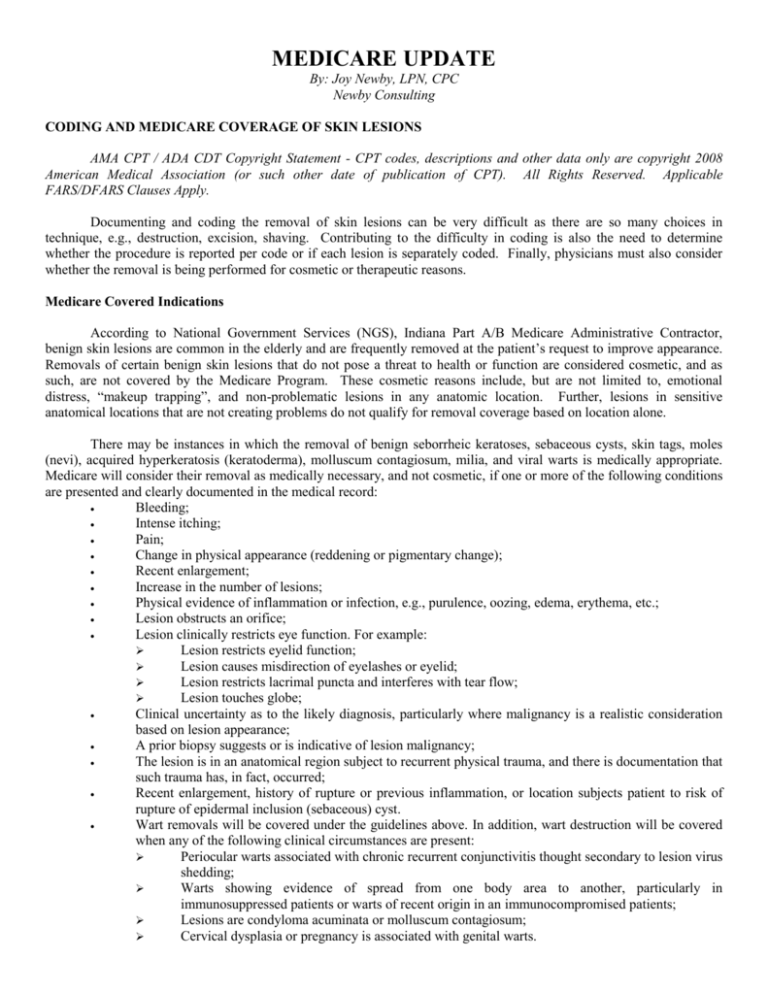
MEDICARE UPDATE
By: Joy Newby, LPN, CPC
Newby Consulting
CODING AND MEDICARE COVERAGE OF SKIN LESIONS
AMA CPT / ADA CDT Copyright Statement - CPT codes, descriptions and other data only are copyright 2008
American Medical Association (or such other date of publication of CPT). All Rights Reserved. Applicable
FARS/DFARS Clauses Apply.
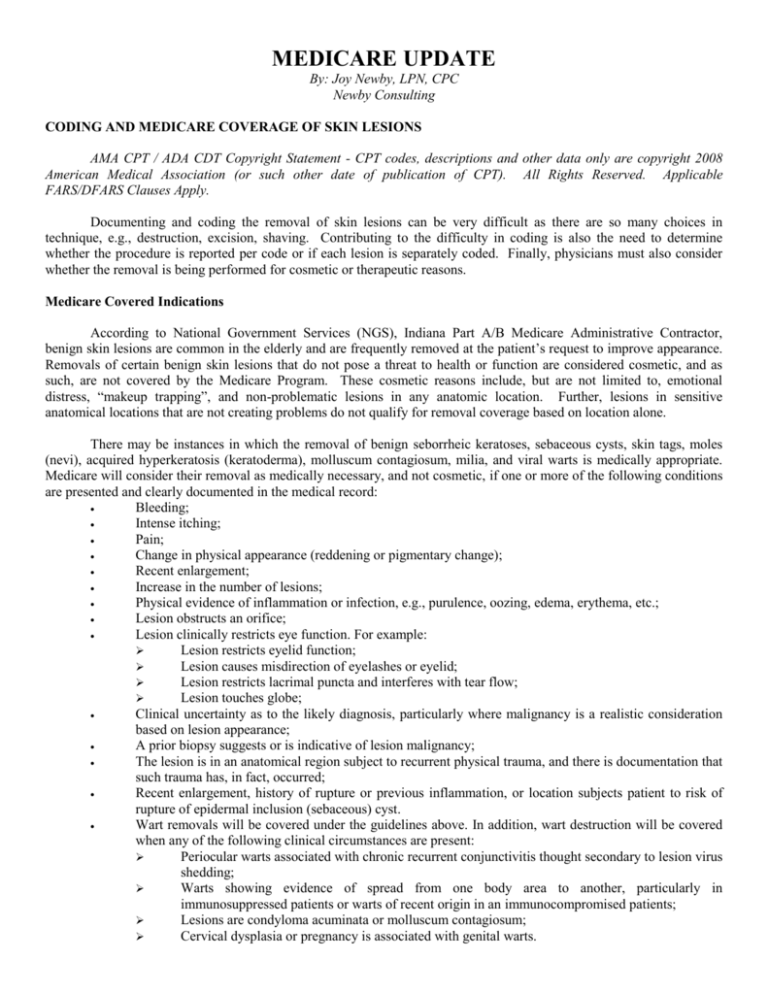
Documenting and coding the removal of skin lesions can be very difficult as there are so many choices in
technique, e.g., destruction, excision, shaving. Contributing to the difficulty in coding is also the need to determine
whether the procedure is reported per code or if each lesion is separately coded. Finally, physicians must also consider
whether the removal is being performed for cosmetic or therapeutic reasons.
