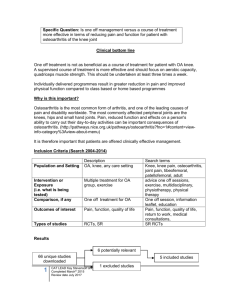
A review of osteoarthritis of the trapeziometacarpal
advertisement

A review of osteoarthritis of the trapeziometacarpal joint (TMJ) Nicole Murphy Bhoomiah Dasari Jo Adams Introduction Osteoarthritis (OA) is a degenerative joint disease of diarthrodial joints, characterised by deterioration of articular cartilage and the formation of new bone growth at joint margins and joint surfaces (Tortora and Grabowski 2003). It is an age associated, mechanically driven disorder that is likely to increase in prevalence in the coming years (Dieppe 2000). It is the most common joint disorder in the western world, present in the majority of people aged 65 years and in 80% of those aged 70 years and over (Arden et al 2006), Autopsy has shown universal evidence of osteoarthritis changes in the over 65s but yet only 60-70% of those present themselves for medical treatment highlighting that osteoarthritis is more of a problem than just those currently receiving treatment (Kraus 1997). Estimates suggest that 16-22% of females and 2-5% of men have OA (Swiggart et al 1999). The disease frequently involves hand joints, in particular the carpometacarpal joint of the thumb (CMJ) (Creamer and Hochberg 1997) and the incidence of hand OA increases with age (Wilder et al 2006). Women have higher rates of hand OA than men (Szoeke et al 2006), in part because women tend to have more severe polyarticular OA that frequently affect the hands and knees (Hirsh 1996, Wilder et al 2006, Stevens and Finlayson 2005).The distal 1 interpahlangeal, proximal interphalangeal and carpometacarpal joints of the hand may all be affected in OA (Wilder et al 2006) and of all individuals diagnosed with osteoarthritis of the hand 25% have isolated osteoarthritis of the Trapeziometacarpal joint (TMJ) of the thumb (Mannoni et al 2000). Healthy men with the strongest grip strengths have an increased risk of developing OA at both the thumb base joints and the proximal interphalangeal and metacarpophalangeal joints (Chaisson et al 1999). Joint hyper mobility does not appear to be a risk factor in developing OA at any hand joint (Kraus et al 2004). Current estimates suggest that OA affects the carpometacarpal joints of 21% of healthy community dwelling women aged over 40 years (von Schroeder 2003, Wilder et al 2006). The progressive nature of TMJ can produce symptoms of pain over the thenar eminences, swelling, and stiffness of the thumb, weakness and in more chronic cases deformity. All these symptoms ultimately lead to a gradual loss of dexterity, precision grip strength and hand function (Roberts et al 2001, Dominick et al 2005). Despite the vast amount of research into the aetiology of osteoarthritis the aetiology remains elusive (Creamer and Hochberg 1997) Disease Severity Osteoarthritis of the Carpometacarpal joint has been classified into four subgroups which classify the severity of the disease (Table 1). 2 Management of the TMJ of the thumb There are three main areas in the management of osteoarthritis of the Carpometacarpal joint of the thumb. These being hand therapy (splinting, patient education, exercise, joint protection and acupuncture), drug therapy (NSAIDs and steroid injections) and surgery (Arthrodesis and Arthroplaty) (Creamer et al 1998, Swigart et al 1999, Damen et al,2001, Stamm et al 2002, Meenagh et al, 2004, Degreef and De Smet 2006). Currently there are no guidelines into the management of osteoarthritis of the carpometacarpal joint of the thumb Splinting Splinting appears to be the preferred conservative treatment for OA of the carpometacarpal joint (Berggren et al 2001; Weiss et al 2000). However there is limited evidence into their use with most of the studies being retrospective rather than randomised controlled trials. Swigart et al’s study (1999) examined retrospectively the effects of splinting on 130 thumbs with varying stages of carpometacarpal joint osteoarthritis. Some patients received surgical intervention. Patients were excluded if they had been treated with exercise or steroid injections making it one of the few studies looking at the effects of a single technique. The intervention consisted of splinting the thumb with a long thumb stabilizer for 3-4weeks, with 3-4weeks period of weaning. In milder forms of OA, stages I and II, 76% benefited from some symptomatic improvement. In the more severe cases of OA, stages III 3 and IV, 54% benefited from some symptomatic improvement. The benefits were maintained in the short term, 60% feeling the benefits immediately and 59% still benefiting 6months later. Although retrospective the study provided some evidence that splinting may delay or prevent the need for surgical intervention. Day et al (2004) investigated the effectiveness of a single corticosteroid injection followed by a three week period of splinting. This study looked at 30 thumbs and evaluated