1. Identification of Patient
advertisement

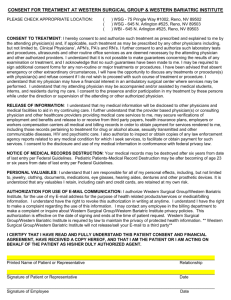
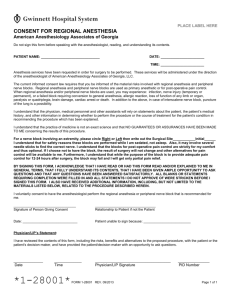
Medical Staff Bylaws, Part C RULES AND REGULATIONS OF THE MEDICAL STAFF I. ADMISSION, DISCHARGE AND TRANSFER OF PATIENTS The hospital shall accept patients for care and treatment except for direct abortion, elective sterilization and artificial insemination. The hospital shall accept on an emergency basis only a) acute alcoholic intoxication with acute complications, and b) drug addiction. Patients whose condition cannot be further improved by acute hospitalization should be discharged to an appropriate lower level of care setting such as a skilled nursing facility, intermediate care, personal care home, or to their homes. Staff members shall make referrals or arrange transfers (consistent with applicable law) to other hospitals or appropriate care settings for those patients whose needs cannot appropriately be met at the hospital. A. Admissions 1. Admission Criteria A patient shall be admitted to the hospital only by a member of the medical staff. All practitioners shall be governed by the official admitting policy of the hospital. The admitting policy shall include admission criteria for each level of care/service provided. Such criteria shall be used to determine appropriateness of patient placement. The patient shall be seen by the attending physician within 24 hours following admission to an acute care setting, unless there are extenuating circumstances. 2. Admission Status The Admitting Department will admit patients to the following status: Emergency: Intended for use by patients for the treatment of life-threatening health care problems that require medical intervention within 24 hours or urgent health problems that require medical treatment within 48-72 hours to prevent a life-threatening situation. Inpatient: Intended for use by physicians for patients in need of medical treatment in an acute care setting. Services needed for medical treatment will likely require an overnight stay. Ambulatory Surgery: Intended for use by physicians for patients having a surgical procedure that will be performed in an ambulatory setting. It is planned that the patient will be discharged from the hospital the same day as the procedure. 1 Outpatient: Intended for use by physicians for patients of whom a diagnostic and/or medical treatment is planned. Services will be provided in an outpatient setting, and it is planned that the patient will be discharged from the outpatient setting following the procedure. Observation: Intended for use by physicians for services furnished in the hospital in which the patient receives periodic monitoring by the nursing staff and others to evaluate an outpatient’s condition or to determine the need for a possible inpatient admission. 3. Pre-certification The attending practitioner is responsible for obtaining the required precertification for services planned for the patient as outlined in the patient's third party payor policies. 4. Admission Diagnosis Except in an emergency, no patient shall be admitted for hospital services until a provisional diagnosis or valid reason for admission has been stated. In the case of an emergency, such statement shall be recorded as soon as possible. 5. Admission to ICU Any physician may admit to the Intensive Care Unit; however, all General Practitioners admitting to ICU must have a consult from an Internist for patients who remain on a ventilator for greater than 72 hours and as for management of thrombolytics. If any questions as to the validity of admission to or discharge from the ICU should arise, the decision is to be made through consultation with the chairman of the Critical Care Committee. 6. Admission Documentation Requirements All practitioners shall be governed by the official documentation policy of the Medical Records department when admitting patients to any of the hospital’s services. The attending practitioner is required to document in the patient's clinical record the medical necessity of services requested, unless there are extenuating circumstances. Documentation must also describe the chief complaint, medical status and plan for treatment in order for certification requirements to be met. 2 Following determination of medical necessity for inpatient services utilizing the approved third party payor criteria/guidelines, an expected length of stay will be assigned according to the diagnostic related category. If the patient requires further health care in the hospital, the attending physician will justify the medical necessity in the progress notes on a daily basis and the length of stay shall be adjusted according to third party payor guidelines. Failure to comply with this policy will be brought to the attention of the Physician Advisor. The Physician Advisor will evaluate the need for continued stay or possible continued stay termination, as stated in the hospital's Utilization Management Plan approved by the Executive Committee of the Medical Staff, the CEO and the Board. 7. Emergency Admissions Emergency services will be provided according to the COBRA/EMTALA guidelines as outlined in the Emergency Department policy. 8. Tuberculosis Admissions Patients with active tuberculosis ordinarily are not admitted to the hospital for tuberculosis treatment; they are treated at home. However, there is no regulation that prohibits admitting a patient who has tuberculosis but needs hospital admission for a diagnosis other than tuberculosis. Management of patients with tuberculosis shall be governed by Infection Control policies and procedures. B. Transfers 1. From Emergency services: When seeking medical treatment for conditions of which needed services are not provided by the hospital, patients will be stabilized and transferred to an appropriate facility following COBRA/EMTALA guidelines. Those conditions include, but are not limited to, psychiatric care, alcoholism, drug abuse, and obstetrics. 2. Prioritizing Transfers: All transfers will comply with COBRA/EMTALA guidelines. Subject to those requirements, priority of patient transfers shall be as follows: Emergency patients to appropriate facility/patient bed. Patients from ICU to acute care unit. Patients temporarily placed in a geographical or a clinical service area because of bed overflow to the 3 appropriate area for that patient. No patient will be transferred without such transfer being approved by the responsible practitioner. C. Discharges 1. Discharge Criteria Patients shall be discharged only on a written order of the attending practitioner. Should a patient leave the hospital against the advice of the attending practitioner or without proper discharge, a notation of the incident shall be made in the patient's medical record. 2. Appropriateness for discharge Appropriateness for discharge shall be determined by discharge criteria established for each level of care/service as outlined in the Provision of Care Plan. II. ANESTHESIA SERVICES A. Anesthesia Care Responsibility for the overall management for anesthesia lies with the Director of Anesthesia. Anesthesia types and location are as follows: general, regional, monitored anesthesia care and moderate sedation care are given in the Operating Rooms, Endoscopy Suite, Catherization Lab, ICU, 4 West, Diagnostic Imaging, Neurology Diagnostics, and Emergency Room. The Director of the Anesthesiology Service shall ensure that there is at least one member of the Anesthesiology Service on duty in the Hospital, or on call at all times, to provide routine and emergency anesthesia care. General anesthesia may only be given in the operating room, the Imaging Services departments, and the Endoscopy Suites. B. Anesthesia Rules and Regulations: 1. Anesthesiologists will be available to assist the Service with Staff development in organization of and participation in educational programs. 2. Anesthesiologists will be available on request of the Medical Staff Members to perform consultations relating to the respiratory care of patients of the Medical Staff Members. 3. Certified Registered Nurse Anesthetists shall administer anesthesia under the supervision, direction and guidance of an anesthesiologist and within their scope of service as granted by the Board of Trustees. 4. Anesthesiologists shall actively participate in advising the nurse anesthetists on refresher courses and requiring continuous education and routine inservice programs. 