Understanding referrals - London Cancer Alliance
advertisement

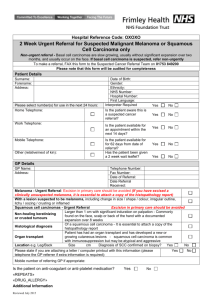
Understanding Referrals An overview for Primary Health Care Teams 1. The NICE Referral Guidelines What are the guidelines? Referral guidelines for primary care for suspected cancer were first published by NICE in 2000. Improvements have been made in the timely diagnosis and treatment of cancer patients, however some patients with suspected cancer are still not being referred urgently which leads to a delay in treatment. The national guidelines have now been updated to better help practitioners distinguish between symptoms associated with common illnesses, and those that might indicate cancer. The revised guidelines cover the referral processes for the following tumour types: Lung Upper and lower GI Breast Gynae Urological Haematological Skin Head and Neck incl. thyroid Brain and CNS Bone cancer and sarcoma The guideline also considers cancers seen in children and young people, and support and information needs for patients. The full suite of information can be viewed on the NICE website at: http://www.nice.org.uk/page.aspx?o=261649. Copies of the Quick Reference Guide for clinicians and information for the public are included on this CD-Rom. How do the changes affect Primary Health Care Teams? The guidelines contain changes to the criteria for urgent suspected cancer referrals, with additional information to support other types of referrals and the management of patients within primary care. The urgent referral fax proformas used by GPs in South East London have been modified to reflect these changes, and are available from the Cancer Network website www.selcn.nhs.uk. Click here for more information about urgent referrals. Primary Health Care Teams are also required to provide information and support to patients during the referral process. This includes information about the possible diagnosis and where they are being referred to, and providing culturally appropriate care. Click here for more information about patient information and support. 2. In the consultation The NICE guidance states that GPs should be familiar with and able to readily identify the typical presenting features of cancers, and take part in continuing education, peer review and other activities to improve and maintain these skills. GPs should review the patient history, examination and initial diagnosis and refer if necessary when common symptoms do not resolve as expected, if confronted by unusual symptom patterns or if patients thought not to have cancer fail to recover as expected. Cancer is uncommon in children, and its detection can present particular difficulties. GPs should listen carefully to the concerns of parents, and discuss the diagnosis with a colleague or specialist when a child fails to recover as expected, or there is uncertainty about how to interpret the symptoms and signs. Page 1 of 5 Understanding Referrals An overview for Primary Health Care Teams The information and support needs of the patient should be assessed during the consultation – click here for more information. 3. How to refer patients Immediate referrals Admission to an acute Trust or a referral occurring within a few hours, or even more quickly if necessary, should be made when a patient presents with severe or life threatening symptoms. The guidelines indicate which clinical symptoms are appropriate for an immediate referral, and these are included for information on the urgent suspected cancer referral proformas. Urgent referrals (Two Week Wait) A patient who is referred urgently is seen within the national target – currently two weeks. This route should be used for patients in whom the GP suspects cancer. The revised NICE guidelines set out the clinical symptoms and findings that are appropriate for urgent referral. To make an urgent referral the GP should complete the SELCN urgent referral proforma and fax it to the relevant hospital within one working day of seeing the patient. Revised proformas are available on this CD-ROM. The proforma is a two-page document – the front side is used to record the patient details and clinical information, the reverse contains the referral criteria and other supporting information. Only the front sheet needs to be faxed. Additional relevant information can be included on separate pages if necessary. Please include a print out of the patient’s computer record summary of relevant past medical and social history, medication and allergies when available. In most places a central appointments team receives the faxes, and phones the patient the next day to confirm an appointment time within the next two weeks with them. If patients cannot be contacted by phone the appointment details are sent in the post. Patients will also be sent some basic information about who will see them and whether they will have tests. Adults should normally be told that they are being referred to a cancer service, but if appropriate provide reassurance that most people who are referred will not turn out to have a diagnosis of cancer. At the very least your patient should be aware that they will be offered an appointment within the next two weeks. A simple leaflet to support this conversation is available on this CD-ROM for GPs to use. Non-urgent All other referrals are classed as non-urgent. The urgent suspected cancer referral proformas also contain information on which clinical symptoms are appropriate for a non-urgent referral. Non-urgent referrals should be made by letter or using the new Choose & Book system within one working day of seeing the patient. Be sure to include all appropriate information in referral correspondence, as the referral will be vetted by clinical teams at the hospitals and prioritised according to urgency of the signs and symptoms. Page 2 of 5 Understanding Referrals An overview for Primary Health Care Teams 4. Patient information and support The revised NICE guidelines make a number of recommendations about the support and information that should be offered to a patient at the time of referral. Assessing patient needs Primary healthcare professionals should provide culturally appropriate care, recognising the potential for different cultural meanings associated with the possibility of cancer, the relative importance of family decision-making and possible unfamiliarity with the