HBImmunity
advertisement
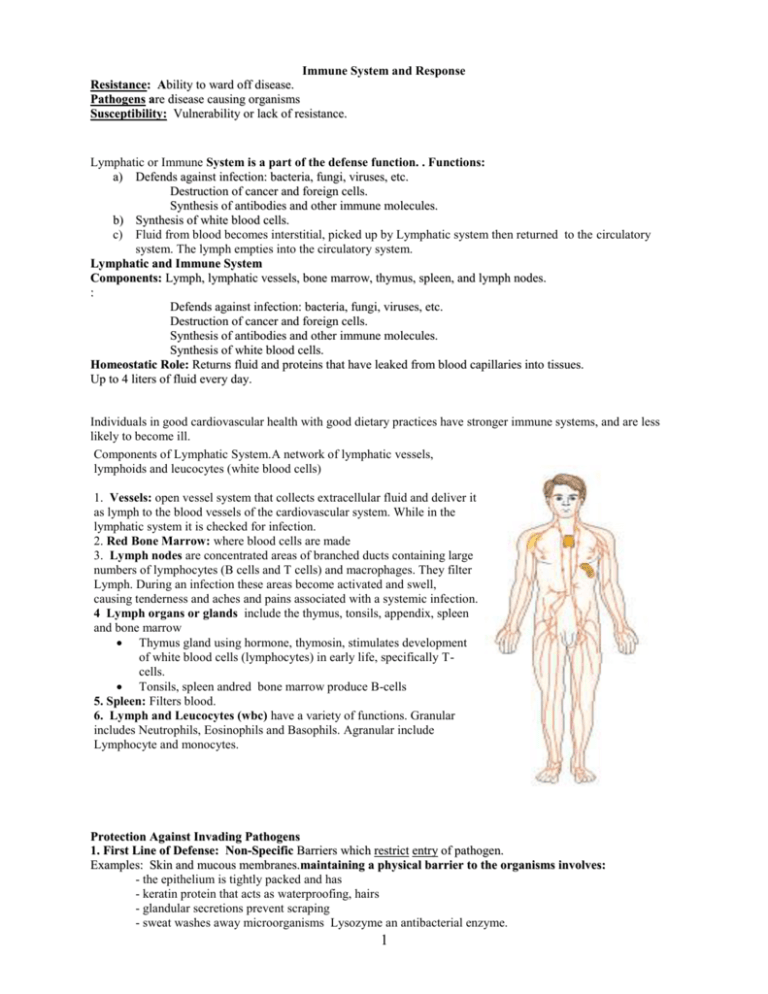
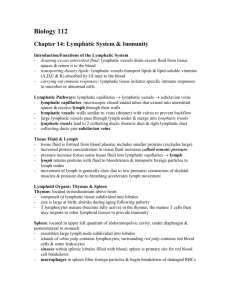
Immune System and Response Resistance: Ability to ward off disease. Pathogens are disease causing organisms Susceptibility: Vulnerability or lack of resistance. Lymphatic or Immune System is a part of the defense function. . Functions: a) Defends against infection: bacteria, fungi, viruses, etc. Destruction of cancer and foreign cells. Synthesis of antibodies and other immune molecules. b) Synthesis of white blood cells. c) Fluid from blood becomes interstitial, picked up by Lymphatic system then returned to the circulatory system. The lymph empties into the circulatory system. Lymphatic and Immune System Components: Lymph, lymphatic vessels, bone marrow, thymus, spleen, and lymph nodes. : Defends against infection: bacteria, fungi, viruses, etc. Destruction of cancer and foreign cells. Synthesis of antibodies and other immune molecules. Synthesis of white blood cells. Homeostatic Role: Returns fluid and proteins that have leaked from blood capillaries into tissues. Up to 4 liters of fluid every day. Individuals in good cardiovascular health with good dietary practices have stronger immune systems, and are less likely to become ill. Components of Lymphatic System.A network of lymphatic vessels, lymphoids and leucocytes (white blood cells) 1. Vessels: open vessel system that collects extracellular fluid and deliver it as lymph to the blood vessels of the cardiovascular system. While in the lymphatic system it is checked for infection. 2. Red Bone Marrow: where blood cells are made 3. Lymph nodes are concentrated areas of branched ducts containing large numbers of lymphocytes (B cells and T cells) and macrophages. They filter Lymph. During an infection these areas become activated and swell, causing tenderness and aches and pains associated with a systemic infection. 4 Lymph organs or glands include the thymus, tonsils, appendix, spleen and bone marrow Thymus gland using hormone, thymosin, stimulates development of white blood cells (lymphocytes) in early life, specifically Tcells. Tonsils, spleen andred bone marrow produce B-cells 5. Spleen: Filters blood. 6. Lymph and Leucocytes (wbc) have a variety of functions. Granular includes Neutrophils, Eosinophils and Basophils. Agranular include Lymphocyte and monocytes. Protection Against Invading Pathogens 1. First Line of Defense: Non-Specific Barriers which restrict entry of pathogen. Examples: Skin and mucous membranes.maintaining a physical barrier to the organisms involves: - the epithelium is tightly packed and has - keratin protein that acts as waterproofing, hairs - glandular secretions prevent scraping - sweat washes away microorganisms Lysozyme an antibacterial enzyme. 1 - cells produce mucus, acids - urine flush passageways 2. Second Line of Defense: non-specific Local response to pathogen after it has entered body engages Lympatic System: does not distinguish between infectious agents and involves Examples: , phagocytes (macrophages and neutrophils), Fever inflammation, and antimicrobial proteins interferon. White blood cells attack invading organisms: - phagocytes remove pathogens by cell-eating. - natural killer cells survey tissue for normal and abnormal cell. An abnormal cell (cancer cell) when detected is bombarded with a protein that causes cell lysis. Chemical Warfare during non-specific defense -Interferon proteins are antiviral compounds that interfere with replication -Complement protein activation, enhances phagocytosis, destroys the membranes of invading cells and promotes inflammation. -Histamine and heparin proteins promote inflammation to create or repair a barrier, slowing the spread of pathogens. They increase blood flow causing swelling, redness, heat and pain. -Fever is regulated by nerve cells in the hypothalamus. Infections, invasions reset the thermostat. High body temperature speeds up the activities of the immune system. Prolonged high fevers disrupt or damage organ systems. Inflamation response is stimulated by Basophil and Mast Cells . These cells release chemical signals: Histamine and other molecules. This causes a Local response to chemical signals: Increase in local blood flow and vascular permeability, Redness, Heat, Swelling, Pain Phagocytic white blood cells come into area: Engulf bacteria, dead cell parts, and other microbes. Tissue heals 