Medicare Covered Indications
According to National Government Services (NGS), Indiana Part A/B Medicare Administrative Contractor,
benign skin lesions are common in the elderly and are frequently removed at the patient’s request to improve appearance.
Removals of certain benign skin lesions that do not pose a threat to health or function are considered cosmetic, and as
such, are not covered by the Medicare Program. These cosmetic reasons include, but are not limited to, emotional
distress, “makeup trapping”, and non-problematic lesions in any anatomic location. Further, lesions in sensitive
anatomical locations that are not creating problems do not qualify for removal coverage based on location alone.
There may be instances in which the removal of benign seborrheic keratoses, sebaceous cysts, skin tags, moles
(nevi), acquired hyperkeratosis (keratoderma), molluscum contagiosum, milia, and viral warts is medically appropriate.
Medicare will consider their removal as medically necessary, and not cosmetic, if one or more of the following conditions
are presented and clearly documented in the medical record:
Bleeding;
Intense itching;
Pain;
Change in physical appearance (reddening or pigmentary change);
Recent enlargement;
Increase in the number of lesions;
Physical evidence of inflammation or infection, e.g., purulence, oozing, edema, erythema, etc.;
Lesion obstructs an orifice;
Lesion clinically restricts eye function. For example:
Lesion restricts eyelid function;
Lesion causes misdirection of eyelashes or eyelid;
Lesion restricts lacrimal puncta and interferes with tear flow;
Lesion touches globe;
Clinical uncertainty as to the likely diagnosis, particularly where malignancy is a realistic consideration
based on lesion appearance;
A prior biopsy suggests or is indicative of lesion malignancy;
The lesion is in an anatomical region subject to recurrent physical trauma, and there is documentation that
such trauma has, in fact, occurred;
Recent enlargement, history of rupture or previous inflammation, or location subjects patient to risk of
rupture of epidermal inclusion (sebaceous) cyst.
Wart removals will be covered under the guidelines above. In addition, wart destruction will be covered
when any of the following clinical circumstances are present:
Periocular warts associated with chronic recurrent conjunctivitis thought secondary to lesion virus
shedding;
Warts showing evidence of spread from one body area to another, particularly in
immunosuppressed patients or warts of recent origin in an immunocompromised patients;
Lesions are condyloma acuminata or molluscum contagiosum;
Cervical dysplasia or pregnancy is associated with genital warts.
A statement of “irritated skin lesion” is insufficient justification for lesion removal when used solely to refer a
patient, describe a complaint, or the physician's physical findings. Similarly, use of an ICD-9 code 702.11 (inflamed
seborrheic keratosis) is insufficient to justify lesion removal, without the medical record documentation of the patient’s
symptoms and physical findings. Be sure to document the patient’s signs and symptoms as well as your physical findings.
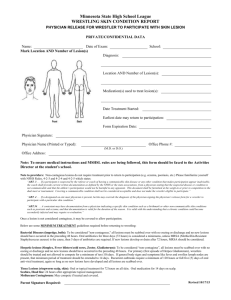
Drawings or diagrams to describe the precise anatomical location of the lesion are helpful. A procedural note,
protocol describing indications, diagnosis, methodology of treatment, or modality is required.
The type of removal is at the discretion of the treating physician and the appropriateness of the technique used
will not be a factor in deciding if a lesion merits removal. However, a benign lesion excision (CPT 11400-11446) must
have medical record documentation as to why an excisional removal, other than for cosmetic purposes, was the surgical
procedure of choice.