4 5. An anesthesiologist will perform a pre-anesthesia evaluation of the patient. He/she will note on the patient’s anesthesia record all pertinent information relative to the choice of anesthesia in relation to the surgical procedure anticipated, and any previous anesthesia history of the patient. In addition, the risks/benefits of anesthesia will be explained to the patient and noted in the medical record based upon ASA Classifications. 6. A member of the Anesthesiology Staff or other qualified licensed, independent practitioner ordering moderate sedation will re-evaluate the patient immediately prior to the induction of anesthesia, and will document the physiological status of the patient, the readiness, availability, cleanliness, sterility where required, and working conditions of all equipment used in the administration of anesthetic agents. 7. All reusable anesthesia equipment in direct contact with the patient shall be cleaned after each use. 8. Following the procedure for which anesthesia was administered, the anesthesiologist or other qualified person will remain with the patient as long as deemed necessary. Personnel responsible for post anesthetic care will be advised of any specific problems presented by the patient’s condition. A member of the anesthesiology staff or other qualified person, based upon Medical Staff pre-approved PAR score criteria, will authorize the discharge of patients to other services. If sedation during surgery is minimal, the anesthesiologist may discharge the patient from the operating room if PAR scores are met and documentation of such is recorded. 9. The anesthesiologist, anesthetist or other qualified person will record all events taking place in the induction of, maintenance of, and emergence from anesthesia. This record will include the dosage and duration of all anesthetic agents, other drugs, intravenous fluids and blood or blood products. 10. Inpatients that stay overnight will have a second visit by anesthesia/CRNA. An anesthesiologist or CRNA in the PACU will make a post-anesthesia visit to the patient and note in the chart the presence or absence of any anesthesiarelated complications and date and time the entry. A post-operative anesthesia note will be written on outpatients by an appropriate member of the anesthesia service. 11. The type and method of anesthesia for a patient will be decided by the anesthesiologist or qualified LIP while taking into consideration any special requests or problems presented by the surgeon. 12. Complication or unusual events occurring to a patient under anesthesia will be reviewed at the Surgical Care Committee meeting in accordance with criteria or indicators established by that Committee. 5 13. The Director of Anesthesia will participate in the development of and have oversight responsibility for moderate sedation to ensure standardization of care delivered. Competency of Medical Staff for the delivery of conscious sedation will be delineated based upon credentialed privileges as set forth by the Anesthesia Service, Credentials Committee, Medical Executive Committee and approved by the Board of Trustees. 14. Advance Directives and Do Not Resuscitate orders will be discussed with the patient by either Anesthesia or the attending physician prior to surgery to ascertain patient’s wishes as they relate to the continuance of advance directives. 15. Anesthesia is defined as the administration (in any setting, by any route, for any purpose) of general, spinal, or major regional anesthesia or sedation with or without analgesia for which there is a reasonable expectation that, in the manner used, the sedation or analgesia will result in the loss of protective reflexes. III. EMERGENCY SERVICES A. Emergency Services Physician The purpose of the Emergency Services Physician (ESP) shall be to practice quality emergency medicine in accordance with the goals of the Medical Staff and the Hospital. 1. The Emergency Services Physicians shall be members of the Hospital Medical Staff. They shall have all the rights, privileges, and responsibilities of staff membership, except that of admitting patients to the hospital. 2. Emergency Services Physicians shall arrange their schedule to provide emergency patient care twenty-four (24) hours per day, seven (7) days per week. Emergency Services Physicians shall also have a Director who is Board Certified for Emergency Medicine and a specialty deemed appropriate by the Chief of the Department of Medicine. The Director shall be responsible for augmenting the physician staff in situations of increased patient volumes or acuity. 3. Services provided by the Emergency Services Physician shall include, but shall not be limited to the following: a. Providing initial emergency health services 24 hours a day to patients of all ages, ensuring the availability of follow-up care, in or out of the hospital as may be required; 6 b. Evaluating patient’s emergency health needs, stabilizing insofar as possible those patients with life-threatening conditions, and providing such services as are immediately indicated; c. Undertaking the responsibility of establishing the necessary training programs for emergency department and community personnel in order to provide them with the basic skills required to intervene in life-threatening situations; d. Managing the ER team in the care of patients with life-threatening illnesses and injuries, as well as the efficient handling of those patients with more routine problems; e. Ensuring that the layout, equipment and supplies are available to meet both emergency and routine demands; f. Responding to emergency situations arising in the Intensive Care Units or on the floor, provided that theses situations do not interfere with the Emergency Room (ER) activity and coverage; and g. Pronouncing patients’ expirations in the hospital at the request of the attending physician. B. 4. The Emergency Services Physician on duty will be physically present in the Hospital at all times. The professional and ethical conduct of the Emergency Services Physician shall be under the auspices of the Department of Medicine and the Medical Executive Committee. It shall be incumbent upon the Emergency Services Physician to perform in the best interest of the patient first, and secondly, of the Hospital and Medical Staff. 5. Patients are classified as urgent, emergent or non-emergent according to established criteria and conditions, which are approved by the Medical Staff and Emergency Services Physician. The guidelines are used by physicians to establish the priority of care. Emergency Department Rules and Regulations: 1. Clinical privileges shall be delineated for all practitioners rendering emergency care in accordance with Staff and Hospital policies and procedures. 2. The Medical Staff shall adopt a method of providing medical coverage in the Emergency Room. Each clinical department shall establish and maintain their own specific rules and regulations governing their call schedules for each clinical service. Each member of the medical staff shall agree and serve as on call physician for emergency department coverage as required. Physicians 7 who fail to comply with such schedules shall be subject to continued disciplinary action as defined by the Medical Staff Bylaws, up to and including termination of privileges. The call schedules established herein shall be in compliance with all applicable requirements of law, including COBRA/EMTALA, and may be altered by the Executive Committee and/or Board if the call schedules established do not appear to meet any requirements of law. C. 3. Staff physicians shall be entitled to the traditional right of treating their patients in the emergency room based upon the individual privileges. Staff physicians may order treatment in writing or by telephone and in so doing, retain responsibility for their patients. Telephone orders by staff physicians shall comply with the policies and procedures of the emergency room. 4. If requested by an emergency room patient, and if determined appropriate in the judgement of the Emergency Services Physician, the patient’s private physician shall be notified in accordance with the emergency room policies and procedures. The Staff Physician may refer his patient to another member of the Staff, including the Emergency Services Physician, who then shall accept the responsibility for diagnosis and treatment rendered in the emergency room, and refer the patient back to his own physician for followup care. 5. If in the judgment of the emergency services physician a patient needs to be admitted to the Hospital as an inpatient, either for observation or for furthers treatment, the patient shall be admitted in the name of the attending physician. Upon transfer from the Emergency Department to a patient unit, the patient becomes the responsibility of the attending physician. Emergency Room Records: An appropriate emergency room medical record shall be kept for every patient receiving emergency service and shall be incorporated into the patient’s medical record, if such exists. 