Blue Box Stuff from Moore
advertisement

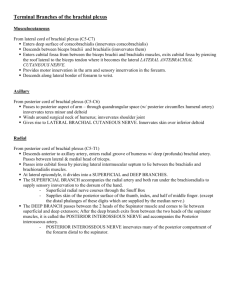
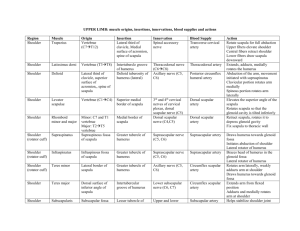
Blue Box Stuff from Moore The Upper Limb The structure of the scapula: anterior – subscapular fossa; posterior – supraspinatous and infraspinatous fossae; articulates with the clavicle at the acromion; has a coracoid process where several muscles (coracobrachialis, pectoralis minor) attach. The structure of the humerus: the head goes into the glenoid fossa of the scapula, just inferior to the acromion. There is the greater tubercle, which is lateral and serves as the attachment for the supraspinatus, infraspinatus, and teres minor muscles. The lesser tubercle is anteromedial and is the attachment for the other muscle of the rotator cuff, the subscapularis. There are tuberosities, which serve as attachments for the deltoid and brachialis muscles, more distal on the anteromedial surface of the bone. At the distal end are the lateral and medial epicondyles. The humeroulnar and humeroradial joint facets are made up of the capitulum, on the radial / lateral side, and the trochlea, on the ulnar / medial side. Posteriorly the olecranon fossa lies in-between epicondyles. The structure of the ulna: The coronoid process is on the proximal, anterior surface, while the olecranon process is on the proximal, posterior surface. It looks like a wrench, sort of. Distally lies the styloid process of the ulna, which actually attaches on the medial surface of the radius (the styloid process of the ulna articulates with the wrist). The structure of the radius: The head of the radius articulates with the capitulum of the humerus, while its styloid process is attached to the wrist. The clavicle is most commonly fractured in the lateral third, medial to the coracoclavicular ligament. The sternocleidomastoid contracts and elevates the medial fragment, while the latissimus dorsi and pectoralis contract and bring the lateral fragment medially. The arm sags because the trapezius supports all of its weight. Patients with broken clavicles present with upper limb supported / in a sling. Nerves The radial nerve runs on the posterior aspect of the arm, runs anteriorly around the lateral epicondyle, then wraps back posteriorly in the forearm, piercing the supinator, to become the posterior interosseous nerve. It branches into the deep (motor) and superficial (sensory) radial nerves. Injury results in anesthesia to the lateral half of the dorsum of the hand, and in loss of extension and abduction of wrist and extension of fingers wrist drop. The ulnar nerve runs on the medial aspect of the arm, wraps posteriorly around the medial epicondyle, where it is liable to be bumped, then passes between the two heads of the flexor carpi ulnaris,. It too divides into superficial and deep branches. Injury results in impaired flexion and adduction of the wrist, and loss of abduction / adduction of the fingers, especially the fifth digit (hypothenar compartment). Loss of sensation occurs to the hypothenar compartment and the medial half of the dorsum of the hand. Patients presenting with ulnar nerve damage cannot flex their fourth and fifth fingers (paralysis of medial half of flexor digitorum profundus and hypothenar muscles). The median nerve pretty much runs as its name implies, passes through the two heads of the pronator teres muscle, then dives in between the flexor digitorum superficialis and the flexor digitorum profundum in the forearm. Injury to this nerve results in loss of sensation to the lateral palmar side of the hand and paralysis of wrist and finger flexors, especially thenar muscles and the second and third digits. This is due to the fact that the median nerve innervates only the lateral half of the flexor digitorum profundus. It can also get trapped between the two heads of the pronator teres, causing pain in the proximal anterior portion of the forearm. Injuries to the brachial plexus are many and complex. Injuries to the superior parts of the plexus usually result from separation of the neck and shoulder. The roots of C5 and C6 may be pulled out of the spinal cord. The suprascapular, axillary, and musculocutaneous nerves do not function. The supraspinatus and infraspinatus (lateral rotation of arm), deltoid and teres minor (abduction), and biceps brachii and brachialis (flexion) are paralyzed. This disorder, known as Erb’s palsy, results in a characteristic “waiter’s tip” presentation of the patient – pronated, medially rotated, and extended. The lateral aspect [lateral antebrachial cutaneous] of the arm is numb. Poorly fitting crutches may injure the posterior cord of the plexus, damaging the radial nerve. The triceps and extensors of the wrist are paralyzed, and unopposed flexion causes characteristic “wrist drop.” Patient also cannot extend their elbow, wrist, or digits. Injury to the inferior roots of the plexus may occur if an infant’s shoulder is pulled during birth or if someone grabs something to stop a fall. The inferior trunk is damaged, and the ulnar nerve loses function. This results in impaired finger flexion, abduction, and thumb adduction. Also the median brachial and antebrachial cutaneous nerves lose function, resulting in numbness of the medial aspect of the arm, forearm, and hand. Injury to the long thoracic nerve can result from a stab wound, mastectomy, weight lifting, surgery, or carrying a heavy object on the shoulder. The serratus anterior [protraction of scapula] loses function, resulting in wing scapula, where the medial edge of the scapula protrudes posteriorly, away from the thoracic wall. The patient cannot abduct the arm above horizontal, nor can