If the patient wishes one or more of these benign asymptomatic lesions removed for cosmetic purposes, the
patient is financially liable for the service rendered. The physician has the responsibility to notify the patient in advance
that Medicare will not cover cosmetic dermatological surgery and that the beneficiary will be liable for the cost of the
service. Although not required, NGS strongly advises executing a Medicare Advance Notice of Coverage (ABN) to show
the physician advised the patient that the procedure(s) is cosmetic and that the patient understands he/she is financially
responsible. NGS also recommends the ABN include the physician’s charge(s) for the procedure(s).
Physicians are not required to submit Medicare claims for removal of benign skin lesions performed for cosmetic
reasons unless the patient requests a formal Medicare denial. If a claim is filed, ICD-9 code V50.1 (other plastic surgery
for unacceptable cosmetic appearance) should be used in conjunction with the appropriate CPT code. The -GY modifier
should be appended to the appropriate CPT code(s) to indicate the procedure is statutorily excluded.
Skin Tags
Regardless of the technique, e.g., scissoring, ligature strangulation, electrosurgical destruction, chemical
destruction, with or without local anesthesia, physicians should report the following codes based on the number of skin
tags removed.
11200 Removal of skin tags, multiple fibrocutaneous tags, any area; up to and including 15 lesions
11201 each additional 10 lesions, or part thereof (List separately in addition to code for primary procedure)
Lesion Destruction
The AMA defines destruction as “the ablation of benign, premalignant, or malignant tissues by any method, with
or without curettement, including local anesthesia, and not usually requiring closure.” According to the AMA, the phrase
any method “includes electrosurgery, cryosurgery, laser and chemical treatment.”
Malignant Lesions
Coding for the destruction of malignant lesions is based on the location and size of the lesion. Each lesion is
separately reported. It may be necessary to use location modifiers, e.g., -RT, -LT, FA-F9, TA-T9, L1-L4 and/or the -59
modifier to indicate separate malignant lesions were removed.
Codes 17260-17266 are used to report the destruction of malignant lesion on the trunk, arms, or legs. Codes
17270-17276 are used to report the destruction of malignant lesion on the scalp, neck, hands, feet, or genitalia. Codes
17280-17286 are used to report the destruction of malignant lesion on the face, ears, eyelids, nose, lips, or mucous
membrane.
Premalignant Lesions
In CPT 2007, the AMA changed the descriptions of codes 17000, 17003, 17004, 17110, and 17111 to distinguish
between the destruction of benign and premalignant lesions.
Medicare covers the destruction of actinic keratoses without restrictions based on lesion or patient characteristics.
Please note destruction of these lesions should be reported using the following CPT codes
17000 Destruction (e.g., laser surgery, electrosurgery, cryosurgery, chemosurgery, surgical curettement),
premalignant lesions (e.g., actinic keratoses); first lesion
17003 Second through 14 lesions, each (List separately in addition to code for first lesion)
17004 Destruction (e.g., laser surgery, electrosurgery, cryosurgery, chemosurgery, surgical curettement),
premalignant lesions (e.g., actinic keratoses), 15 or more lesions
CPT code 17000 should be reported with one unit of service for destruction of the first lesion; CPT code 17003
should be reported with the units equal to the number of additional lesions from 2 through 14; and 17004 should be
reported with one unit of service, representing 15 or more lesions and should not be used with 17000 or 17003.
Benign Lesions
Unless one of the above indications are met and documented, Medicare considers destruction of benign lesions
cosmetic.
Destruction of benign lesions should be reported based on the number of lesions destroyed using the following
codes
17110 Destruction (e.g., laser surgery, electrosurgery, cryosurgery, chemosurgery, surgical curettement), of
benign lesions other than skin tags or cutaneous vascular proliferative lesions; up to 14 lesions
17111 15 or more lesions
CPT code 17110 should be reported with one unit of service for removal of benign lesions other than skin tags or
cutaneous vascular lesions, up to 14 lesions. CPT code 17111 is reported with one unit of service representing 15 or more
lesions. Do not use 17111 in conjunction with 17110.
Shaving of Epidermal or Dermal Lesions
According to the AMA, shaving is the “sharp removal by transverse incision or horizontal slicing to remove
epidermal and dermal lesions without a full-thickness dermal excision. This procedure includes local anesthesia and
chemical or electrocauterization of the wound. The wound does not require suture closure.” Each lesion is separately
reported based on size and location. It may be necessary to use location modifiers, e.g., -RT, -LT, FA-F9, TA-T9, L1-L4
and/or the -59 modifier to indicate separate lesions were removed.
