Prof. Bryan Young BMC Neurology Dear Prof. Young: Thank you for
advertisement

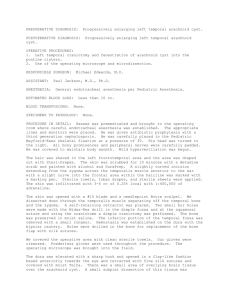
Prof. Bryan Young BMC Neurology Dear Prof. Young: Thank you for the opportunity to revise our manuscript entitled “The effectiveness of neuroendoscopic versus non-neuroendoscopic procedures in the treatment of lateral ventricular cysts: a retrospective medical record review study” for resubmission to BMC Neurology. We would also like to thank the reviewers for providing valuable comments. Our responses to those comments follow. Reviewer #1 Comment: It is unclear how patients were selected for either neuroendoscopy or open surgery. The abstracts indicate that patients were randomly assigned to the groups but there are no details of the randomization process. The authors should clarify how patients were assigned to the two operative groups. Response: The neurosurgeon initially used open surgery procedures and then gradually transitioned to endoscopic procedures. Therefore, the patients were not randomly assigned. The abstract has been revised to reflect the fact that there was no randomization. Comment: Although I believe the authors are only discussing intraventricular arachnoid cysts, throughout the paper, they refer to tumours. This results in confusion as to what the actual patient population. References to tumour throughout the paper should be replaced with the term cyst. Response: We agree and have changed “tumor” to “cyst” where appropriate. Comment: While the neuroendoscopic technique is described in detail, the technique for open surgery is less clear. More details regarding open surgery should be provided such as incision and craniotomy size. Response: We have added more details on the open surgery procedure. (see the third paragraph under the heading Surgical Method on pg 7) Comment: The authors refer to cysts being « almost » totally removed-clarify how degree of resection was objectively measured. Response: Determining the degree of cyst removal during the operations was based on the normal anatomy of the ventricle. When the walls of the lateral ventricle, choroid plexus and interventricular foramen were revealed as normal and CSF circulation was restored then the cyst wall can be considered to be completely removed. Comment: There remain scattered grammatical errors throughout the paper. Response: The paper has been reviewed again for grammar errors. Those found were corrected. Comment: It seems counter-intuitive that endoscopic management would yield a higher rate of cyst resection than open surgery. The authors should provide a proposed explanation for why this is so. Response: We have provided an explanation in the first paragraph of the Discussion section. We have argued that the endoscopic approach improves visualization in tight spaces, particularly within the lateral ventricle; increases the degree of freedom in creating corridors; etc. Comment: In the results section, the authors state that « most « fevers were non-infectious. Were any of the fevers caused by an infection. If not, « most » should be removed. They should also provide an explanation for the high fever rate in the endoscopy group. Response: Actually, all the fevers were non-infectious. We have revised the Results section to indicate this (see pg 9). As we have indicated in our manuscript we believe that fevers were most likely the result of intracerebroventricular rinsing during surgery. Comment: Did any patients have radiographic improvement without symptomatic improvement? Response: In the neuroendoscopy group, there was one case in which the symptoms were not relieved following cyst resection 6 months after the operation. This patient later received a ventricularperitoneal shunt operation. But for most patients, the neuroendoscopic approach not only removed the cyst but also restored the CSF circulation to the normal level. Reviewer #2 Comment: It is not clear whether this paper is primarily focused on the surgical treatment of arachnoid cysts. The authors may want to specify that they are indeed reporting their experience in treating this entity. A short description of arachnoid cyst would be a welcoming introduction to readers who are not familiar with this problem. Response: We have clarified the aim of this study in the abstract. The study is focused on the surgical treatment of arachnoid cysts. We have also provided a brief description of arachnoid cysts in the introduction and cited the following reference: Westermaier T, Schweitzer T, Ernestus RI. Arachnoid cysts. Adv Exp Med Biol 2012;724:37-50. Comment: Arachnoid cysts are more commonly found along the sylvian fissure (50%) and only 1% of them are located at the lateral ventricle. The majority of the patients do not need surgical treatment. Response: Because a cyst in the lateral ventricle occludes the CSF circulation route it produces high ICP. This situation requires surgical treatment. We have noted this requirement for surgery in the Introduction. (see pg 4) Comment: In this study the authors presented their experience and outcome in using endoscopic technique to resect these cysts at the lateral ventricles. They compared the outcomes of this approach to that of craniotomy and shunting. In this study there are 26% more patients with gross total resection in the endoscopic group than in the group treated with craniotomy; which may explain the difference in the higher recurrence rate in the craniotomy group (20.5%). Endoscopic approach definitely improves the visualization in tight spaces especially within the lateral ventricle. This may be one of many contributing factors in the difference in the outcome. However, its use in some cases are limited by the size of the ventricles. The authors may want to re-think their discussion and expand on the interpretation of their data. Response: We have added to the Discussion section the view of Gangemi et al [25] that endoscopic cyst fenestration from the lateral ventricle or third ventricle according to the extension of the cyst is a relatively easy procedure and safe procedure which does not risk damaging the deep incisural and quadrigeminal veins. (see pg 11) The reviewer noted that the use of the endoscopic approach in some cases is limited by the size of the ventricles but we found in our cases of lesions in the lateral ventricle that the ventricle had been stretched. Comment: The authors may want to offer an explanation why endoscopic approach allows more thorough resection of the cyst; such as improved field of view, the degree of freedom in creating surgical corridors etc. Response: As noted in a response above, the characteristics of the endoscope are helpful for completely exposing the cyst and subsequent total removal of the masses. Comment: The subdural and fever may be explained by the presence of “chemical aseptic” meningitis and decompressing the cyst into the subdural space, thus creates a transient "cystic subdural fistula/shunt" hence less chance of recurrence. The merit of this study is its avocation in using endoscopic technique and demonstrates it is more superior than open craniotomy ( a 64 vs 5.1 difference in marked improvement between the two groups. Response: Yes, we wanted to share our experience of using neuroendoscopy for treating arachnoid cysts which demonstrated advantages over open craniotomy.