they push with their arm. Injury to the axillary nerve can result from fracture of the humerus, or dislocation of the shoulder joint. The deltoid atrophies, leaving flatness on the lateral proximal side of the arm. The patient cannot abduct the arm. injury to the thoracodorsal nerve can result from operations of the axilla. Injury results in paralysis of the latissimus dorsi. Arteries and veins The subclavian artery first sends off a vertebral branch superiorly, then a thyrocervical trunk superiorly and an internal thoracic artery inferiorly. Once it crosses the first rib, it is named the axillary artery. The first branch of the axillary artery is the supreme intercostal [1 st and 2nd intercostal spaces]. It is followed by the thoracoacromial artery [deltoid, pectorales, and various other areas.] The next branch is the lateral thoracic artery [lateral portion of the breast], then the subscapular artery [anterior surface of the scapula], and the posterior and anterior circumflex humeral arteries [head and neck of humerus]. *The posterior circumflex humeral and axillary nerve both enter the quadrangular space of the arm. The axillary vein is large and lies anterior to the axillary artery. These two, along with the brachial plexus, are enclosed in the axillary sheath. Anastamosis: If the axillary artery is ligated in between the thyrocervical trunk and the subscapular, blood can still flow distally through anastomoses. Blood flows from the dorsal scapular branches of the transverse cervical artery [a branch of the thyrocervical trunk] into the first few intercostal arteries, which anastomose with the circumflex scapular branch of the subscapular. Blood flows up through the subscapular artery into the rest of the axillary. Laceration of the brachial artery can result from a broken elbow. This is an emergency because the damage to the flexors of the fingers can be irreversible, resulting in formation of scar tissue and permanent contracture of the digits. The brachial artery divides into the ulnar and radial artery, with the ulnar artery branching into the ulnar and common interosseous arteries. The common interosseous artery branches further into anterior and posterior interosseous arteries. The hand A fall on the hand may fracture the distal end of the radius, resulting in a “Colle’s fracture.” The distal fragment of the ulna is displaced posteriorly and the hand looks sort of like a fork. The scaphoid bone is also often fractured breaking a fall, and results in tenderness of the base of the anatomical snuff box. The “anatomical snuff box:” bounded by the tendons of the extensor pollicis longus superiorly, extensor pollicis brevis and abductor pollicis longs inferiorly. Within it are contained the radial artery and the superficial radial nerve. Tendinitis of the common flexor tendon can result from repetitive use of the flexors, and pain is experienced on the anteromedial side of the elbow, where the flexor tendon is located. Patients will have trouble flexing their fingers against resistance. Tendinitis of the common extensor tendon, located on the posterolateral aspect of the elbow, results in pain when supinating and extending the digits. Patients will have difficulty extending their fingers against resistance. . Infections in the hand are limited to the compartment they begin in, unless they break through intercompartmental septa. Thus, most are localized to the thenar, hypothenar, or adductor compartments of the hand. They can, however, spread distally through the wrist into the forearm. Infections of a tendinous sheath of one finger will generally stay in that sheath unless neglected. The abductor pollicis brevis/ digiti minimi is most lateral / medial (respectively) and superficial. Medial / lateral to that is the flexor pollicis brevis / digiti minimi, and deep to both is the opponens pollicis / digiti minimi. The lumbricals are innervated by either the median (II and III) or ulnar (IV and V) nerves, and flex the metacarpophalangeal joints / extend the interphalangeal joints. The interossei are innervated by the ulnar nerve and adduct (palmar) or abduct (dorsal) the fingers about the middle finger. Carpal tunnel syndrome is characterized by compression of the median nerve within the carpal tunnel. Patients present with tingling of the lateral aspect of their hand, and a loss of coordination of the thumb due to weakness of the muscles of the thenar compartment. The second and third fingers, too, may lose function the disorder is severe enough. The shoulder area The sternoclavicular joint is the only attachment of the upper limb to the axial skeleton. It is enclosed in an articular capsule, and like the temporomandibular joint, contains an articular disc which gives it freedom of rotation. It is anchored to the first rib by the costoclavicular ligament laterally and the sternoclavicular ligament medially. The joint is very sturdy and the clavicle will break before the joint dislocates. The acromioclavicular joint is also enclosed in an articular capsule. It is anchored by the coracoacromial, acromioclavicular, and coracoclavicular ligaments. When these ligaments rupture from a hard fall on the shoulder, the joint can dislocate. The shoulder will fall away from the clavicle due to the weight of the upper limb. The shoulder joint is made up of the articular surface of the humerus and the glenoid fossa of the scapula. The fossa is very shallow but is deepened somewhat by a rim of fibrocartilage named the glenoid labrum. The four rotator cuff muscles provide most of the stability for this joint, which is prone to dislocation and other injuries due to its degree of