1. The emergency room medical record shall accompany patients being admitted as an inpatient. 2. The emergency room medical record shall include the following: a. Pertinent history of the injury or illness including details relative to first aid or emergency care given to the patient prior to his arrival at the Hospital; b. History of allergies; c. Description of significant clinical, laboratory, and X-ray findings. In cases where the X-ray interpretation of the radiologist is different from that 8 initially made by the emergency services physician, copies of the radiologist’s report shall be made available and brought to the attention of the emergency services physician. The physician or licensed staff will notify the patient and instructions are documented on the original encounter documentation form; d. Diagnosis including condition of the patient; e. Treatment given and plans for management; f. Condition of the patient on discharge or transfer; g. Final disposition, including instruction given to the patient and/or family for necessary follow-up care; h. Signature by the physician in attendance who is responsible clinical accuracy of the emergency room medical record; and i. Discharge instructions given to patient/family with clear understand j. Along with warnings as to applicable food and drug interactions. D. IV. Patients Screening and Transfers: 1. Every patient presenting to the Emergency Department for treatment or screening shall be screen in accordance with the requirements of good medical procedure and COBRA/EMTALA. Patient shall be triaged based upon condition; the triage shall not be in lieu of, but may be in conjunction with, an appropriate medical screening. 2. Medical screenings in the Emergency Department may be delegated by the Medical Staff to include the following categories of LIP:, Physician or Physician Extenders, i.e., Physician Assistant and/or Advanced Practice Registered Nurse (APN/FNP) 3. Patients with conditions whose definitive care is beyond the capabilities of this hospital shall be referred to the appropriate facility, when in the judgement of the attending physician or emergency services physician, the patient’s condition permits such a transfer. The Emergency Department shall comply with COBRA/EMTALA guidelines in the transfer of all patients. GENERAL CONDUCT OF CARE The medical staff shall be responsible for the medical care and treatment of each patient in the hospital, for the prompt completion and accuracy of the medical records, for necessary special instructions, and for transmitting reports of the condition of the patient to the referring practitioner and to relatives of the patient. 9 A. Physician Coverage 1. Each member of the medical staff shall name one, and preferably two, members of the medical staff as his alternate(s), who may be called to attend his patients in an emergency or in his absence. The physician whom the attending physician names to be responsible for the care of his patients in his absence must be a member of the medical staff and have comparable clinical privileges to manage the patients for whom he has agreed to accept coverage. In case of failure to name such alternate, the President of the Medical Staff and/or the CEO shall have the authority to call on any member of the staff as an alternate should this be considered necessary. a. Whenever these responsibilities are transferred to another staff member, a note covering the transfer of responsibility shall be entered on the order sheet of the medical record. b. A practitioner who will be unavailable for over 24 hours shall, on the order sheet of the chart of his patients, indicate in writing the name of the practitioner who will be assuming responsibility for care of the patients during his absence and he shall communicate this to the covering practitioner. The physician whom the attending physician names to be responsible for the care of his patients in his absence shall be responsible for total coverage of the patients, including discharge. It is the attending physician's responsibility to do the discharge summary. B. Consent For Treatment A treatment consent form, signed by or on behalf of every patient admitted to the hospital, must be obtained at the time of admission. The admitting officer should notify the attending practitioner whenever such consent has not been obtained. When so notified, it shall, except in emergency situations, be the practitioner’s obligation to obtain proper consent before the patient is treated in this hospital. C. Informed Consent 1. In addition to obtaining the patient’s general consent for treatment, informed consent shall be obtained by the surgeon, physician or practitioner responsible for the specific treatment(s). 2. The medical record shall contain evidence of the patient’s informed consent for procedures or treatment for which it is appropriate, as determined by the medical staff and described in the hospital’s informed consent policy. 3. The patient or responsible person should be informed of all procedures to be performed, including the probability of success, risks, alternatives, and benefits. 10 D. 4. Consent forms should include the identity of the patient, the date, the procedure or treatment to be rendered (in layman terminology when possible), the name(s) of the individual(s) who will perform the procedure or administer the treatment, and authorization for disposition of any tissue or body parts as indicated. 5. The hospital informed consent policy and procedure shall be consistent with legal requirement, and shall govern the procedure followed by physicians and other staff members in obtaining and documenting informed consent. 6. The policy shall also include special aspects of obtaining consent such as: emergency treatment, unaccompanied minors, photographs, observation of a surgical procedure or for other education purposes. 7. Informed consent may be withdrawn by the patient, or in cases whereas the patient is incapable of consent or withdrawal, by the designed authority to act on behalf of the patient. Consent may be withdrawn by verbal or written request at any time prior to the procedure. Orders for Treatment All orders for treatment shall be in writing, signed, dated, and timed by the responsible practitioner or dictated and subsequently signed, dated and timed by the practitioner. E. Consultations: 1. Consultation shall be completed within 24 hours of request unless emergent or otherwise indicated by the ordering physician, or defined by Medical Staff Policy. 2. Except in an emergency, consultation is required in the following situations: a. when requested by the patient or responsible decision-maker; b. when the patient is critically ill; unless the physician has privileges for care of critical illness; c. curettages or other procedures by which a known or suspected pregnancy may interrupt; and d. when diagnosis is obscure after ordinary diagnostic procedures have been completed e. when there is doubt about the therapeutic measures to be used; 11 f. high risk patients undergoing major operative procedures; g. in situations where the specific skills of other physicians may be needed h. at any other time specified in the rules of the applicable department 3. Consultation reports shall contain: a. review of the patient’s record by the consultant; b. pertinent findings by physical exam; and c. consultant’s opinion and recommendations. F. Care of the Suicidal Patient For the protection of patients and the medical and nursing staffs of the hospital, certain principles are to be met in the care of the potentially suicidal patient. G. 1. Any patient known or reasonably suspected to be suicidal shall be referred to another institution where suitable facilities are available. 