improvements in both self-reported functional ability using the Disabilities of the Arm, shoulder and Hand questionnaire (Hudak et al 1996) and visual analogue scales for pain scores. This study discovered that long term relief from the symptoms of OA could be achieved in stage I OA but less than 25% of those suffering with stage IV benefited from a one off corticosteroid injection. Overall 40% of participants received symptomatic improvement that was considered sufficient and sustained irrespective of their stage. Joint Protection & Exercise Joint protection is a well-recognised technique in the management of rheumatoid arthritis but has not been widely reported as being used in other musculoskeletal conditions. There is limited published evidence of the effectiveness of applying joint protection techniques in osteoarthritis. Stamm et al (2002) carried out the initial randomised controlled trial. Forty patients were recruited onto the trial. The control group was provided with non-slip matting which they were to use when opening jars as well as oral and written 4 information on OA. The intervention group received both oral and written information on joint protection and a hand exercise programme. The joint protection instruction and training lasted for 30 minutes per patient. Assistive devices for Activities of Daily Living were also provided. Assessment of grip strength and self-report functional ability were carried out at baseline and at three months post intervention. There were statistically significant more patients who improved grip strength by at least 10% changes in the joint protection group than in the control group, although self-report pain levels and general functional ability was no different between groups. Although unlikely to be fully powered this randomised controlled trial does provide early evidence that straightforward, uncomplicated joint protection advice and home hand exercises does have the potential to impact on hand function in OA affecting the hand. Surgical management TMJ of the thumb is the most common site for which surgery is sought because of the profound impact on hand function and disabling symptoms (Pellegrini 1992), making it difficult to do simple household tasks, such as turn door knobs and open jars. As most of the surgical treatments offer satisfactory results with respect to relieving pain, restoring stability and strength, choosing the appropriate surgical technique can be challenging to both hand surgeons and the hand therapists. The first line of treatment of the TM joint arthritis is the use of nonsurgical modalities such as drug therapy, rest, splinting and patient education. When 5 such measures are no longer sufficient to control the progressive nature of the osteoarthritis or to keep symptoms at an acceptable level, surgical procedures become an option. In order to deal with such problems as pain, swelling and decreased strength and range of motion, a number of surgical alternatives have been developed to improve patient’s function and quality of life. It is shown that surgery has been responsible for a dramatic improvement in the quality of many with osteoarthritis (Turner, Foster and Johnson 2004). In most cases of osteoarthritis of the TM joint, surgery becomes an option at stages II, III, and IV, as classified by Eaton and Glickel (1987). The available surgical treatments include arthrodesis and excision of part or the entire trapezium combined with interposition of fascia, tendon, Gortex, silicon or metal implants (Belcher and Nicholl 2000). Gervis (1949) first reported the use of trapeziectomy for this condition and many other have reported high success since then (See for example, Gervis 1973, Iyer 1981, Dhar et al 1994, Hollevoet et al 1996, Vandenbroucke et al 1997). The evidence however suggests that although trapeziectomy is the method of choice for treating osteoarthritis at the base of the thumb, it has a reputation for causing instability, weakness and loss of power of the thumb (Murley 1960, Kvarnes and Reikeras 1985, Burton and Pellegrini 1986, Necking and Eiken 1986). The review of the literature suggests that despite many improvements in the surgical techniques, controversy still exists regarding which technique achieves the best outcome (Glyka, Karen and Achilleas 2004) and as such there is no 6 consensus in the literature as to which clinical outcomes are most important in thumb basal joint surgery and how these should be measured and documented. To address the question, Glyka, Karen and Achilleas (2004) undertook a systematic review. Based on their search strategies, these authors concluded that for stage II, the arthrodesis seems to be the choice of treatment, especially for young, posttraumatic, high-demand hand. This is followed by the osteotomy and trapeziectomy with or without interposition/ligament reconstruction. As far stage III & IV are