Skin to Skin Care in the ISCC
advertisement

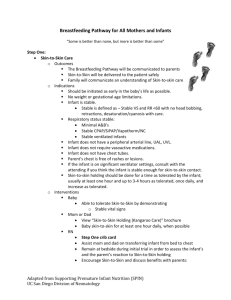
POLICY/PROCEDURE TITLE: Skin to Skin Care in the ISCC (S2S) Women & Infant Services RELATED TO: [ ] ADMINISTRATIVE [ X] CLINICAL Revision date: 3/1/08 [ ] Medical Center Policy (MCP) [X] Nursing Practice Stds. Effective date: 3/1/08 [ ] JCAHO [X] Patient Care Stds. Unit/Department of Origin: ISCC [ ] QA [ ] Other Other Approval: PAGE 1 OF 2_ [ ] Title 22 POLICY STATEMENT: The many benefits of skin-to-skin care are well documented in the medical and nursing literature including but not limited to: state regulation, temperature stabilization, heart rate and breathing regularity in the infant, maternal infant bonding and increased milk production in the mother. The benefits to skin-to-skin care encourage its use as soon as infants are stable even if they are intubated and have lines in place. The times when infants would not be considered stable for skin-to-skin care would include but are not limited to: infants that are not hemodynamically stable, infants requiring humidity, pre or post operative infants with unmanageable pain. These patients should be reassessed frequently for change in status making them able to participate in skin-to-skin care. RNs will facilitate daily skin-to-skin care for all infants as long a time period as the parent can provide and infant tolerates. The medical team will write an order hold skin-to-skin care during periods of physiologic instability. All infants that have their skin-to-skin care held for instability will have their status reviewed each shift to resume skin-to-skin care as soon as possible. RESPONSIBLE PARTY: ISCC RNs, MDs, NNPs, RTs, OTs, LCs and families of infants in the ISCC. EQUIPMENT: Mother (or Father) Chair and foot stool Privacy screen Pillow(s) Tape or Velcro clips for securing lines/tubing Blankets Hat for infant’s head ***Optional: Mirror for Mother or Father to see baby SPECIAL CONSIDERATIONS: If patient is intubated two healthcare professionals are required for transfer of infant, one of which being an RN and the other being a second RN, MD, or RT. The second professional should be focused on stabilizing the ETT and airway while mother picks up infant and RN stabilizes lines. Both professionals and parent monitor patient tolerance. UCSD Medical Center page 2 PROCEDURE: Educate parents o Benefits o Encourage wearing a tank top or a shirt that opens in front. o Suggested length of time and frequency of sessions o How to transfer baby o Reading infant signals, issue booklet, “Understanding My Baby’s Signals” if family does not already have one. o What to watch for while holding skin-to-skin Gather equipment: chair for mother, privacy screen, tape, blankets, hat, mirror Encourage mother to go to the bathroom and get a drink before transfer because she may be holding her infant for a long period of time. Record baby’s vital signs Place chair as close to bedside as possible. For mom’s comfort offer privacy screen and place it around chair and bedside Have mother remove bra, unbutton shirt and stand as close to bed as possible. Have mother unwrap infant and remove infant’s t-shirt or clothes. Support mother in picking up infant and placing him/her skin-to-skin on her chest being mindful of all tubing, leads and lines. Reinforce education of reading infant cues and tolerance. Place blanket over infant or pull up tank top over infant and then place blanket over them both. Hold chair stable and guide mother to sit in chair, monitor tubing, leads and lines. Secure tubing, leads and lines with tape or Velcro clips to chair or mom to prevent dislodging. Place pillows and foot stool to mother’s comfort. Document education give to mother (and family), transfer of infant and tolerance. At the end of session encourage and assist mother to stand and reverse the transfer process with mother returning the infant to the bed, changing diaper and positioning to the infant’s comfort. Document the length of time of infant skin-to-skin and tolerance. REFERENCES: DiMenna, L. (2006). Considerations for implementation of a neonatal kangaroo care protocol. Neonatal Network, 25: 6, (p. 405-412). Smith, K.M. (2007). Sleep and kangaroo care: Clinical practice in the newborn intensive care unit. Journal of Perinatal Neonatal Nursing. Vol. 21 No. 2 (p. 151-157). Merenstein, G. B. & Gardner, S. L. (2006). Handbook of neonatal intensive care. Sixth Edition (p. 296-303).