2. The patient must be attended at all times by an adult individual approved by a nursing supervisor until transfer. 3. A request for psychiatric consultation and treatment is required for all patients who have attempted suicide or have taken a chemical overdose. It must be documented in the patient's medical record that such services were at least offered. Emergency Treatment 1. In the case of an emergency, any physician or dentist member of the medical staff shall be permitted to do everything possible to save the patient's life, or to save the patient from serious harm, to the degree permitted by his license and regardless of department or staff status or clinical privileges. In so acting, the practitioner is obligated to summon all available consultative aid deemed necessary. 2. An "emergency" is defined as any condition in which serious permanent harm or exacerbation of injury or disease could result to a patient or in which the life of a patient is in immediate danger and any delay in administering treatment could add to that danger. 3. In cardiac arrest, a code Blue shall be called through the public address system and shall be carried out according to the procedures developed and approved by the Critical Care Committee. 12 H. Deaths: 1. In the event of a hospital death, the deceased shall be pronounced dead by the attending practitioner, house physician or delegated nursing staff pursuant to hospital policy within a reasonable time. The time of death shall be noted in the medical record. 2. If CPR is attempted, a brief statement regarding procedures, medication, etc. shall be recorded on the progress sheet. In unexpected death, the electrocardiogram monitor strip may be employed to further substantiate death. 3. The attending physician should be notified of all cases regarding death of patients to which he was attending. 4. Release of bodies shall conform to applicable law, which states that in cases of death from violence, apparent suicide, or any suspicious, unusual or unexplained manner, the county medical examiner must be notified before the body is released. 5. It shall be the duty of all staff members to secure autopsies where appropriate. An autopsy may be performed only after proper consent has been obtained. All autopsies shall be performed by a hospital pathologist or a physician delegated this responsibility. Provisional anatomic diagnoses shall be recorded on the medical record within three days and the complete report and final diagnoses made part of the record within 60 days. 6. An autopsy should be considered under the following circumstances: a. death under age 50; b. death within 48 hours of a surgical/invasive procedure, including radiological procedure; c. death associated with drug reaction; d. deaths within 48 hours of admission; e. emergency room deaths; f. outpatient deaths; g. deaths in which the admission diagnosis suggests death was not expected; 13 h. deaths in which it is believed that an autopsy would diagnose a known or suspected illness that may have a bearing on survivors or recipients of transplant organs; and i. I. deaths known or suspected to have resulted from environmental or occupational hazards. Physician Orders 1. Orders: Verbal Orders/Telephone Orders a. All orders for treatment shall be in writing, dated, timed and signed by the responsible practitioner or dictated to a delegated staff member, authenticated by signature, dated and timed by the responsible practitioner. Verbal and telephone orders should be used infrequently and only when necessary to ensure the continuity of patient care in a timely manner. A verbal/telephone order shall be considered to be in writing if dictated within the following limitations: Registered Nurse or Licensed Practical Nurse - all orders Registered Dietitian - Diet or Nutritional orders only Registered Medical Technologist - Laboratory orders only Registered Pharmacist - Medication orders only Registered Physical Therapist - Physical Therapy orders only Registered Radiology Technologist - Diagnostic Imaging orders only Registered Respiratory Therapists - Respiratory Therapy orders only Registered social Worker - Social Service orders only b. All orders, including those dictated over the telephone shall be signed, dated, and timed by the appropriately authorized person to whom dictated information was given, along with the name of the practitioner per his/her own name. The responsible practitioner shall authenticate such orders at the next hospital visit in which a patient visit occurs and an entry written in the medical record, not to exceed 48 hours. Restraint orders are considered potentially hazardous and shall be signed within 24 hours of initiation, reviewed and renewed each calendar day thereafter as needed or indicated. 2. Legibility of Orders. The practitioner’s orders must be written clearly, legibly and completely. Orders that are illegible or improperly written will not be carried out until rewritten or clarified according to hospital policy and procedure. The use of “renew” and “continue” orders is not acceptable. 14 3. Renewal of orders post-op. All previous orders are canceled when patients go to surgery. The attending physician must be consulted before administering any orders carried out prior to surgery and maintenance therapy if those orders have not been re-ordered in the post-operative period. 4. Medication Orders: a. All drugs and medications administered to patients through a written order shall be those listed in the latest edition of a) United States Pharmacopoeia, b) National Formulary, c) American Hospital Formulary Service, d) AMA Drug Evaluations, or e) any other drugs considered and approved by the Pharmacy and Therapeutics Company of the Hospital. b. self-medication by patients shall not be permitted unless written in the orders by the attending physician. 5. Restraint Orders Patients with restraint orders must be seen by physician each calendar day and a new order issued if continuation of the restraint is clinically indicated. 6. Standing Orders Standing orders shall be instituted only after approval of the appropriate committee. Standing orders shall be reviewed by the responsible medical staff committee in accordance with hospital policy and procedure, or at a minimum of every two years. As with any order for treatment, all standing orders must be signed and dated and timed by the responsible practitioner when utilized. Printed orders of individual physicians shall be reviewed every two years by the physician to ensure continued appropriateness. 7. Orders From Non-Medical Staff Members The ordering of any test or procedure by a Licensed Independent Practitioner who is not a medical staff member shall not constitute the exercise of clinical privileges, since the practitioner would not be personally rendering patient care within the hospital. Nevertheless no practitioner shall be entitled to order tests or procedures unless the order has been verified. The department receiving the order will be responsible for contacting the ordering practitioner to verify that the order or prescription is valid and that the order came from the ordering practitioner. If a practitioner, who is not a member of the medical staff, orders a test or procedure which requires the ordering practitioner to render patient care, the order will not be honored. A practitioner must be a member of the medical staff to provide patient care. 15 V. MEDICAL RECORDS The attending physician shall be responsible for the preparation of a complete and legible medical record for each patient. All significant clinical information pertaining to a patient shall be incorporated in the patient medical record. Required contents of the medical record are governed by the Coding Documentation policy of the Medical Records Department. All medical records entries are to be dated and timed. A. Practitioner Responsibility for Completion of Medical Records A complete medical record includes, but is not limited to, the following items: 1. 2. 3. 4. 5. 6. 7. 