concerned, the majority of their reviews support the same choice as the stage II except osteotomy, which was replaced by total joint arthroplasty. Overall, ligamentous reconstruction and tendon interposition appeared to be the most popular choice for stages III & IV. From the review, it is also noted that some studies have indicated that there is no difference in outcome between the techniques with the chosen technique often being at the surgeon’s discretion (Schroder et al 2002, Martou et al 2004, Taylor et al, 2005). Current research has suggested that there are a number of predisposing factors that will affect the outcome of surgery. Evidence has found that age, the presence of MCP hyperextension and web angle retraction, provide poorer results (Degreef and De Smet, 2006). With several of these factors being secondary complications of OA earlier intervention appears to provide more satisfactory results. While recognising the importance of systematic reviews & standardised protocols, authors of this paper believes that no conclusions on the superiority 7 of a single technique over other techniques are drawn without properly conducted comparative studies and randomised controlled trails, preferably with large sample size. Implications for Practice Evidence has suggested that although conservative management will not cure OA of the carpometacarpal joint of the thumb it appears to provide some form of symptomatic relief in most patients. The evidence suggests that the management technique chosen will reflect the stage of osteoarthritis for each individual. In early stage OA conservative management such as splinting, corticosteroid injections, joint protection and exercise appears to be beneficial. However in later stage OA, although conservative management can be attempted, there is a poorer outcome of surgery if secondary affects of OA have developed. In these cases it has been suggested that surgery is a more beneficial option. 8 Table 1: Stages of disease severity for OA of the CMCJ Stage Description Stage 1 Normal articular contours; joint space may be widened due to effusion or laxity of the ligamentous support of the basal joint. Stage 2 Joint space slightly narrowed. Minimal sclerosis of the subchondral bone. Mild/moderate subluxation. Osteophyte formation may be present. Stage 3 Further narrowing. Osteophyte formation. Moderate subluxation. Hyperextension at MCP joint. Stage 4 Presentation similar to stage III. Thumb immobile. Little pain experienced. Scaphotrapezial joint often shows osteoarthritis changes. (Eaton and Glickel 1987) 9 References Arden N, Nevitt MC (2006) Osteoarthritis: Epidemiology. Best Practice and Research in Clinical Rheumatology 20(1):3-25. Belcher HJ, Nicholl JEA (2000) A comparison of trapeziectomy with and without ligament reconstruction and tendon interposition. Journal of Hand Surgery. (Br.) 25B: 350-356. Berggren MJ, Davidson A, Lindstrand J, Nylander GP (2001) Reduction in the operation after conservative treatment of osteoarthritis of the first carpometacarpal joint: A seven year prospective study. Scandinavian Journal of Plastic and Reconstructive Surgery and Hand Surgery 35(4): 415-417. Burton RI, Pellegrini VD 1986) Surgical management of basal joint arthritis of the thumb ( Part II): Ligament reconstruction with tendon interposition arthroplasty. Journal of Hand Surgery (Am.) 11(3): 324-332. Chaisson CE, Zhang Y, Sharma L, Kannel W, Felson DT (1999) Grip strength and the risk of developing radiographic hand osteoarthritis: results from the Framingham study Arthritis and Rheumatism 42(1):33-38 Creamer P, Hochberg MC (1997) Osteoarthritis. Lancet 350(9076):503-508. Creamer P, Flores R, Hochberg, MC (1998) Management of osteoarthritis in older adults. Clinics in Geriatric Medicine 14(3): 435-454. Day CS, Gelberman R, Patel AA, Vogt MT, Ditsios K, Boyer MI 2004) Basal joint osteoarthritis of the thumb: a prospective trial of steroid injection and splinting. The Journal of Hand Surgery 29A (2): 247-251. 10 Damen A, Withag KM, van der Lei B, den Dunnen WFA, Robinson PH (2001) Conservative treatment of CMC-1 osteoarthritis. European Journal of Plastic Surgery 24(1):33-37. Degreef I, De Smet L (2006) Predictors of outcome in surgical treatment for basal joint osteoarthritis of the thumb. Clinical Rheumatology 25(2):140-142. Dhar S, Gray IC, Jones WA, Beddow, FH (1994) Simple excision of trapezium for osteoarthritis of the carpometacarpal joint of thumb. Journal of Hand Surgery (Br.):19: 485-488. Dieppe P (2000) The management of osteoarthritis in the third millennium. Scandinavian Journal of Rheumatology 29(5): 279-281. Dominick KL, Jordan JM, Renner JB, Kraus VB (2005) Relationship of radiographic and clinical variables to pinch and grip strength among individuals with osteoarthritis. Arthritis and Rheumatism 52(5): 1424-1430. Eaton RG, Glickel SZ (1987) Trapeziometacarpal osteoarthritis: Staging a rationale for treatment. Hand Clinics 3(5): 455-471. Gervis WH (1949) Excision of the trapezium for osteoarthritis of the trapeziometacarpal joint. Journal of Bone and Joint Surgery 31B:537-539. Gervis WH (1973) A review of excision of the trapezium for osteoarthritis of the trapezio-metacarpal joint.after twenty-five years. Journal of Bone and Joint Surgery 55B: 56-57. Glyka M, Karen V, Achilleas T (2004) Surgical treatment of osteoarthritis of the carpometacarpal joint of the thumb: A Systemic Review. Plastic & Reconstructive Surgery 14(2); 421-432. 