yet doesn’t benefit from treatment Females gender is strong factor for having NTG, progression of disease, and benefit of treatment Female gender does NOT show up as risk factor in Ocular hypertension NTG: Pathophysiology Unknown Theories: Small vessel disease 3 Vasospasm Hemodynamic crisis (single event theory) Nocturnal hypotension Structurally weak lamina (collagen vasculopathy) New theory: autoimmunity 30% prevalence of systemic autoimmune diseases in NTG vs POAG and controls Immuno-pathogens may damage optic nerve, vessels, or both Patients with “NTG” have increased prevalence of monoclonal paraproteinemias Paraproteinemias are seen in patients with peripheral neuropathies ”NTG” may be organ-specific autoimmune disease Patients with “NTG” have increased prevalence of monoclonal paraproteinemias Paraproteinemias are seen in patients with sensory peripheral neuropathies (Wax et al. 1994 Am J Ophthalmol) Immunoglobin IgG, IgA (and other retinal antibodies) deposition found in RGC layer of patient with NTG and paraproteinemia (Wax et al. 1998 Arch Ophthalmol) Increased antiphospholipid antibodies (antiphosphatidylserine) in “NTG” vs POAG vs controls IgG anticardiolipin antibodies greater in “NTG” than POAG and controls (Kremmer et al. 2001 Clin Exp Immunol) Serum from NTG pts. contained high titres of antibodies against retinal proteins, including rhodopsin and heat-shock protein (HSP) Immune responses to HSP implicated in human autoimmune diseases HSP are significant autoantigens Antibodies to HSP found in many autoimmune disease NTG vs POAG Sharper field loss in NTG Shallower cupping in NTG Larger overall disc area in NTG Disc hemorrhages 5-fold more prevalent in NTG than POAG Higher and greater incidence of peripapillary atrophy and crescents in NTG than POAG NTG: Diagnostic Evaluation Diagnosis of exclusion R/O impostors Complete eye exam and history Pachymetry and gonio especially important Multiple IOP readings at different times of day General medical exam and neuro-evaluation Serial fields and photos Medical evaluation NTG: Medical Evaluation Vascular studies 4 Blood glucose CBC (Hyperviscosity/ anemia) B12 ANA ACE CXR FTA-ABS/ RPR Lyme Thyroid Mitochondrial DNA SPEP retinal antibodies Serum chemistries (lipids) ESR (erythrocyte sedimentation rate) Carotid blood flow studies Neuroimaging (if under age 65, rapidly progressing, unilateral, dyschromatopsia, acuity loss) of the orbits and chiasm. NTG may actually be a systemic disease with ocular manifestations Autoimmunity? This may be a self-limiting autoimmune disease that mimics glaucoma NTG: Management Determine progressive nature. If non-progressive, monitor. If progressive, reduce IOP by 30% (per CNTGS results) NTG: Management Prostaglandins are supported due to their ability to reduce IOP that is already within the statistically normal range with minimal adverse effects Alpha-2 adrenergic agonists and beta blockers theoretically may affect OPP adversely CAIs often not advocated due to poor IOP lowering potential in statistical normal range Trabeculoplasty and trabeculectomy Clinical Pearl: Do not rush to make this diagnosis. It should take at least 6-12 months in order to make the diagnosis when you insist on determining progression. Clinical Pearl: Glaucoma is glaucoma regardless of the pressure level. However, in the “normotensive” range, there is a great difference between an IOP of 19 mm Hg and 12 mm Hg in terms of management. Conclusion: “NTG” is a diagnostic garbage can in which many things are thrown. There may be a rare few patients who have true glaucoma at a statistically normal intraocular pressure. However, most of the patients diagnosed as “NTG” likely have congenital anomalies, other neuropathies, other types of undiscovered glaucoma, or a self-limiting neuropathy that mimics glaucoma and may have an autoimmune etiology. 5