concept of support outside the family. Ensure patients are able to consult a primary healthcare professional of the same sex, if preferred. Discuss with patients (and carers as appropriate) their preferences for being involved in decision-making about referral options and further investigations (including risks and benefits). Take into account personal circumstances, such as age, family or work responsibilities, isolation, or other health or social issues. Referring the patient Normally tell adults that they are being referred to a cancer service, but if appropriate provide reassurance that most people who are referred will not turn out to have a diagnosis of cancer. In children and young people, discuss the referral decision and any information needs with the parents or carers (and the patient, if appropriate). Follow current advice on communicating with patients and/or their carers and breaking bad news. The primary healthcare professional will be aware that some patients find being referred for suspected cancer particularly difficult because of their personal circumstances, such as age, family or work responsibilities, isolation, or other health or social issues. Inform the specialist of any additional support needs, with the patient’s agreement. In situations where diagnosis or referral has been delayed, or there is significant compromise of the doctor/patient relationship, take care to assess the information and support needs of the patient, parents and/or carers, and make sure these needs are met. Give the patient an opportunity to consult another primary healthcare professional if they want to. “I felt like I was causing trouble…” (Bexley patient) “The GP didn’t try to find out why I was in pain…” (Southwark patient) Page 3 of 5 Understanding Referrals An overview for Primary Health Care Teams After the consultation Assess the patient’s need for continuing support while waiting for their referral appointment. Invite the patient to contact you again. “My GP has offered me support while being treated…” (Southwark patient) Consider the information and support needs of patients and the people who care for them. Have information available in a variety of formats on both local and national sources of support. Be aware that men are likely to have similar support needs to women, but may be more reticent about using support services. Useful resources for GPs Information on tumour types More information about tumour types and the tests a patient might have is available from Cancer BACUP – call 0808 800 1234 or visit the website: www.cancerbacup.org.uk. Cancer Service Directories Several acute Trusts have produced a Directory of Cancer Services for primary health care teams to use. They are available on this CD ROM, along with other local information directories. Breaking Bad News The Cancer Network has summarised guidelines for breaking bad news to a patient in a leaflet. The summary and the full guideline are available on this CD-ROM. Cancer patients and carers across South East London, in partnership with Macmillan and the Cancer Network, have made a video documenting how significant news was broken to them, and how their experience could have been improved. Copies will be available in Primary Care and Acute Trusts to use with clinical and management teams. For more information contact Bonnie Yandall, User Partnership Facilitator for the Cancer Network, on 020 7593 0160 / bonnie.yandall@selondon.nhs.uk. Patient experience of referrals The user partnership group in Bromley (known as Voices In Bromley) identified the initial part of many cancer patients journey - where patients become aware of symptoms, go to their GP and are referred to hospital - as an area they would like to improve. They asked patients from other parts of South East London about their experiences of GP consultations and referrals, collated the results and are now identifying ways to improve the referral process. The full report is available on this CD ROM. For more information please contact Pip Wittenoom, Primary Care Service Improvement Facilitator for the Cancer Network, on 020 7593 0160 / pip.wittenoom@selondon.nhs.uk. Page 4 of 5 Understanding Referrals An overview for Primary Health Care Teams 5. National waiting times targets First seen for suspected cancers GP referral for suspected cancer Diagnostic phase (CT, MRI, endoscopy, biopsy, etc) and MDT First Treatment Decision to Treat made 14 days 31 days for all cancers 62 days for all cancers from urgent GP referral. There are three Cancer Waiting Times targets that Acute and Primary Care Trusts are actively being monitored against: All urgent cancer referrals from GPs seen within two weeks (14 days) 31 days from cancer diagnosis to treatment for all patients 62 days from urgent cancer referral by a GP to first treatment. Across South East London we are routinely achieving the two-week target for urgent referrals and in most cases the 31-day target from diagnosis to treatment. Over 90% of urgent referrals are treated within 62 days, and a great deal of work is going into improving these results for all patients. 6. Feedback & Performance Management Each Acute Trust cancer multidisciplinary team is required to provide information to referring GPs and other PCTs on the ‘appropriateness’ and timeliness of urgent suspected cancer GP referrals. In this context the term appropriate means whether the referral has been made in accordance with the agreed referral criteria listed on the reverse side of the referral proforma. The Acute Trusts should also monitor and feed back to PCTs and individual GPs the number of patients referred as urgent, proportion of urgent referrals who are subsequently found to have cancer, and numbers of routine referrals who are found to have cancer. Some Trusts in South East London already have these audit and feedback processes in place, while others are developing them at present. Nationally, studies show that 15 -20% of patients referred as urgent suspected cancer referrals are diagnosed with cancer. An ongoing area of concern is that many patients who do have cancer are not being referred on the 2-week route. As a local example, approximately 5% of patients referred with suspected colorectal cancer are subsequently diagnosed with cancer, and up to 74% of patients who do have colorectal cancer are not referred urgently. Page 5 of 5