8. B. Identification data Medical history and physical examination Diagnostic/therapeutic orders Evidence of informed consent Clinical observations and results of treatment Reports and results of tests and procedures Conclusions at end of hospitalization Final diagnosis/procedures Identification Data This data should include the patient's name, address, date of birth and next of kin. There should also be a number that identifies the patient and the patient's medical record(s) pursuant to hospital policy and procedure. C. History and Physical 1. A medical history and an appropriate physical examination must be completed within 24 hours of admission or registration for patients admitted to inpatient or observation status, but prior to surgery or procedure requiring anesthesia services. Patient admitted to the Skilled Nursing Unit shall have a medical history and appropriate physical examination completed within 48 hours of admission to the unit in accordance with unit guidelines. 2. Other non-inpatient services may require that a medical history and physical examination be performed. The extent of medical history and physical examination for those services are governed by the medical staff guidelines for operative/invasive procedures. 3. The medical history and physical examination should include the chief complaint, details of the present illness, relevant past social and family and medical histories appropriate to the patient’s age, inventory of body systems, relevant physical examination, current medications including 16 other counter drugs, homeopathic and vitamin, mineral supplements; conclusions or impressions drawn from the medical history and physical exam, diagnosis or diagnostic impression, types of treatment and treatment plan, in accordance with the applicable hospital policy and procedures. D. 4. Whenever possible, the medical history should be obtained from the patient. Opinions of the interviewer should not be recorded in the body of the history. 5. If a complete medical history and physical examination has been completed by a practitioner granted authority to perform H&P by state licensure within 30 days prior to the admission, such as in the physician staff member's office, a durable legible copy of this report may be used in the patient's hospital medical record; provided the record is updated pursuant to hospital policy at the time of admission and/or prior to any operative/invasive procedure. 6. History and physical examinations for inpatients must be performed by a qualified physician or delegated by the attending to the designated LIP; Physician Extenders, i.e., Physician Assistant and/or Advanced Practice Registered Nurse. The attending physician retains responsibility for the content of the History and Physical examination and must so indicate by countersigning the History and Physical. The History and Physical must be authenticated by the attending physician within the hospital policy and procedure for authentification of records. 7. The Medical staff will monitor the quality of the History and Physical through the established Performance Improvement Plan and peer review. Clinical Observations The Medical staff should give a pertinent chronological report of the patient's course in hospital and should reflect any change in condition and the results of treatment. Pertinent progress notes should also be made by others so authorized by the medical staff, such as house staff members, individuals who have been granted clinical privileges, and specified professional personnel. A progress note must be entered daily by the attending physician or by the physician covering in his absence. 1. Each consultation report should contain a written opinion by the consultant that reflects, where appropriate, an actual examination of the patient and the patient's medical record(s). 2. Nursing notes and entries by specified professional personnel should contain pertinent, meaningful observations and information such as vital signs and, where appropriate, the status of infusions, surgical dressings, tubes, catheters and drains, treatment modalities or consultation recommendation. Authorization for medical records documentation is specifically limited to 17 Nursing staff, Physical Therapist, Radiology Technicians, Dieticians, Social Services, Laboratory Services, and Risk Management, as relates to the scope of their assigned authority. E. Consultation Report Each report should contain a written opinion of the consultant that reflects, where appropriate, an actual examination of the patient and patient’s medical record(s). F. Nursing Notes and Entries Specified Professional Personnel Entry should contain pertinent, meaningful observations and information such as vital signs and, where appropriate, the status of infusions, surgical dressings, tubes, catheters and drains. G. Reports/Results of Diagnostic Tests All diagnostic and therapeutic tests/procedures should be recorded and authenticated in the medical record. This may also include any reports from facilities outside the hospital, in which case the source facility shall be identified on the report. Reports of pathology and clinical laboratory examinations, radiology and nuclear medicine examinations or treatment, anesthesia records, and any other diagnostic or therapeutic procedures should be completed promptly and filed in the record within 24 hours of completion if possible. H. Pre-Operative Diagnosis The responsible practitioner should record and authenticate a pre-operative diagnosis prior to surgery. I. Operative Report An operative report must be dictated and a progress note written immediately after surgery. The operative report should contain a description of the findings, the technical procedures used, the specimens removed, the post-operative diagnosis and the name of the primary surgeon and any assistants. The complete operative report should be authenticated by the surgeon and filed in the medical record as soon as possible after surgery. J. Conclusions at Termination of Hospitalization 1. The following items should be included in the Discharge Summary of inpatients: a. Significant findings b. Procedures performed c. Treatment rendered d. Condition on discharge 18 e. Specific instructions given to the patient and/or family on discharge including physical activity, medications, diet and follow-up care. f. Final diagnosis K. 2. A final progress note may be used for outpatient and observation stays of under 48 hours. A final progress note may be substituted for the clinical resume in the case of observation patients. The final progress note shall include the patient’s condition at discharge, discharge instructions given to the patient and family, and the follow up care. 3. When pre-printed instructions are given to the patient or family, the record should so indicate and a sample of the instruction sheet in use at the time should be on file in the medical record department. If authorized in writing by the patient or a legally qualified representative, a copy of the clinical resume should be sent to any known medical practitioner and/or medical facility responsible for the subsequent medical care of the patient. 4. In the event of death, a summation statement shall be added to the record as part of the dictated Discharge Summary pursuant to hospital policy. The death summary should include: the reason for admission, the findings, hospital course, and events leading to death. Autopsy Report Autopsy will be performed in accordance with hospital policy and procedure as approved by the Medical Staff, and under the WV State guidelines of the Office of the Medical Examiner. When an autopsy is performed, provisional anatomic diagnoses should be recorded in the medical record within three days and the complete report should be made a part of the record within 60 days. L. Consent for Release of Medical Information 1. Obtaining Consent Written consent of the patient or his legally qualified representative is required for release of medical information to persons not otherwise authorized to receive this information. This shall not be construed to require written consent for use of the medical record for automated data processing of designated information, for use in patient care evaluation studies, such as retrospective audit and medical staff monitoring functions, for departmental review of work performance, for official surveys for hospital compliance or for educational purposes. Medical records may be removed from Hospital's jurisdiction and safekeeping only in accordance with a court order, subpoena or statute. 