Patient Education: About PEG Tubes
advertisement

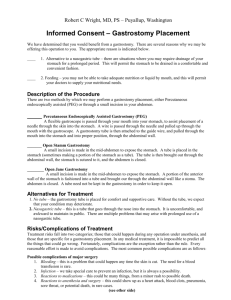
Patient and Caregiver Education on Gastrostomy/PEG Tube Placement What is gastrostomy feeding tube placement? Gastrostomy feeding tube placement is a procedure in which the surgeon creates an alternate entrance into the stomach. A tube is placed through the abdominal wall directly into the stomach, bypassing the mouth and esophagus. When done at the time of an operation it is called open gastrostomy tube placement. When performed with the aid of a lighted flexible scope it is called Percutaneous Endoscopic Gastrostomy tube insertion (or PEG). When are gastrostomy tubes used? Gastrostomy tubes are placed when patients cannot swallow or utilize the normal oral/esophagus route for food intake. This procedure is most often done for patients suffering from a stroke, an operation on the mouth, throat, or neck, or patients who have an altered state of consciousness and are not awake enough to use the normal swallowing mechanism. Gastrostomy tubes are sometimes placed to suction or aspirate stomach contents following surgery or if a patient is experiencing a bowel obstruction. Gastrostomy tubes allow for decompression of the stomach to prevent vomiting or aspiration pneumonia (regurgitation of stomach contents into the windpipe and lungs). When shouldn’t a gastrostomy feeding tube be used? Families and/or patients may choose not to have a gastrostomy tube placed, even though they cannot take food or medication orally. Sometimes patients weigh the risks of not being able to eat properly, complications of the tube placement, etc., and choose to accept the natural course of their underlying illness. A thorough discussion should take place between the patient, his/her family, and the surgeon before undertaking this procedure. How is a patient prepared for gastrostomy feeding tube placement? Arrangements are made for a patient’s post-operative care and recovery before the operation is performed. Patients are assessed by their physician with a history and physical examination. Occasionally, laboratory or special x-ray studies are performed to confirm the patient’s underlying problem or better identify their anatomy. Some patients will require a special swallowing study confirming their risk for abnormal swallowing and aspiration pneumonia. Some patients will require an upper GI x-ray to determine the anatomy of the upper gastrointestinal tract, particularly if the patient has undergone previous stomach surgery. The patient should rest and follow their physician instructions regarding nutrition and medications. Patients and their families should have a clear understanding about the risks and benefits of the procedure before proceeding. What happens during the procedure? Gastrostomy feeding tube placement is done in two basic ways. In the first, open gastrostomy tube placement is generally performed under general anesthesia. This procedure is often done at the time of another major operation in anticipation of postoperative need for emptying (decompressing) the stomach, or for future feeding. The second way, called percutaneous endoscopic gastrostomy (PEG) tube placement is usually done with sedation given in the vein and a local anesthetic applied to the back of the mouth. The procedure is done with the guidance of an endoscope placed through the patient’s mouth into their stomach. How is an open gastrostomy tube placement performed? Patients receive a general anesthetic. In the course of performing a major abdominal operation the surgeon will cut into the abdominal wall entering the abdominal cavity. This is called a laparotomy. During this procedure the stomach is exposed and a small incision is made in the wall of the stomach. The gastrostomy tube is placed through a small cut in the abdominal wall and into the stomach. A balloon on the end of the tube is inflated inside the stomach. Traction is placed on the tube to elevate the stomach against the abdominal wall where it is secured with sutures. Sometimes a second smaller tube is threaded through the stomach tube into the first part of the intestine. This is called a jejunostomy tube and is used to feed or administer medications to patients further down the gastrointestinal tract beyond the stomach. This smaller tube may reduce the risk of regurgitation or reflux of contents into the stomach, esophagus, and lung. Following the tube placement the abdominal wall incision is closed and the patient is taken to the recovery room. How is a PEG tube placement performed? Percutaneous endoscopic gastrostomy (PEG) tube placement is usually done with sedation given into the vein and a local anesthetic applied to the back of the mouth and throat. Patients generally sleep through the procedure and have no recollection of it having been performed. The surgeon will guide an endoscope through the mouth into the stomach. An endoscope is a long, narrow tube with a camera and light on the end. It lets your surgeon look directly into the stomach. The stomach is inflated with air. PEG tube systems involve placement of multiple Tfastener devices that pull the stomach up against the abdominal wall. External cotton plugs are secured on the outside of the abdomen and surround the tube site. These remain in place for two weeks while the body heals. A needle is then guided through the skin and abdominal wall into the stomach. This can be directly viewed through the endoscope to ensure proper placement. A wire is passed through the needle and grasped by the