(SIG) Grant Proposal - Chronic Pain Scotland
advertisement

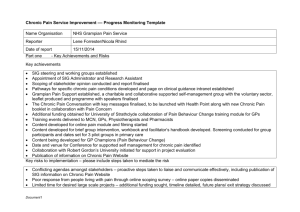
NHS Grampian 1 Chronic Pain Service Proposal Chronic Pain Service Proposal NHS Grampian This proposal seeks Scottish Government Health Department funding to support a two year programme of service improvement to more effectively and efficiently meet the increasing need presented by people with chronic pain. In order to achieve this aim, we perceive the main task at hand be to develop a biopsychosocial self management model of care in the community and up skill the knowledgebase of key functions across primary care and as such improve the services at Level One of a Tiered model of care, which we perceive as being the currently least developed Tier within the field of chronic pain. This would entail making sure that patients’ get the earliest possible and most appropriate treatment locally, but with ready access to specialist services when needed, in line with the Scottish Service Model for Chronic Pain and forthcoming SIGN Guideline. For a self management approach to be successful, it is crucial to deliver it in a way that is acceptable to patients and does not make them feel that they are receiving an inferior service, and as such the implementation of this we think will have to be by very specialist staff. For any changes to services to be truly evidence based, we further wish with support from specialist academic staff to evaluate all projects to a high scientific standard, so that the effectiveness and efficiency of all projects can be demonstrated within a scientist-practitioner model, both to make sure that the changes implemented are of clinical benefit and to due this opportunity to add to the evidence base within the field of chronic pain management more widely. In order to achieve our aims, and thereby allowing as many patients as possible to be treated in the community, we believe there is a need to both up-skill primary care staff and develop Tier One pain services as a viable and preferable alternative, fully utilising established and evidence-based self management approaches. We envisage this to take the form of a multi-stranded approach involving complementary streams, training primary care staff in chronic pain management and self management and psychosocial aspects of chronic pain, involving both communication that support and encourage patients towards an understanding of their pain as a phenomena that requires self management and developing a service that delivers upon the key elements of quality, being safe and sustainable, clinically effective and patient centred. NHS Grampian 2 Chronic Pain Service Proposal NHS Grampian Service The local service is based in Aberdeen and provides a specialist Chronic Pain Consultant service which is made up presently of 3 Consultants, a Clinical Fellow, a Psychologist, a Psychiatrist, a specialist physiotherapist and specialist nursing. The local service has been under significant pressure over the last 2 years with transfer of the Elgin service to Aberdeen. The service is extremely keen to develop links with primary care in a way that bridges the gap between tier one and two as detailed in the Scottish Service Model for Chronic Pain. The service provision that is lacking is this bridge between what GPs provide and the specialist interventions. There are significant numbers of patients who presently don’t get the best service due to lack of resources and alternatives to offer the patient in their journey of accepting their long term condition and how they will cope. It is widely accepted there is no new funding and we need to make better use of what allocation already exists. This is about shifting the care to the right setting with the right support at the right time for each patient. NHS Grampian’s strategic development plans will enable our aims to be achieved as our clinic activity relocates to a new purpose built facility in December 2013, The Health Village. The ethos of this community based facility is to maintain the patients well within the community. It will house some key secondary care services that have a heavy patient group that fits this ethos alongside social work, voluntary sectors and other support networks to help integrate these with patients and clinical teams raised collective awareness and collaboration improving the range and quality of services to patients. Proposed Developments 1. Primary Care educational package To scope the requirements for Pain education across Primary Care to assess the needs of GPs, Physiotherapists and district nurses and other interested parties. From this initial work establish the most effective delivery method that will provide the greatest impact to the broadest audience and test this. This could be the GP scholarship scheme or a primary care based package. The initial work will establish the direction and content of the programme that will follow. 2. Tier one pain service project Rolling out an online Level One, self management course; Pathway Through Pain Developing a manual for self management in chronic pain, pulling together relevant information in an accessible format utilising the web-based educational resources developed by the National Steering Group for Chronic Pain Delivering a brief, structured multi-disciplinary self management/educational group intervention in a community setting for patients referred, aimed at reducing the rate of subsequent requirement of secondary care pain service services 3. Practice-Based Community Project Development of a Chronic Pain Toolkit for first line management that can be launched as a tool accessible to all healthcare professionals to use including health point staff, with appropriate sign posting accessible online and in print with links for GPs and NHS Grampian 3 Chronic Pain Service Proposal Physiotherapists, involving a directory of resources, e-Health and the third/voluntary sector of available and appropriate pathways across the four tiers. Launch to include training of health point staff in the use of toolkit. Through the initial scoping exercise we may alter focus depending on the findings but the overall direction will not alter. Our ambition is to use this opportunity as a test of change and demonstrate the impact of these activities with a view to continuing the programme in the future. Resources The project will be managed formally with auditable minutes and actions shared with the National Scottish Pain Steering Group. The specialist team supporting these developments will be: Band 8b Clinical Psychologist/Lead- Dr Lene Forrester Band 8a Specialist Physiotherapist – Mrs Nicola Rhind Consultants – Prof Chambers/Dr Kanakarajan/Dr Nagaraja Practice GP – to be identified Specialist/Research Nurse/Assistant – to be recruited Admin/secretarial support – to be recruited Christine Leith/ Tara Murray - Management support Health Economist – Dr Paul McNamee, Health Economics Research Unit, University of Aberdeen GP Advisor with special interest/expertise in pain – Dr David Watson An extended team will be identified as part of this scoping exercise to include patients and representatives from the third sector. In addition governance arrangements will be ensured through the involvement of a non executive representative from the board. The aim of the wider group is to test the scope and delivery methodology will deliver our agreed objectives. All our projects will be evaluated to a high scientific standard in order that they provide an evidence base for service change. This will be achieved with support from specialist academic staff in order that effectiveness and efficiency can be demonstrated within a scientistpractitioner model. This will ensure that proposed changes are of clinical benefit. This will further add to the evidence base within the field of chronic pain management more widely. The projected expenditure against each resource may well alter depending on the initial scoping exercise but will remain within the overall budget. A full and transparent process will be audited to detail revised plans and what each resource will deliver for the funding allocated. Monitoring, Reporting & Evaluation Expected Outcomes Service users and their carers will have a better understanding of chronic pain as a long term condition requiring self management Services users and their carers will have local access to self management tools and training earlier in their care Up to date and comprehensive information on local services is readily available and accessible Service users receive a multidisciplinary assessment early in their care NHS Grampian 4 Chronic Pain Service Proposal Staff who are involved in the care of patients with chronic pain are more knowledgeable and confident in advising and supporting them Staff will be more aware of how and when to access further support when needed Resources are used effectively. Patients are referred and move through pathways appropriately Current and new sources of local self care education (e.g. Pain Association Scotland courses) are supported on an ongoing and sustainable basis Achievement of access targets at all stages of the pathway Measurement of the expected outcomes before, during and after the programme will allow the programme to be evaluated. Timescales and interim goals will be further developed and the monitoring and reporting progress be implemented.