Chapter 14 Disease of Nerve System
advertisement

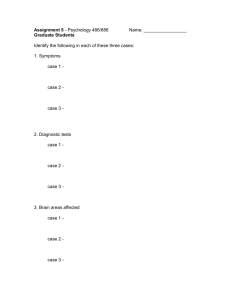
Chapter 14 Diseases of Nervous System OBSERVATIONAL METHODS OF SPECIMEN Observation gists of gross specimen: to observe whether vessels of cerebral pia mater congest; whether there is hemorrhage, effusion or exudation in subarachnoid space; whether cerebral hemispheres are symmetrical; whether gyrus widen or narrow; whether sul cus flatten or deepen; whether medium arteries at base of skull suffered atherosclerosis; whether there is notch at cerebellum and hippocampal sulcus and gyrus. At first, we should identify the cut surface were coronary, horizontal or sagittal section; then observe whether there is hemarrhage focus in brain; whether lateral ventricle dilate; whether ventrical wall is smooth; whether soften, local or nodular focuse; at last, observe the size, shape, color, texture and boundary to around cerebral tissue further. Observation gists of tissue sections: In gross, to observe whether weak or deep staining area exist. Microscopically, to observe whether there are pathological changes in subarachnoid space, vessels of cerebral pia mater, nerve cell or perivascular space. We should observe the features of focus carefully and identify the property of lesion, if local locus exists. AIMS 1.To grasp the pathological features of epidemic meningitis and type B epidemic encephalitis, and the differences between them. 2.To understand the classification and morphological character of common tumor in central nerve system. CONTENTS Infective disease Tumor of nerve system Gross specimen Tissue section Suppurative meningitis Suppurative meningitis Epidemic encephalitis B Epidemic encephalitis B Astrocytoma Astrocytoma Ependymoma Ependymoma Meningioma Meningioma Neurilemmoma Neurilemmoma KEY POINTS OF SPECIMEN OBSERVATION 1. Infective disease (ⅰ) Suppurative meningitis Basic pathologic changes (1) Gross morphology The brain is swollen and vessels of cerebral pia mater are congested. Subarachnoid space is filled with yellow purulent exudates, which covered the surface of gyrus and sulci. In mild case, the exudates distribute along the blood vessels. Cerebral ventricular enlargement can be induced by disturbance of cerebrospinal fluid circulation. (2) Histopathology Vessels of cerebral pia mater are dilated and congested apparently. Severe case can suffered vasculitis and thrombosis. The subarachnoid space is filled with a large number of neutrophils,fibrin, a small amount of monocyte and lymphocyte. Cerebral cortex swell slightly accompanying with neuron degeneration and lymphocyte infiltration surrounding the small blood vessels. Specimen observation Case abstract:Male, 15 years old. Fever (39.8℃) headache and vomit for 2 days, unconsciousness for 3 hours. Physical examination: stiff neck, Kernig sign (+), petechia can be seen all over the body. WBC in blood 1.2×109/L, cerebrospinal fluid is turbid, WBC in CSF 3.2×109/L, gram-positive cocci can be seen. He was anxious accompanying with twitch and then was dead. Gross specimen: (Fig.14-01a,b) The blood vessels in meninges are dilated and congested. The yellow-tan purulent exudates of acute bacterial meningitis obscure the sulci or covers on the gyrus. Lesions on sulcus are more apparent. Tissue section: (Fig. 14-02a,b) The blood vessels in cerebral pia mater are dilated and congested apparently. The subarachnoid space is filled with a large number of neutrophils, fibrin. Lymphocytes infiltrate surrounding the small blood vessels. What’s the change of CFS? Question: What type of inflammation does epidemic meningitis belong to?. What manifestations can it lead to? If the inflammation was not cure thoroughly, which kind of outcome can be led to? (ⅱ)Epidemic encephatitis B Basic pathologic changes (1) Gross morphology The brain is swollen and the vessels are congested. Diffuse or aggregated small semi-hyaline necrotic lesions can be seen inside the cerebral parenchyma. (2) Histopathology Multiple dispersed small reticular necrosis (liquefactive necrosis). Blood vessels dilate and congest with lymphocyte and monocytes infiltration and formation of perivascular lymphocytic cuffing. Nerve cells degeneration, necrosis, surrounded by proliferated oligodendrocyte, which is called satellitosis; if it is swallowed by microglia, it’s called neuronophagia. Microglia surrounding small vessels or necrotic nerve cells proliferate and form glial nodules. Specimen observation Case abstract:Female, 6 years old. High fever (40.8℃), headache, lethagy for 2 days, coma for 3 hours. Physical examination: stiff neck, Kernig sign (+), Brudzinski sign (+), WBC in CSF 0.1×109/L, lymphocytes 0.9, bacteria (-). She was dead after ineffective emergency treatment. Gross specimen: (Fig. 14-03) There are soften focuses in millet or pin size at deep layer of gray matter, basal ganglia on the coronary section. Tissue section: (Fig. 14-04a, b, c, d) To observe the features of perivascular cuffing, reticular necrosis, satellitosis; neuronophagia and glial nodules. Questions: What is the transmission intermediator and long-term reserve host of epidemic encephatitis type B virus? Which location of brain can be commonly involved and what kind of clinical manifestation may be induced? 