endoscope. Your surgeon will then place a plastic gastrostomy tube over the wire, through the abdomen, and into the stomach. The end of the tube is inflated and secured to the skin. Ultimately a permanent hole between the stomach and skin is created called a fistula which is maintained unless the tube is removed. Replacement tubes may be placed through the fistula when needed. What happens after the gastrostomy procedure? Following a gastrostomy tube placement patients are monitored in the recovery room. Some patients will recover and be discharged to their home, nursing home, or extended care unit. Other patients may need to stay in the hospital for one to three days based on their condition. Most PEG tube patients leave the same day. Instructions will be given to the patient’s caregiver regarding care of the gastrostomy tube. Decompression with suction to empty the stomach can be performed immediately. Generally gastrostomy tube feedings can be started within one or two days of gastrostomy tube placement. Patients and their caregivers are given instructions on how to care for their tube. Follow-up care will be performed by your doctor or caretaker, including examination of the gastrostomy tube site and removal of T-fasteners two weeks following the procedure. What are the benefits of gastrostomy tube placement? Most patients’ nutrition can be improved by ensuring proper amounts of protein, calories, supplements, minerals, vitamins, and fluids through the tube. Compliance with medication administration often improves. Patients may receive nutrition and medication even when they do not feel well and would normally not be eating or drinking properly. For those patients who undergo gastrostomy tube placement for decompression they often feel relief of abdominal bloating, gas, pain, distention, and cramps. This also reduces the risk of stomach reflux into the esophagus and trachea (windpipe). For some patients there is a decreased risk of aspiration and pneumonia. What are the risks associated with gastrostomy tube placement? The risks of this procedure include general anesthesia or sedation. Patients may need to have their tube changed periodically. The area around the tube may become infected after the operation. Infection or bleeding within the abdomen may occur. Internal organs (such as colon or small bowel) other than the stomach can be injured during tube placement and require surgical correction. Your surgeon should discuss the risks of the procedure and how they apply to a specific patient’s situation. When should I call the surgeon? Call your surgeon immediately if the tube comes out or is blocked. Your doctor should be notified if the patient experiences any fever, chills, nausea, vomiting, abdominal pain, distention, bleeding, or signs of skin infection at the tube site. What are the most common reasons for gastrostomy tube placement? Gastrostomy feeding may be indicated for patients with a functioning gastrointestinal tract who require long term tube feeding. This includes patients in whom malnutrition already exists, or may result, secondary to: Neurologic diseases resulting in an abnormality in swallowing. Tumors of the head, neck, or esophagus resulting in an abnormality in swallowing. Upper airway diseases/mouth, throat, or neck trauma resulting in an abnormality in swallowing. In addition, some patients who require either chronic supplemental fluids for hydration or chronic gastric decompression are candidates for gastrostomy tube placement. Who should not have a gastrostomy tube placed? Patients who should not undergo placement of a gastrostomy tube include those with a nonfunctioning stomach or bowel, excessive fluid in the abdomen, or an active untreated abdominal infection. High risk patients include those with known hiatal hernia, gastroesophageal reflux disease, a history of aspiration pneumonia, terminal cancer and morbid obesity. How will my gastrostomy tube be cared for? Each patient should receive instructions for the care of the gastrostomy tube. Abbreviated instructions are listed here: blue centimeter (CM) markings on the tube should be noted and maintained in their initial position. the patient is known to pull on tubes, soft restraints or mittens can be used or the tube may be secured below a dressing. skin around the tube and T-fastener sites can be cleansed daily with soap and water, hydrogen peroxide, or Povidone-iodine solution. The area under the skin disk can be cleaned with a cotton-tipped applicator. No dressing is necessary unless specifically instructed. gastrostomy tube should be flushed with 20 or 30 mL of warm water before and after each intermittent/bolus feeding or every three to four hours during continuous feeding. Also, the tube should be flushed before and after medication administration or after checking for residual gastric contents. head of the patient’s bed should be elevated at least 30 degrees while feeding. the stoma track between the skin and stomach matures (usually 14 days following placement) the sutures for T-fasteners can be cut at the skin level. This allows the 1 cm stainless steel “T” to pass into the stomach and bowel and out with the stool. The external portion of the suture and cotton plug is discarded. should become familiar with the gastrostomy tube and the use of a jejunostomy tube if it has been threaded through the gastrostomy tube. The small white side port on the gastrostomy tube still allows access to the stomach if a jejunostomy (orange or yellow tipped) tube is in place through the gastrostomy tube.