Sensory innervation of the digit is by four nerve branches
advertisement

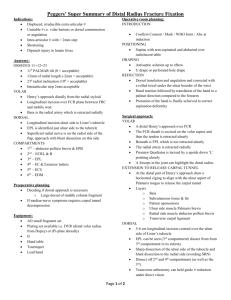
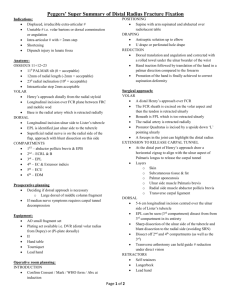
Title: Randomized Controlled Comparison of Two Common Digital Nerve Block Techniques Authors: Jason G. Williams, M.D., Donald H. Lalonde, M.D. Introduction: Sensory innervation of the digit is via four nerve branches, two dorsal and two volar. 1 Knowledge of this nerve distribution has led to development of many different techniques of digital nerve blockade with local anesthetic. These range from the classic dorsal block to the more recently described subcutaneous volar block, with myriad variations in between. As the digital nerve block is one of the most commonly performed procedures in the emergency department it is important for any physician managing hand injuries to be able to administer an effective, reliable and safe block. Previous studies have compared the effectiveness of various block techniques2,3,4, but none to date has compared the single injection volar subcutaneous block of Harbison5 to a traditional dorsal approach block. The purpose of this study is to compare these two techniques in terms of pain, reliability, duration or effect, and recipient preference. Materials and Methods: Approval of this study was granted by the Research Ethics and Review Board of the Saint John Regional Hospital, Saint John, New Brunswick. Twenty-seven volunteers were enrolled between July and September 2003. Informed consents were obtained from each individual. The subject was excluded if any medical contraindications to the procedure existed. A random number table was used to plan the injections. This randomized which finger was injected first (right or left) and which technique was used first (volar or dorsal). All injections were performed by the same physician (JGW) with standard technique (Figures 1 and 2). All injections were done using a reusable dental syringe with a 30-gauge needle, and 1.8 ml cartridges of 2% lidocaine with 1:100 000 epinephrine. Figure 1: Two-injection dorsal approach technique. Figure 2: Single injection volar approach technique The volunteers did not watch the procedure. Following each block, the subjects indicated the discomfort experienced on a 010 visual analog scale. After both blocks were completed, subjects were asked: “If you required a digital block in the future, which method would you prefer?” Thirty minutes after the injections, distribution of anesthesia was determined by pinprick testing. The areas were mapped and photographed. The duration of anesthesia was determined from the time of injection to the time that normal sensation returned to the fingertip. This was normally reported back to the investigators the following day. Results: Of the twenty-seven volunteers, there were 16 females and 11 males with a mean age of 31 (range 23-51). Occupations of the subjects included nurses, staff physicians, administrators, medical students and technicians. Whereas all volar blocks achieved complete fingertip anesthesia, two dorsal blocks failed to achieve complete anesthesia to pinprick. Pinprick testing also revealed that anesthesia over the dorsal aspect of the proximal phalanx was inconsistently achieved with the volar block. Separate two by two mixed ANOVAs were conducted to analyze the effects of sequence and procedure on the dependent variables of duration and level of pain. In each analysis the between subject variable was sequence of injection and the within subject variable was procedure. In the first analysis, duration for volar injection (mean = 417.32 min) was longer than the duration for dorsal injection (mean = 304.82 min) F (1,20) = 63.24, p<0.001. The mean level for rated pain was less for volar injections, 4.06 than for dorsal injections, 4.52. A binomial test revealed that the volar injection was preferred, p<0.05. 10 9 8 Pain (0-10) 7 6 5 4 3 2 1 0 Volar Dorsal Figure 3: Pain associated with digital blocks assessed on a 0-10 visual analog scale. There was no statistically significant difference in discomfort associated with volar versus dorsal approach digital blocks. 25 # of Subjects 20 15 10 5 0 Volar Dorsal Figure 4: Twenty-two out of 26 subjects preferred the single injection volar subcutaneous block to the two injection dorsal method. This difference is statistically significant, P<0.05. Discussion: Harbison described the volar subcutaneous block in 1991. 5 The block involved a single volar injection into the subcutaneous space over the flexor sheath. He reported this technique to carry all the advantages of the transthecal block described by Chui6, but was less painful and easier to administer. Subsequently, Low et al compared the subcutaneous block to the transthecal block in a randomized double-blinded study and confirmed that the subcutaneous block was as effective, but was easier to administer and caused less discomfort than the transthecal block. 2 Brutus et al also found the subcutaneous single injection block to be safe, efficient, and easy to perform. 6 Several authors consider the volar block preferable to the traditional dorsal block because it involves only a single injection, uses a small volume of anesthetic, and carries virtually no risk of direct nerve or vessel injury .2,6,7 The present study is the first to compare the volar subcutaneous block to a traditional dorsal technique. Our findings contradict classic teaching that volar blocks are more painful than dorsal blocks. In fact, we found no statistically significant difference in pain between the two methods. Moreover, 80% of our study participants preferred the volar block and would select this technique if given the option if a future digital block was required. Anesthesia of the proximal dorsal aspect of the digit was not consistently achieved with the volar block. This is consistent with the literature, and as suggested by previous authors, a secondary dorsal sensory nerve block may be necessary if procedures are planned over the dorsum of the proximal phalanx. 2,5,7 There were no complications in this series. Specifically, there were no adverse effects related to the use of epinephrine in our injections. The use of epinephrine is likely responsible for the long duration of effect of both the volar (7 hours) and dorsal (5 hours) blocks. Conclusion: The single injection volar subcutaneous digital block is an easy to administer, safe, reliable, and effective block that is longer lasting, no more painful, and preferred by 80% of subjects to the traditional two injection dorsal digital block. References: 1. Ramamurthy S, Hickey R: Anesthesia, Green, DP, Hotchkiss RN, Pederson, WC (ED): Green’s Operative Hand Surgery, Fourth Edition, Philadelphia, Churchill Livingston, 1999, Chapter 2, pages22-47. 2. Low CK, Vartany A, Engstrom JW, Poncelet A, Diao E: Comparison of transthecal and subcutaneous single-injection digital block techniques; J Hand Surg; 22A;901-905;1997. 3. Hill RG, Patterson JW, Parker JC, Bauer J, Wright E, Heller MB: Comparison of transthecal digital block and traditional digital block for anesthesia of the finger; Ann Emerg Med;25;604-607;1995. 4. Cummings AJ, Tisol WB, Meyer LE: Modified transthecal digital block versus traditional digital block for anesthesia of the finger; J Hand Surg; 29A;44-48;2004. 5. Harbison S: Transthecal digital block: flexor tendon sheath used for anesthetic infusion (Letter); J Hand Surg; 16A; 957;1991. 6. Chui DTW: Transthecal digital block: flexor tendon sheath used for anesthetic infusion; J Hand Surg; 15A;471-473;1990. 7. Brutus JP, Nikolis A, Baeten Y,Chahidi N, Kinnen L, Ledoux P, Moermans JP: Reducing patient discomfort during digital blockade: the subcutaneous single injection digital block- a simple, safe and fast procedure; Can J Plastic Surg; 11(1);3335;2003.