11 Hollevoet N, Kinnen L, Moermans JP, Ledoux P (1996) Excision of the trapezium for osteoarthritis of the trapeziometacarpal joint of the thumb. Journal of Hand Surgery 21B:458-462. Hudak PL, Amadio PC, Bombardier C (1996) Development of an upper extremity outcome measure: DASH (Disabilities of the Arm, Shoulder and Hand). The Upper Extremity Collaborative Group (UECG). American Journal of Industrial Medicine 29 (6): 602-608. Iyer KM (1981) The results of excision of the trapezium. Hand13: 117-120. Kvarnes L, Reikeras O (1985) Osteoarthritis of the carpometacarpal joint of the thumb. An analysis of operative procedures. Journal of Hand Surgery 10B: 117120. Kraus VB (1997) Pathogenesis and treatment of osteoarthritis. Medical Clinics of North America 81(1): 85-112. Kraus VB, Li YJ, Martin ER, Jordan JM, Renner JB, Doherty M, Wilson AG, Moskowitz R, Hochberg M, Loeser R, Hooper M, Sundseth S (2004) Articular hypermobility – no evidence of increased incidence of osteoarthritis in any hand joint. Arthritis and Rheumatism 50(7): 2178-2183. Mannoni, A, Briganti MP, Di Bari M, Ferruci L, Serni U, Masotti G (2000) Prevalence of symptomatic hand osteoarthritis in community dwelling older persons; the ICARe Dicomano study. Osteoarthritis & Cartilage 8(Suppl A):S1113. Martou G, Veltri K, Thoma A (2004) Surgical treatment of osteoarthritis of the carpometacarpal joint of the thumb: a systematic review. Plastic & Reconstructive Surgery 114(2):421-432. 12 Meenagh GK, Patton J, Kynes C, Wright GD (2004) A randomised controlled trial of intra-articular corticosteroid injection of the carpometacarpal joint of the thumb in osteoarthritis. Annuals of the Rheumatic Diseases 63(10):1260-1263. Murley AHG (1960) Excision of the trapezium in osteoarthritis of the first carpometacarpal joint. Journal of Bone and Joint Surgery 42B: 502-507. Necking LE, Eiken O (1986) ECRL-strip platy for metacarpal base fixation after excision of the trapezium. Scandinavian Journal of Plastic and Reconstructive Surgery 20:229-234. Pellegrini VD Jr (1992) Osteoarthritis at the base of the thumb. Orthopaedic Clinics of Norrth America 23 (11): 83-102. Roberts R, Jabaley M, Nick T (2001) Results following trapeziometacarpal arthroplasty of the thumb. Journal of Hand Therapy 14(2): 202-207. Schroder J, Kerkhoffs GMMJ, Voerman HJ (2002) Surgical treatment of basal joint disease of the thumb: a comparison between resection-interposition arthroplasty and trapezio-metacarpal arthrodesis. Archives of Orthopaedic & Trauma Surgery 122(1):35-38. Stamm, T.A., Machold, K.P. Smolen, J.S., Fischer, A., Redlich, K., Graninger, Ebner W, Erlacher L. (2002) Joint Protection and home hand exercises improve hand function in patients with hand osteoarthritis: a randomised controlled trial. Arthritis & Rheumatism 47(1):44-49. Turner A, Foster M, Johnson S (2004) Occupational Therapy and Physical Dysfunction, Principles, Skills and Practice (5th Ed.). Edinburgh: Churchill Livingstone. 13 Swigart CR, Eaton RG, Glickel SZ, Johnson C 1999) Splinting in treatment of arthritis of the first carpometacarpal joint. The Journal of Hand Surgery 24A (1):86-91. Szoeke CE, Cicuttini FM, Guthrie JR, Clark MS, Dennerstein L (2006) Factors affecting the prevalence of osteoarthritis in healthy middle-aged women: Data from the longitudinal Melbourne Women’s Midlife Health Project. Bone 39 (5): 1149-1155. Taylor EJ, Desari K, D’Arcy JC, Bonnici AV (2005) A comparison of fusion, trapeziectomy and silastic replacement for the treatment of osteoarthritis of the trapeziometacarpal joint. Journal of Hand Surgery 30B (1):45-49. Tortora G.J, Grabowski SR (2003) Principles of Anatomy & Physiology (10th Ed.). Chichester: John Wiley & Sons. Vandenbroucke J, Schriver De F, Smert L De, Fabry G (1997) Simple trapezectomy for treatment of trapeziometacarpal osteoarthritis of the thumb. Clinical Rheumatology 16:239-242. Von Schroeder HP (2003) Surgical Management of Osteoarthritis of the Hand and Wrist. Geriatrics and Aging 6(8): 16-19. Weiss S, LaStayo P, Mills A, Bramlet D (2000) Prospective analysis of splinting the first metacarpal joint; objective, subjective, and radiographic assessment. Journal of Hand Therapy 13(3): 218-26. Wilder FV, Barrett JP, Farina EF (2006) Joint specific prevalence of osteoarthritis of the hand. Osteoarthritis Cartilage 14(9):953-957. 14