Forearm compartment syndrome: an incision
advertisement

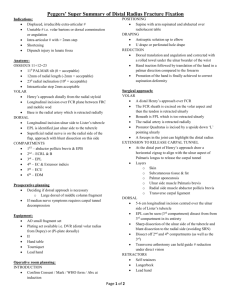
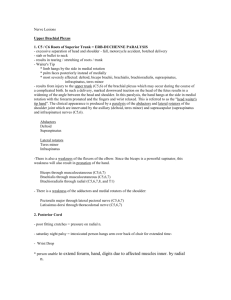
Anatomic Analysis of Surgical Approaches to the Deep Volar Forearm Daniel N. Ronel, MD, Estomih Mtui, MD, William B. Nolan III, MD Forearm compartment syndrome is a surgical emergency that requires release of the superficial muscle compartments. In some clinical situations it is imperative to also explore the deep muscle compartments, such as in cases of high-voltage electrical injury, severe crush injuries, extended extrinsic pressure (such as an unconscious patient lying on their own forearm), and when there is ongoing sepsis or suspicion of necrotic muscle despite previous fasciotomy.1-4 In some cases, even after compartment fasciotomy, the epimysium of individual muscles must be incised to relieve persistently elevated tissue pressure.5 This can only be achieved with adequate visualization of the deep space. If epimysiotomies of the deep muscles are not performed in these situations, necrosis and contracture may result. There are no anatomical guides for surgical exploration of the deep compartments that would minimize collateral damage to surrounding vessels, nerves, and muscles. Anatomical textbooks do not delineate the dominant vascular pedicles within the deep space in enough detail to plan a safe surgical approach. Surgical injury in the setting of ischemia, especially vascular injury, compounds the tissue damage that has already occurred. Three standard approaches to the deep forearm have been described, either in the context of fractures or of nerve compression. These ulnar, central, and radial approaches do not attempt to minimize iatrogenic trauma to small arteries, because they are not described in the setting of forearm ischemia. In the Henry approach to the anterior radius, for example, the recurrent radial vessels are ligated. Incisions described for the treatment of compartment syndrome often criss-cross the forearm or gently sweep across it in various directions (Figure 1). Incisions that cross the forearm will transect more of the venous and lymphatic return than will a straight incision, and the resolution of forearm edema could be impaired. Such incisions may also prevent the future design of a radial forearm flap, as the vascular supply and outflow of the skin pedicle would be compromised. Figure 1. Forearm incisions. Modified from Gelberman, et al (with permission). Method: We evaluated four surgical approaches to the deep forearm by performing detailed anatomical dissections on embalmed and plastinated cadavers. In the radial approach the skin incision was made radial to the midline of the volar forearm, starting at the proximal wrist crease and extending to the antecubital fossa. The superficial fascia was released and the dissection continued radial to the FCR and between the FCR and the FDS. In the central approach the skin incision was made over the center of the volar forearm. The superficial fascia was released and the deep dissection continued either radial or ulnar to the palmaris longus and then between tendons of the FDS. In the ulnar approach the skin incision was made radial to the FCU at the wrist and extended to the medial epicondyle of the humerus. The superficial fascia was released and the dissection continued radial to the FCU, between the FCU and the FDS. We used a scoring system to rate the approaches for their ability to visualize the deep space without causing iatrogenic injury to superficial muscles, arteries, and nerves (Table 1). Each element was scored on a scale of 1 – 3, with 1 being the best (the least damage was caused by the surgical approach) and 3 being the worst (the most damage was caused by the surgical approach). In the category of muscle injury, the surgical approach scored a “1” if there was no muscle injury, a “2” if sharp dissection of muscle was required to access the deep space, and a “3” if the division of a superficial muscle was required. For arterial injury, the surgical approach scored a “1” if no arterial branches were divided, a “2” if less than 50% of the segmental branches to any muscle were divided, and a “3” if more than 50% of the segmental branches to any muscle or if a dominant pedicle was divided. For nerve injury the surgical approach scored a “1” if no dissection around a motor nerve was required, a “2” if dissection around a motor nerve was required, and a “3” if division of a motor nerve was required. Table 1: Surgical approach scoring system Muscle injury score Criterion 1 No muscle injury 2 Sharp dissection required 3 Division of superficial muscle required Arterial injury score Criterion 1 No arterial branches divided 2 Less than 50% of segmental branches to any muscle divided 3 More than 50% of segmental branches or a dominant pedicle to any muscle divided Nerve injury score Criterion 1 No dissection around a motor nerve required 2 Dissection around a motor nerve required 3 Division of motor nerve required Results: Each surgical approach