2. Tumor of nerve system (ⅰ) Astrocytoma Basic pathologic changes (1) Gross morphology Tumors are in different size, gray and blur boundary; The cut surface is either firm, or soft and gelatinous, cystic degeneration may be seen; Variations in the gross appearance of glioblastoma multiforme from region to region are characteristic. (2) Histopathology Polymorphic tumor cells proliferate diffusively, which can be divided into hair cell type (degree I), fibrous type, primary plasma type (degree II), obesity type (degree II-III). If cell density increase; cell atypia is apparent accompanying with increased mitosis Fig.; blood vessels proliferate, it’s known as anaplastic astrocytoma (degree III). If cell density increase; cell atypia is obvious accompanying with bizarre mononuclear or multinulear giant cells; blood vessels proliferate apparently with hemorrhage, necrosis et al., it’s known as glioblastoma multiforme (degree IV). Specimen observation Case abstract:Female, 40 years old. Headache for 3 years, aggravate and accompany with vomit for 10 days. Physical examination: papilledema. MRI shows mass of pons measuring 6cm×4cm, with blur boundary. She died of brain hernia. Gross specimen: (Fig. 14-05a,b) (a) coronary section of brain, pons is replaced by tumor completely. Cut surface of tumor is gray with blur border. It’s glioma. (b) pleomorphic glioblastoma, coronary section, there is a massive, yellowish gray tumor on one side cerebral hemisphere, with blur border and apparent hemorrhage and necrosis. Tumor also involves the other side of cerebral hemisphere. Tissue section: (Fig. 14-06a,b,c) (a) There is brain tissue on the left side; glioma on the right side, which shows plenty of uniform cells, resembling normal glial cell, without clear border to normal tissue. Blood vessels increase, dilate and congest. It’s fibrillary type. (b) A: fibrillary type; B: protoplasmic type. (c) There are plenty of polymorphous cells, most of which are plump satellite cells with red-stain plasma and asymmetrical nucleus. Bizarre nuclear giant tumor cells can be seen. It’s gemistocytic type. (d) Tumor cells are dense, with dark nucleus and apparent atypia. Necrotic area can be seen, surrounding with tumor cells arranged in barrier form, capillaries proliferate. It’s glioblastoma multiforme. Questions: What about the prognosis of Astrocytoma? Which type has the worst prognosis? (ⅱ) Ependymoma (1) Gross morphology Classic ependymoma is located in the ventricular system, predominantly in the fourth ventricle. Ependymomas appear as well defined, sphere or lobular shape neoplasms with grey cut surface, even or granular texture. Hemorrhage, cystic degeneration or calcification can be seen. (2) Histopathology Ependymomas are generally composed of uniform cells with indistinct cytoplasnic borders and round or oval nuclei. Cells arrange in crypt form or form cavity (rosettes); or arrange around blood vessels (pseudorosettes), with slim processes connecting with vascular wall; some cells form papillary structure. Specimen observation Gross specimen: (Fig. 14-07a,b) (a) Sagittal section, there is a well-defined spheroid mass in the fourth ventricle, with gray cut surface, even texture and local hemorrhage. (b) Horizontal section, please observe and describe by yourself. Tissue section: (Fig. 14-08) Tumor cells surround vascular cavity to form pseudorosettes. Tumor cells are in carrot shape, slim processes attach to vascular wall. Question: What are the differences between astrocytoma and ependymoma? (ⅲ) Meningioma Basic pathologic changes (1) Gross morphology Meningioma is located in both sides of superior sagittal sinus, sphenoid crest, olfactory sulcus and spinal cord; Meningiomas are generally spherical. Most meningiomas have a smooth or slightly lobulated surface and a rubbery consistency with solid texture. They are gray, granular or reticular. (2) Histopathology Tumor cells surround blood vessels in concentric circle or whirlpool shape. Central vessels suffered hyaline degeneration and even calcify into Psammoma bodies; Meningioma exhibits a wide range of histological patterns and a single meningioma may show a combination of patterns. The meningothelial, transitional, and fibrous variants are the predominate patterns. Specimen observation Gross specimen: (Fig. 14-09a,b) (a) There is a reddish-yellow firm neoplasm in one side of sagittal sinus, with granular capsule. (b) To observe and describe by yourself. Tissue section:(Fig. 14-10a,b) (a) Transitional type, tumor cells surround blood vessels in whirlpool shape. (b) Meningothelial type, tumor cells arrange in concentric circle form, at the center of which psammoma bodies can be seen. Question: What are the main influences on body of meningioma? (ⅳ) Neurilemmoma (Schwannoma) Basic pathologic changes (1) Gross morphology Neurilemmoma are round of nodular shape, capsulated. The cut surface is often gray or yellow-tan, sometimes multi-colored resulting from hemorrhagic focus or hemorrhagic cyst formation. (2) Histopathology There are two histological types Antoni A type: tumor cells are spindle-shaped with blur border, rod-shaped nuclei. Tumor cells are arranged in compact intertwining fascicles (palisading appearance). It’s known as verocay body. Antoni B type: tumor cells are sparse arranged loose reticular structure. There is much myxoid substance with sac formation. Specimen observation Gross specimen: (Fig. 14-11a,b) To observe and describe by yourself. Tissue section: (Fig. 14-12a,b) In left area, cells are abundant, arrange in barrier form. Nuclear are surround by purple substance (verocay body). It’s “Antoni A” area. In right area, cells are sparse. Stroma is loose accompanying with myxoid degeneration. It’s “Antoni B” area. Question: How to distinguish neurilemmoma from leiomyoma and fibroma in morphological or immunohistochemical aspect? CASE DISCUSSION Case one Case abstract. Boy, two years old, high fever and twitch. He suffered poor consciouness and appetite accompanying with mild cough. He underwent high fever and ejective vomitting one day ago. Then he suffered dysphoria and twith. Past history is normal. Physical examination. T39.7℃,P 132/min, R32/min, BP 10/6.5kpa. Acute expression, opisthotonus. There are many pin-size petechia on his back skin accompanying with plump anterior fontanelle, stiff neck and tachypnea, mild wheezing in lower field of both lungs. Boundary of heart is normal; rhythm of the heart is regular without cardiac murmur. Soft abdomen, mild hepatosplenomegaly, Kernig sign (+), Brudzinski sign (+). Laboratory examination. WBC 20.8×109/L, polymorphonuclear leukocyte 81%, rod neutrophil 13%, lymphocyte 5%, eosinophilic granulocyte 1%, CO2 combinding ability 25vol%. CSF examination: pressure 268mmH2O, light yellow, turbid, cell amount 25000/mm3, total protein 140mg%, chloride 420mg%. Bacteria culture: Diplococcus pneumoniae are seen. Blood smear of dorsal petechia: gram-positive cocci can be seen. Treatment history. After inhospitalization, he received therapies of correcting Water-Electrolyte disorder and acidosis, broad-spectrum antibiotic and hormone treatment. Body temperature restore to normal for a time. Then this boy was coma accompanying with unstable BP. The dorsal petechia increased and aggregated suddenly with BP decrease. The he was dead. Autopsy abstract. (Fig. 14-13) Vessels on the surface of brain dilate and congest severely; subarachnoid space is turbid with aggregation of grey suppurative exudation. Both adrenal hemorrhage (Fig. 14-14). There are some grey focuses at the lower lobes of both lungs. Microscopically, bronchiole and surrounding alveolar cavities are filled with neutrophils (Fig. 14-15). Cross striation of myocardium disappear. Hepatocytes are swelling accompanying with purple granules in cytoplasm. Fatty vacuoles can be seen. Questions. 1. According to above case report, give a diagnosis. 2. What’s the relationship among the pathological changes in autopsy? 3. What’s the relationship between clinical manifestations and pathological changes? 4. To discuss the death reason of this case. Case two Case abstract. A 33-year-old male with a long history of epilepsy was evaluated for a seizure. A general neurologic examination was unremarkable. Radiology studies of the brain revealed a right frontal mass. MRI images showed a homogeneously enhancing subfrontal extra-axial mass measuring 3.5×2.3×2.0cm located right to the midline with surrounding edema, minimal midline shift and mild deformity of the right frontal horn (Fig. 14-16). The lesion was broad based with dural extension into the anterior falx. Sagittal images showed irregular margins at the brain interface suggesting an intra-axial component. At the time of surgery, the frontal cortex was noted to have a "rock" hard consistency. Microscopic changes. (Fig 14-17a,b,c,d) Please observe ①How many kinds of cell components in this tumor? ②What is the dense blue structure in Fig14-17d? ③What can be inferred from the polymorphism of this tumor? Questions. 1. What is your pathological diagnosis of this case? Why? 2. According to this case, please talk something about how to estimate the malignancy of intracranial tumor? PRACTICE REPORT 1. Illustrate the microscopic appearance of epidemic encephalitis B. 2. Description (1) The gross specimen of purulent meningitis; (2) The microscopic appearance of meningioma and neurilemmoma. 3. To write the discussion epitome of each case. QUESTIONS FOR REVIEW 1. What are the differences between epidemic meningitis and type B epidemic encephalitis? 2.As for clinical treatment, what differences should be considered between tumor originated from central nerve system and from the other system? ( China Medical University Li Qingchang, Tang Na, Liu Yang)