2. Confidential Records 19 When certain portions of the medical record are so confidential that extraordinary means are considered necessary to preserve privacy such as in the treatment of some psychiatric disorders, these portions may be stored separately, provided the complete record is readily available when required for current medical care follow-up, for review functions or for use in patient care evaluations or for use in patient care evaluation studies. The medical record should indicate that a portion has been filed elsewhere in order to alert authorized reviewing personnel of its existence. M. Quality of the Medical Record The quality of the medical record depends in part on the timeliness, meaningfulness, authentication and legibility of the informational content. 1. Authentication a. Entries in medical records may be made only by medical staff members or individuals given specific clinical privileges. b. All entries in the record must be dated, timed and authenticated and include an established method to identify the authors of entries. Such identification may include written signatures, initials, or electronic signature. c. When electronic signatures are authorized, the individual whose signature is represented shall place in the administrative offices of the hospital a signed statement to the effect that he is the only one who has access to electronic signature and is the only one who will use it. There shall be no delegation of the use of electronic signature to another individual. d. The parts of the medical record that are the responsibility of the medical practitioner’s shall be authenticated by him. For example, when specified professional personnel have been approved for such duties as medical history taking and for documenting some aspects of the physical examination, such information shall be appropriately authenticated by the responsible practitioner. The responsible medical staff member's own pertinent observations and significant physical findings should be added wherever necessary or he may record his own history and physical examination of the patient. e. When members of the house staff and other specified professional personnel are involved in patient care, sufficient evidence should be documented in the medical record to substantiate the active participation in, and supervision of, the patient's care by the responsible attending practitioner as dictated by hospital policy and procedure. 2. Symbols/Abbreviations 20 a. To avoid misinterpretation and/or potential medical errors, only authorized symbols and abbreviations may be used in the medical record. Only those abbreviations and symbols approved by the medical staff in coordination with national patient safety initiatives may be used. Utilization of abbreviations and/or symbols deemed as inappropriate or dangerous per hospital policy may not be utilized. Repetitive use of unacceptable abbreviations and/or symbols can constitute grounds for peer review. b. No change can be made in the history and physical or progress notes. However, if the attending physician does not agree with what is written, he may place an addendum. Notation errors made in the record must be noted as error, with the practitioner’s initials according to hospital policy. 3. Legibility In the interest of accuracy, legibility and reproducibility, and where budgetary and personnel availability permit, it is recommended that medical record entries, where appropriate, be typed. Special consideration should be given to the typing of radiology and pathology reports, operative reports and clinical resumes. When transcription and filing of these medical record reports cannot be accomplished in a timely manner, written entries pertinent to the continuity of patient care shall be recorded. Legibility of the medical record is monitored through the Performance Improvement Plan for the facility. 4. Timely completion of medical records The medical record should be complete at the time of discharge, including progress notes, final diagnosis and (dictated) clinical resume. Where this is not possible because final laboratory or other essential reports have not been received at the time of discharge, the patient's chart will be available in a stated place in the medical record department. a. Upon discharge of a patient the medical staff is required to complete the medical record within 30 days. b. A completed medical record includes dictation, transcription, and signatures. c. Physicians may have admitting and consultative privileges temporarily suspended from inpatient and outpatient settings (including operative/invasive procedures) following a one week notice that a record is determined to be delinquent. Physicians who do not complete the delinquent records within 30 days of the suspension notice are subject to disciplinary action as defined in the Medical Staff Policy on Medical Records Delinquency. 21 d. Any physician placed on medical records suspension three or more times for incomplete medical records within any reappointment cycle, is subject to disciplinary action, including suspension of 31 days or more, as defined by the Medical Staff Policy on Medical Records Delinquency. e. When a physician's privileges have been suspended, he must arrange for his emergency admissions to be admitted under another physician's care or admit his patient to another hospital. f. In case of re-admission of a patient, all previous records shall be available for the attending physician. This shall apply whether the patient is attended by the same physician or by another. g. Reappointment decisions shall be based in part by a physician's performance in timely completion of medical records. The Credentials Committee shall take into consideration the practitioner’s compliance with medical records policy and procedures and delinquency rates and make recommendations for limitation, restriction and/or denial of reappointment when warranted or as defined by hospital policy and procedure. h. No medical staff member should be permitted to complete a medical record on a patient unfamiliar to him in order to retire a record that was the responsibility of another staff member who is deceased or unavailable permanently or protractedly for other reasons. The committee delegated the responsibility for medical record review will have the responsibility to retire medical records upon the authority of the Executive Committee. VI. GENERAL RULES REGARDING SURGICAL CARE A. Pre-Operative Requirements 1. Surgery is performed only after a history and physical examination have been completed pursuant to hospital policy and procedure, indicated diagnostic tests have been completed, preoperative diagnosis have been completed, informed consent has been obtained explaining risks and benefits of the planned procedure and for the administration of blood/blood components, and all have been recorded in the patient's medical record. 2. In emergency situations where there is inadequate time to record the history and physical examination before surgery, a brief note including the condition of the patient at the time of surgery, cardiovascular findings, vital signs, and reason for surgery must be recorded before surgery. 22 B. 3. Pre-operative laboratory work may be determined by the surgeon. In addition the anesthesiologist will determine the appropriate lab/diagnostic work-up needed as part of the anesthesia pre-operative evaluation using the American Anesthesia Standards. 4. Whether or not a patient is pregnant should be determined prior to a surgical procedure as part of the preoperative evaluation performed by the anesthesiologist. A pregnancy test should be ordered to make this determination. 5. If the aforementioned items are not recorded, the operation shall be canceled by the operating room supervisor, attending surgeon and/or the anesthesiologist, unless the attending surgeon states, in writing, that such a delay would constitute a hazard to the patient, or the anesthesiologist, in consultation with the surgeon, states that the surgery may proceed. Dental Procedures: A patient admitted for dental care is the dual responsibility of the dentist and a physician member of the medical staff. Surgical procedures performed by dentists shall be under the overall supervision of the chief of surgery. 