Codes 11300-11303 are used to report the shaving of skin lesions on the trunk, arms, or legs. Codes 11305-11308
are used to report the shaving of skin lesions on the scalp, neck, hands, feet, and genitalia. Codes 11310-11313 are used
to report the shaving of skin lesions on the face, ears, eyelids, nose, lips, and mucous membrane
Excision of Benign Lesions
The AMA defines excision as a “full-thickness (through the dermis) removal of a lesion, including margins, and
includes simple (non-layered) closure when performed.” Coding excision of benign lesions is based on the location and
size of the lesion. Each lesion is separately reported. Size is determined by measuring the greatest clinical diameter of the
apparent lesion plus that margin required for complete excision (lesion diameter plus the most narrow margins required
equals the excised diameter). The margins refer to the narrowest margin required to adequately excise the lesion, based
on the physician's judgment. The measurement of lesion plus margin is made prior to excision.
It may be necessary to use location modifiers, e.g., -RT, -LT, FA-F9, TA-T9, L1-L4 and/or the -59 modifier to
indicate separate lesions were removed. These codes include simple repair. When the excision of benign lesions require
more than simple closure, e.g., requiring intermediate or complex closure, report 11400-11466 in addition to appropriate
intermediate (12031-12057) or complex closure (13100-13153) codes. For reconstructive closure, see 14000-14300,
15000-15261, and 15570-15770.
As previously stated, Medicare considers the removal of benign lesions cosmetic unless one or more of the above
indications are present and documented.
Excision of Malignant Lesions
As previously stated, the AMA defines excision as a “full-thickness (through the dermis) removal of a lesion,
including margins, and includes simple (non-layered) closure when performed.” Coding excision of malignant lesions is
based on the location and size of the lesion. Each lesion is separately reported. As with benign lesions, size is determined
by measuring the greatest clinical diameter of the apparent lesion plus that margin required for complete excision (lesion
diameter plus the most narrow margins required equals the excised diameter). The margins refer to the narrowest margin
required to adequately excise the lesion, based on the physician's judgment. The measurement of lesion plus margin is
made prior to excision.
It may be necessary to use location modifiers, e.g., -RT, -LT, FA-F9, TA-T9, L1-L4 and/or the -59 modifier to
indicate separate lesions were removed. These codes include simple repair When the excision of benign lesions require
more than simple closure, e.g., requiring intermediate or complex closure, report 11400-11466 in addition to appropriate
intermediate (12031-12057) or complex closure (13100-13153) codes. For reconstructive closure, see 14000-14300,
15000-15261, and 15570-15770.
Visits and Lesion Removal – To bill or Not to bill – That is the question!
Medicare will not pay for a separate E/M service on the same day as a lesion procedure unless a documented
significant and separately identifiable visit service is rendered. In addition, the procedure must be clearly documented in
the patient’s medical record and modifier -25 should be appended to the E/M code.
Clearly if the patient is seen for a different problem on the same day as the lesion procedure, both the visit (with
the -25 modifier) and the lesion procedure should be billed. For example, the patient presents for a follow-up of
hypertension and the physician also examines, diagnoses, and destroys two actinic keratitis lesions, both the visit and
surgical destruction procedure should be reported.
Typically for Medicare patients, the physician will only report the procedure when the patient presents for an
evaluation of the lesion and the physician diagnoses and destroys/excises a lesion. CMS does not normally allow
additional payments for an E/M services performed by a provider on the same day as a procedure. According to NGS,
E/M services provided on the same day as a lesion procedure, for the purpose of making the decision to perform the
procedure, are not separately payable. Modifier -57 cannot be used since the decision to perform the lesion removal is
considered a routine preoperative service and a visit or consultation should not be billed. Further, modifier -57 is only
applicable for major procedures that have a 90-day global period.
A visit on the same day as a procedure can only be reported when the physician performs an E/M service that is
significant, separately identifiable, and above and beyond the usual preoperative and postoperative care associated with
the procedure, Modifier -25 must be appended to the E/M code to allow additional payment for the separate service.
CMS provides the following clarification on reporting a visit on the same day as a minor procedure:
A visit on the same day could be properly billed in addition to suturing a scalp wound if a full neurological
examination is made for a patient with head trauma. Billing for a visit would not be appropriate if the physician
only identified the need for sutures and confirmed allergy and immunization status
Most lesion procedures include a ten (10) day postoperative period. Medicare will not pay for a separate E/M
service by the operating physician during the global period unless the service is for a medical problem unrelated to the
surgical procedure. The visit service must be documented in the patient’s medical record. In these situations, the
physician must add modifier -24 to the E/M code and the diagnosis for the unrelated diagnosis should be used in
conjunction with the CPT code.