3. Third line of defense: Specific defense protects against one type of infection. Uses Lymphocytes and Antibody. Engages B and T cells.It involves the antigen-antibody response that creates a type of memory. The specific response is more effective. It is characterized by specificity, memory and prompt response to an antigen. Immunity: “Free from burden”. Ability of an organism to recognize and defend itself against specific pathogens or antigens. ACTIVE Immunity ● The individual’s body makes antibodies against a particular antigen ● This can happen through natural infection or through immunization involving vaccines ● Primary exposure is shorter-lived and slower to respond while a secondary exposure is a rapid, strong response ● This type of immunity is usually long-lasting ● It depends on memory B and T cells PASSIVE Immunity ● An individual is given prepared antibodies against a particular antigen ● This type of immunity is short-lived ● This can happen naturally as antibodies are passed from mother to fetus or artificially via an injection of antibodies Immune Response: Involves production of antibodies and generation of specialized lymphocytes against specific antigens. It involves antigen/antibody binding An Antigen is any molecule that elicits a response. In terms of pathogens these molecules are on the surfaces of viruses, bacteria or fungi (molds). Often they are proteins but can be other molecules. Antibodies are found in our body fluids: Blood, Lymph, Interstitial fluid 2 An antibody is produced specific to the antigen. The antigen remains in the system (blood and lymphatic system). On a second invasion, the antibody recognizes the antigen. Antibodies can be passed from one individual to another: Mother-child: Mother’s antibodies cross placenta. Also found in breast milk. Serum: Snake bite antivenom. Vaccination or Immunization: Process in which harmless forms of antigen or pathogen are introduced into body to provoke an immune response. Types of Leukocytes: Granular (include Neutrophils, Eosinophils, Basophils) Agranular ( Leukocytes and monocytes) Order of Population Density (Never Let Monkeys Eat Bananas) Cell Type Main Characteristics Macrophage Neutrophil Phagocyte; acts in nonspecific and specific responses; presents antigen to T cells, cleans up Fast-acting phagocyte; takes part in inflammation, not in sustained responses, and is most effective against bacteria. Most abundant. Secretes cytokines. Secretes enzymes that attack certain parasitic worms Eosinophil Basophil and Secrete histamine, other substances that act on small blood mast cell vessels to produce inflammation; also contribute to allergies Dendritic cell Lymphocytes: Cytotoxic T cell Processes and directly presents antigen to helper T cells All take part in most immune responses; after antigen recognition, clonal populations of effector and memory cells form. Effectors secrete five types of antibodies. Plasma and Memory Types Effectors secrete interleukins that stimulate rapid division and differentiation of both B cells and T cells Effectors touch-kill infected cells, tumor cells, and foreign cells Natural killer (NK) cell Cytotoxic cell of undetermined affiliation; kills virus-infected cells, bacteria, and altered body cells by a touch-kill mechanism B cell Helper T cell How Lymphocytes form: Stem Cells for all blood cells are found in Red Bone Marrow. Colony Stimulating Factor direct stem cells to become WBC. These further differentiate into a diverse population of WBC. B- Cell form and mature in bone. T-cells leave bone and mature in the thymus. Two Types of Specific Responses involving B or T lymphocytes 1. Humoral Response. Substances from cells are released into the blood Lymphocytes are also derived from stem cells in the bone marrow. They include: B cells, involves the humoral response, carry the antibody to the plasma, cells or interstitial fluids. B cell have antigen receptors (antibodies) attached to their outer surfaces. Upon invasion by pathogen, they bind to the antigen. They are then stimulated to proliferate. Now, all of these identical effector cells secrete specific antibodies. Once antibody/antigen binding occurs there is precipitation out of solution and attack by phagocytes or activation of complement proteins that lyse invaders. Helper T-cells use cytokines to stimulate Clonal Selection and Expansion. At that time B-cell either produce a new lineage of plasma B and memory or the recruit an existing memory B and make many clones of it. Most will become plasma B and release antibody into plasma and others will become memory B. 2. Cell Mediated Response T cells, involved in cell mediated response, travel inside bloodstream. They destroy cancer cells, self cells infected with fungi, viruses, protozoans, and bacteria. T helper cells: Play a central role in immunity. Act indirectly by controlling the immune functions of other cells: Increased antibody production by B cells. 