1. Dentists’ responsibilities are to provide in an outpatient setting the following: a. A detailed description of the exam of the oral cavity and a pre-operative diagnosis; including any relative History and Physical information as may be required under the operative/invasive guidelines. This H&P may be delegated under the facility’s applicable policy but must be countersigned by the Dentist. The dentist retains accountability for the H&P as performed under the policy guidelines. b. A complete operative report describing the findings and technique and in case of extraction of teeth, the dentist shall clearly state the number of teeth and fragments removed, and all tissue including teeth and fragments shall be sent to the hospital pathologist for exam. c. Progress notes as are pertinent to the oral condition; and Clinical resume or summary statement including the patient’s condition at discharge, discharge instructions to the patient and family, and the follow up care required. d. To establish an attending physician to co-manage the patient’s care whenever dictated by medical necessity, patient condition or whenever inpatient admission is planned or required. 23 2. Physicians’ responsibilities for patients requiring inpatient admission are: a. Medical history pertinent to the patient's general health; b. A physical exam to determine the patient's condition prior to anesthesia and surgery; and c. Supervision of the patient's general health status while hospitalized 3. The discharge of the patient shall be on written order of the dentist member of the medical staff and the medical staff physician. Podiatry Procedures: A patient admitted for podiatry care is the shared responsibility of the podiatrist and a physician member of the medical staff. Surgical procedures performed by podiatrists shall be under the overall supervision of the chief of surgery. 1. Podiatrist’s responsibilities are to provide in an outpatient setting the following: a. A detailed description of the exam of the involved extremity and a preoperative diagnosis; including any relative History and Physical information as may be required under the operative/invasive guidelines. This H&P may be delegated under the facility’s applicable policy but must be countersigned by the Podiatrist. The podiatrist retains accountability for the H&P as performed under the policy guidelines. b. A complete operative report describing the findings and technique; and c. Progress notes that are pertinent to the condition of the involved extremity, clinical resume or summary statement including the patient’s condition at the time of discharge, discharge instructions given to the patient and family, and follow-up care required. d. To establish an attending physician to co-manage the patient’s care whenever dictated by medical necessity, patient condition or whenever inpatient admission is planned or required. 2. Physicians’ responsibilities for patients requiring inpatient admission are to provide: a. Medical history pertinent to the patient’s general health; b. A physical examination to determine the patient’s condition prior to anesthesia and surgery; and c. Supervision of the patient’s general health status while hospitalized. 24 3. D. The discharge of the patient shall be on written order by the podiatrist and physician member of the medical staff. Informed Consent for Surgical Procedures 1. Written, signed, informed surgical consent shall be obtained prior to any operative procedure, except in those situations wherein the patient's life is in jeopardy and suitable signatures cannot be obtained due to the condition of the patient. The responsibility for obtaining informed consent is that of the treating surgeon, physician or other practitioner and documentation of the completion of this process must be provided in accordance with hospital policy and procedure. 2. In emergencies involving a minor or unconscious patient in which consent for surgery cannot be immediately obtained from parents, guardian or next of kin, these circumstances should be fully explained on the patient's medical record. a. A consultation in such instances may be desirable before the emergency operative procedure is undertaken if time permits. b. Hospital administration should also be notified of the situation. 3. Should a second operation be required during the patient's stay in the hospital, a second consent specifically related to that procedure should be obtained according to hospital policy and procedure. 4. If two or more specific procedures are to be carried out at the same time and this is known in advance, they should all be described and consented to on the same form. 5. If, post-operatively, a patient develops a complication from an operation and requires immediate attention or surgical intervention, a new consent is not required if the patient has not yet left the Recovery Room, unless there is actual knowledge that the contemplated procedure is outside the scope of the original consent. E. Surgical Assistants 1. In any surgical procedure with unusual hazard to life there must be a qualified assistant present and scrubbed. 2. An assistant may be a physician or a specially trained registered nurse, or licensed practical nurse, or a physician's assistant who is employed by the hospital or has been granted the appropriate clinical privileges. 25 F. Surgical Specimens 1. All tissues, foreign bodies, implants and other specimens removed at the operation, as defined by policy and procedure, shall be sent to the hospital pathologist, who shall make such exam, as he may consider necessary to arrive at a diagnosis. 2. This authenticated report shall be made a part of the patient's record. G. Operating Room Start Time Surgeons must be in the operating room and ready to begin an operation at the time scheduled. In no case will the operating room be held longer than 15 minutes after the time scheduled for a surgery. H. Scheduling Surgical Procedures 1. Prioritizing a. Emergency surgery is assigned first priority and elective surgery is assigned second priority. b. When an elective case is preempted by an emergency, the elective case is re-scheduled as soon as possible. The nursing unit is notified about the emergency by surgery personnel, and the re-scheduled surgeon is notified by the surgery supervisor or anesthesiologist. c. Priority time is on a first come, first serve basis for advance elective surgery. d. Limited records concerning case scheduling are maintained in order for a surgeon to understand how his starting time was determined. 2. Emergency Coverage Emergency Coverage of the operating room shall be maintained at all times. 3. Scheduling Conflicts Scheduling conflicts between surgeons regarding scheduling of emergency cases should be resolved by the surgeons or referred to the chairman of the surgery and anesthesiology department, as defined by departmental policy. 4. Reserving an Operating Room The following information is required to make a surgical reservation: 26 a. Patient's first and last name; b. Age of patient; c. Room number if patient is in hospital; d. Diagnosis; e. Operative procedure to be done. If exploratory laparotomy, the physician must state what he expects to do, e.g. exploratory laparotomy and possible colon resection; f. Name of assistant or a request that one be provided; g. Type of anesthesia to be given; h. Request any special equipment or procedure, e.g. technician, frozen section; and time required. 5. Use of the Operating Rooms Beyond Scheduled Time To facilitate use of the operating rooms and/or complete operations started, adjustments in schedule time may be necessary for cases posted at a requested hour when cases in process extend beyond the operating room time scheduled. The affected surgeon will be notified of these changes prior to time of scheduled case. I. Safety 1. Identification of Patient Verification of the patient identity will be completed according to hospital process using two patient identifiers and being completed at each change in venue as defined by hospital policy and procedure. 2. Pre-operative Evaluation and Documentation The medical record is checked for a written surgical order, pre- operative diagnosis, recorded history and physical exam, required laboratory procedures, informed consent forms, and pre-operative checklist. 27 3. Policy and Procedures Policy and procedures shall be developed to outline specific pre-operative requirements for all operative and invasive procedures according to the type of anesthesia used. a. The policy shall be applicable to any procedure performed in either an inpatient or outpatient setting. b. The policy shall include the level of assessment required before, during and after the procedure. c. The policy shall include monitoring requirements. 