easily allowed the release of the superficial volar compartment. In the radial approach, the FDS impeded access to the deeper forearm in all the specimens. Division of the origin of FDS III was necessary to evaluate the FPL and FDP muscles (Figure 2, left). Segmental branches from the radial artery to the FCR impeded deep dissection in all the specimens (Figure 2, right). There was no significant injury to motor nerves. Figure 2. Radial approach. Left: access to the deep space requires division of the FDS. Right: branches from the radial artery to the FCR impede deep exploration. In the central approach it was difficult to separate the proximal fibrous raphe of the palmaris longus from the FCR or the FCU. Sharp dissection of the raphe or division of the FDS was required to reach the FPL and FDP. The division of several arterial branches from the ulnar artery to the FDS was required in 70% of the specimens (Figure 3, left). Dissection through and around the FDS was adjacent to motor nerve branches from the median nerve in 60% of the specimens (Figure 3, right). Figure 3. Central approach. Left: there is no plane in the proximal FDS, it is difficult to separate the FCR or FCU from the palmaris, and ulnar artery branches to the FDS impede deep access. Right: sharp dissection around median nerve branches to the FDS is required. In the ulnar approach, the PQ was reached between the ulnar artery and the FDS. One or two distal segmental arterial branches to the FDS and/or the FCR required division in 50% of the specimens (Figure 4, left). As the dissection moved proximally, the remainder of the deep compartment could easily be seen if the ulnar neurovascular bundle was raised with the FDS (Figure 4, right). This approach spared all proximal segmental branches to the FCR and FDS. In two specimens, one segmental branch to the distal FCU was divided. No dissection of superficial muscles or motor branches was required with the ulnar approach. Figure 4. Ulnar approach. Left: access to the PQ only requires division of one or two branches from the ulnar artery to the FDS. The scissors are under the fascia of the PQ, which is easily divided. Right: the deep compartment is easily seen in the interval between the FDS and FCU. The radial approach scored an average of 6.1 (SD 0.32); the central approach scored an average of 5.8 (SD 0.63), and the ulnar approach scored an average of 4.0 (SD 1.05). Using the Mann-Whitney test for non-parametric data (U statistic = 5.8656), the ulnar approach caused significantly less surgical trauma than the radial approach (p < 0.001, z = 4.0701) and the central approach (p < 0.003, z = 3.4349). Table 2: Comparison of surgical approaches Approach Average score* SD Radial 6.10 0.32 Central 5.80 0.63 Ulnar 4.00 0.05 *Lowest possible score (safest approach) = 3 Highest possible score (least safe approach) = 9 Conclusion: In the volar forearm, an ulnar approach to the deep space is simple, causes the least surgical injury, and provides access to the deep structures. The skin incision is similar to that described by Matsen, which extends from the medial epicondyle to the flexor crease of the wrist.2 The superficial compartment along the radial side of the FCU is opened distally, which reveals the ulnar neurovascular bundle. The muscle is retracted ulnarly, and the plane of dissection between the FCU and the FDS can be appreciated. The PQ can be seen distally between the ulnar neurovascular bundle and the FDS: one or two branches from the ulnar artery to the FDS may need to be ligated in order to release the PQ. Moving proximally, the ulnar neurovascular bundle is raised with the FDS to preserve its branches to that muscle. Although a branch from the ulnar artery to the FCU may need to be ligated, the FCU receives most of its blood supply via a dominant pedicle from the posterior ulnar recurrent artery. Raising the FDS in the middle third of the forearm allows easy access to the remaining muscles of the deep volar compartment, the FPL and the FDP. Exposure of the three deep muscles allows their evaluation for ischemia and, if needed, individual epimysiotomy. This approach to the deep space requires no sharp dissection. References 1. Gelberman, R.H., Zakaib, G.S., Mubaral, S.J., Hargens, A.R., and Akeson, W.H. Decompression of forearm compartment syndromes. Clin. Ortho. Rel. Res. 134: 225-9, 1978. 2. Matsen III, F.A., Winquist, R.A., and Krugmire, R.B. Diagnosis and management of compartmental syndromes. J. Bone Joint Surg. 62A: 286-91, 1980. 3. Rowland, S.A. Fasciotomy: the treatment of compartment syndrome. In Green, D.P., Hotchkiss, R.N., and Pederson, W.C. (Eds.), Green’s Operative Hand Surgery, 4th Ed. New York: Churchill Livingstone, 1999. Pp. 689-710. 4. D’Amato, T.A., Kaplan, I.B., and Britt, L.D. High-voltage electrical injury: a role for mandatory exploration of deep muscle compartments. J. Natl. Med. Assoc. 86: 535-7, 1994. 5. Eaton, R.G, and Green, W.T. Epimysiotomy and fasciotomy in Volkmann’s contracture. Ortho. Clin. North. Amer. 3: 175-86, 1972.