mobility. There are many bursae in the region but Moore especially mentions the subacromial bursa, which lies in between the acromion and the tendon of the supraspinatus on the superior aspect of the joint. Inflammation of this bursa (bursitis) causes pain only when the arm is abducted – the tendon is in contact with the acromion only then. Anterior dislocation of the shoulder joint is caused by excessive extension and lateral rotation of the humerus. The head of the humerus is driven anteriorly and the joint capsule and glenoid labrum are torn off the fossa. Quarterbacks who are hit forcefully on the arm as they are about to release the ball; i.e. when their shoulder is fully abducted, will tear the joint capsule so that the humeral head will lie inferior to the glenoid cavity. Patients will present with the injured arm rotated anterosuperiorly (forward, medially rotated) under the coracoid process, holding the nonfunctional arm with their other arm. One must suspect damage to the axillary nerve in a shoulder dislocation because it lies very close to the inferior aspect of the joint capsule. The elbow joint This joint is not stable in children due to incomplete ossification. Separation of humeral, ulnar, or radial epiphyses can occur when a child falls on his / her elbow. Dislocations tend to occur posteriorly because the humerus is pushed through the weaker anterior portion of the humeroradial / humeroulnar joint capsule [think this one through]. The medial epicondyle of the humerus also ossifies late, and can be avulsed in a fall. It will be pulled distally due to traction of the ulnar collateral ligament. Since the ulnar nerve passes through this region, avulsion of the medial epicondyle can also stretch this nerve and cause difficulties flexing digits IV and V and adducting the wrist. If someone is holding a child’s hand and suddenly tugs it, an injury known as subluxation is likely to occur. The sudden force on the forearm tears the distal attachment of the annular ligament of the radius. The head of the radius is then pulled distally, out of the torn ligament. The poor child will present with his / her elbow flexed and forearm pronated. The wrist and hand I have no good mnemonic for the eight carpals. I tend to remember starting from the “Thumb Side” – the most lateral carpals are the Trapezium and the Scaphoid. Proceeding medially from the trapezium are the trapezoid, capitate, and hamate. Doing the same from the scaphoid are the lunate, triquetrum, and the pisiform. I guess you can also remember that the Pisiform is on the Pinky side of the hand. I dunno, whatever works best for you. A broken scaphoid bone results in tenderness of the anatomical snuff box. With the exception of the thumb, digits have one metacarpal and three phalanges. The metacarpophalangeal joints are capable of flexion / extension, ab / adduction, and rotation. The interphalangeal joints can only flex / extend. The carpometacarpal joint in the thumb is the joint capable of fl / ex, ab / ad, and rotation, while the metacarpophalangeal and interphalangeal joint fl / ex. Sudden tension on an extensor tendon may avulse part of its attachment. Patient will present being unable to extend the distal interphalangeal joint. Case Studies 6-1 … Check the description of injuries of the brachial plexus. 6-2 … Check the description of a dislocated acromioclavicular joint. 6-3: The lack of response to pinprick on digit V and medial border of palm indicates that the ulnar nerve, which supplies sensation to this area, is damaged. This is corroborated by the lack of finger adduction strength in the boy’s hand (caused by impaired palmar interossei). The boy would probably also have lack of finger abduction strength (dorsal interossei), impaired flexion of digits IV and V (medial flexor digitorum profundus), and impaired wrist flexion and abduction (flexor carpi ulnaris). Prognosis for recovery is good, as the nerve was not severed. 6-4: Wrist-drop and lack of sensation to the lateral half of the dorsum of the hand is screaming “Radial nerve damage!!” Elbow flexion would be impaired if the forearm was midway between supination and pronation, as the brachioradialis (“hand shake muscle”) is responsible for elbow flexion in this situation; it is innervated by the radial nerve. The humerus is shortened because the biceps, brachialis, and triceps contract to immobilize the ends of the broken bone. The radial nerve is prone to injury at the lateral aspect of the arm, midway down, because it lies right next to the humerus 6-5: The trapezium and scaphoid lie in the floor of the snuff box, along with the distal end of the radius. The scaphoid was most probably fractured. 6-6: The tendon of the palmaris longus was probably severed, as well as the flexor carpi radialis. Her median nerve was definitely severed; the lack of thumb opposition, fine control of digits II and III, and lack of sensation over the lateral half of the palm demonstrate deficits in median nerve function [opponens pollicis, the first two lumbricals, and sensory innervation to the lateral palm are provided by the median n.] Her superficial radial artery was probably severed; wrist flexion would be affected a bit by the severing of her palmaris longus, which attaches to the palmar aponeurosis. Her wrist will probably adduct when she flexes it, due to the unopposed action of the flexor carpi ulnaris. 6-7: The lady’s ulna styloid process was probably fractured, and with muscle contraction, brought to the same level as the radial styloid process, which makes the wrist look like a fork (Colle’s fracture). The scaphoid, again, was probably fractured in this fall.