3 Increased phagocytosis by macrophages. There are several types of T cells. Killer T-Cells (or Cytotoxic T-cells, CTL, recognize and attack pathogen-infected cells and are the only T cells that kill. They kill with complement protein or with the porforin protein. Helper T (T4 or CD4) cells must be activated. Once activated they secrete interleukin proteins to promote an immune response. For example the secretion of interleukin-2 amplifies both the humoral and cell-mediated response, bringing into play B-cells. Suppressor T-Cells (T8 or CD*) suppress the activity of other lymphocytes so they don’t destroy normal tissue APC= antigen presenting cells: these cells ingest a microbe and display both a self-protein/foreign antigen on its surface. Helper T-cells bind to this complex and are as a result activated to produce interleukin-2 and stimulate the production of cytotoxic T cells and B-cells (humoral response). These cells destroy the foreign cell. Overall: Our cells have fingerprints and the immune system depends on recognizing the fingerprints. It has to distinguish “self from non-self”. It is the proteins that are on the plasma membrane that determine self. These proteins are inherited in the genes. Therefore, only identical twins can have identical set of self-proteins. Organ transplants are rejected because of the differences in self-proteins. Organ rejection is minimized by finding a donor with matching self-proteins and/or using drugs that suppress the immune response. You can imagine the other complications caused by suppressing the immune response. Disorders of the Immune System 1.Autoimmune diseases the immune system turns against its own body cells (rheumatoid arthritis, insulin dependent diabetes, Crohn’s, lupus) Autoimmune diseases can each affect the body in different ways. For instance, the autoimmune reaction is directed against the brain in multiple sclerosis or the gut in Crohn's disease or destruction of insulin-, producing cells of the pancreas in Type 1 diabetes mellitus. In other diseases, such as systemic lupus erythematosus (lupus), affected tissues and organs may vary among individuals with the same disease. 2.Allergens elicit the production of IgE antibodies. These antibodies promote the production of histamine. Hypersensitivities to harmless substances such as pollen, food or animal hair. Histamines are produced in amounts greater than normal causing symptoms like nasal irritation, itchiness and tears. Antihistamines interfere with histamine action and give temporary relief. Excessive release of histamines can cause anaphylactic shock which can lead to death. 3.AIDS is caused by HIV a RNA virus. HIV attacks T-helper cells destroying the humoral and cell-mediated immunity. Currently treatment with the triple cocktail postpones the development of AIDS. New approaches to treatment include injecting patients with HIV-resistant stem cells and the development of a vaccine. Concerning AIDS due to HIV infections, helper-T-cell count is most important. A blood test showing the number of T4 cells you have tells you how health your immune system is especially for AIDS and when to start taking the medications. T4 cells are the main target of HIV. Normal T4 count is between 500 and 1500 cells/mm3. Individuals with AID show a drop of 50 to 100 cells per year. T4 below 200 allows for opportunistic infections (Pneumocystis carinii pneumonia). Individuals with T4 counts around this level should begin prophylactic treatments (prevents opportunistic infections). T4 counts 350 and lower are a good time to start the anti-Hiv therapies. 4. Tissue REJECTION: This can occur when cytotoxic T cells respond to tissue that is not recognized as “self” tissue . Controlled by giving patients immunosuppressive drugs and by transplanting organs that have the same MHC proteins in the donor and recipient. 5. SCIDS 4