4. Care and Transport of Patients Patients will be transported to the surgical suite by a nurse, technician or nursing assistant, and O.R. attendant; and from the recovery room by a recovery room nurse and O.R. attendant a. Patients will be transported from the OR Holding Area to the surgical suite by a circulating nurse from the waiting area. b. Patients will be transported from the surgical suite to level one recovery by a nurse anesthetist or anesthesiologist together with the circulating nurse or attendant. 5. Septic Cases a. All surgical procedures done on patients in isolation will be considered septic cases, i.e. purulent drainage, possible or known tuberculosis, or active infection of any type. b. These cases are brought directly to the operating room and taken directly back to the patient's room at the end of surgery when the patient is "awake". c. If procedure is done under general anesthesia, the patient is taken to the isolation room in PACU. After patient is "awake," he is taken back to his room. d. Terminal cleaning will be done in the operating room at the completion of the case and all personnel in the room during the procedure will change their complete attire before entering another room. e. All equipment will be terminally disinfected and sterilized if possible. 28 f. All anesthetic equipment will be gas sterilized before reuse. VII. General Rules and Regulations: A. Visitors B. 1. If the visitor is from a recognized training program, the surgeon need only obtain verbal permission from the patient or guardian and document the same in the chart. Medical Executive Committee and Medical Staff Office should be notified in advance of any visitor planed for a procedural area. 2. If the visitor is not from a recognized training program, the surgeon must obtain prior authorization from the Medical Executive Committee and have the patient sign an authorization form; likewise the surgeon must sign a second form authorizing the visitor. 3. The O.R. supervisor should be informed in advance when a visitor will be in the operating room. With approval of the O.R. supervisor, and in accordance with the rules and regulations and the bylaws, only people with bona fide medical reasons or technical personnel, as required, will be allowed in the operating room. Photography A photo release form is to be signed by the patient, which releases the hospital, its agents, employees and physicians from any responsibility or liability, and/or breech in confidentiality which could result in connection with the use of any photos taken. C. Confidentiality and Security of Information Technology Services: All medical staff members are required to abide by the policies and procedures of the facility for appropriate access of the information systems. This includes all patient personal information maintained under HIPAA guidelines and facility policies. Medical Staff violations of the appropriate access policies and procedures will be addressed through the Executive Committee according to policy and may include disciplinary action including the loss of medical staff membership and privileges. VIII. DISASTER PLAN There shall be a plan for the care of mass casualties resulting from any major disaster based upon hospital's capabilities in conjunction with other emergency facilities in the community. It shall be developed by a committee, which includes a member of the medical staff, the chief nursing officer or designee, and a representative from Hospital administration. When approved by the Medical Staff and Board, the plan shall be made available to the medical staff. The disaster plan should make provisions within Hospital for: 29 Availability of adequate basic utilities and supplies, including gas, water, food and Essential medical and supportive materials; An efficient system of notifying and assigning personnel; Unified medical command under the direction of a designated physician (the chairman of the committee or designated substitute); Conversion of all usable space into clearly defined areas for efficient triage, patient observation, and immediate patient care; Prompt transfer, when necessary, and after preliminary medical or surgical services have been rendered, to the facility most appropriate for administering definitive care; A special disaster medical record such as an appropriately designated tag that Accompanies the casualty as he is moved; Procedures for the prompt discharge or transfer of patients in the hospital who can be Move without jeopardy; Maintaining security in order to keep relatives and curious persons out of the triage area; Pre-establishment of a public information center and assignment of public relations Liaison duties to a qualified individual; and Advance arrangements with communications media to provide organized dissemination of information. Efficient system of credentialing, assigning, and supervising those practitioners that maybe needed to assist with patient care need when so determined by Medical Staff President, Chief Executive Officer and/or their designees in accordance with hospital policy. All physicians shall be assigned to posts in the hospital and it is their responsibility to report to their assigned stations. The President of the Medical Staff and Chief Executive Officer will work as a team to coordinate activities and directions. In case of evacuation of patients from one section of the hospital to another or evacuation from the hospital premises, the President of the Medical Staff and/or his designee will authorize the movement of patients. All policies concerning direct patient care will be the joint responsibility of the President of the Medical Staff and Chief Executive Officer of the hospital. In either's absence, the delegated alternate will assume responsibility. The disaster plan should be rehearsed at least twice a year, preferably as part of a coordinated drill in which other community emergency service agencies participate. The drills, which should be realistic, must involve the medical staff as well as 30 administrative, nursing and other hospital personnel. Actual evacuation of patients during drills is optional. A written report regarding the evacuation rehearsal and implementation of all drills shall be made. IX. CRITICAL CARE UNITS The Critical Care Committee shall propose specific regulations concerning the Critical Care Units of the hospital. These regulations shall be subject to the approval of the Executive Committee in the same manner as department rules and regulations. X. DEPARTMENTS Each department will establish its own regulations and procedural rules. These will vary with the complexity of the department and the degree to which each department finds it necessary to duplicate the overall organizational pattern of the medical staff itself. XI. CONTINUING EDUCATION Every member of the staff is expected to attend a reasonable amount of the hospital's continuing educational programs. Each is also required to document, as part of the re-credentialing process, any continuing educational courses attended outside the hospital. XII. PATIENT SAFETY: All members appointed to the Medical Staff will participate and encourage processes under which patient safety and quality of care are improved, including but not limited to those processes, policies and procedures, committees and functions outlined within these bylaws. XIII. PHYSICIANS HEALTH: The Organization has an obligation to protect patients from harm. In this regard, the medical staff and organization leaders have designed a process that provides education about physician health issues addresses prevention of physical, psychiatric or emotional illness and facilitates confidential diagnosis, treatment and rehabilitation of physicians who suffer from a potential impairment as defined by the Medical Staff policies and procedures. (Medical Staff Policy/ Impaired Physicians – Medical Staff Policy/Disruptive Physicians) XIV. MASTER COPY OF MEDICAL STAFF BYLAWS, RULES AND REGULATIONS A master copy of the medical staff bylaws, rules and regulations shall be kept with the staff minutes. The staff secretary shall record changes and keep the master copy up-to-date. 31 ADOPTED by the active medical staff on January 15, 1980. APPROVED by the Board on January 23, 1980. 32