clinical evaluation of eye movements
advertisement

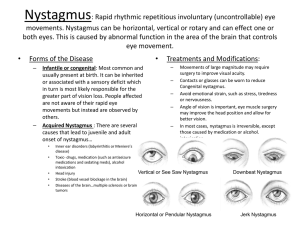
Neurologic exam CLINICAL EVALUATION OF EYE MOVEMENTS Dr. Bruce Giffin Wednesday, April 18, 2007 10:00 AM LEARNING OBJECTIVES: The student should be able to examine and evaluate eye movements recognize abnormal eye movements and patterns of abnormality that anatomically localize the lesion responsible for abnormal eye movements Abnormalities of eye movement can result from (1) disease of one of the six muscles that move the eye (2) disease of the neuromuscular junction (3) a lesion of the cranial nerves (nucleus or nerve fibers) that supply the extraocular muscles (All of the above are referred to as “nuclear” or “infranuclear palsy”) (4) a dysfunction of the highly specialized neural mechanisms that enable the eyes to move together (referred to as “supranuclear palsy”; “internuclear ophthalmoplegia”) (5) anything affecting the mechanical properties of the eyeballs themselves (e.g., a soft tissue mass in the orbit restricting the movement of the eyeball) Eye movement testing includes examination for: DUCTIONS o the extent of eye movement when each eye is tested individually VERSIONS o the extent of eye movements when both eyes are tested together o the long axes of the eyes remain parallel to each other SACCADIC EYE MOVEMENTS o the rapid movement from one point of fixation to another o tested with alternate commands to gaze at two targets (e.g., pen and finger) PURSUIT EYE MOVEMENTS o the slow eye movement used to maintain fixation on a moving object o tested by having the patient follow a small slowly and smoothly moving object to ensure foveation VESTIBULAR-POSITIONAL EYE MOVEMENTS o vestibular-ocular reflex o eye movements that compensate for movement of the head to maintain fixation of an object on the fovea VERGENCES o the ability of the eyes to work together and converge or diverge on a target o the long axes of the eyes do not remain parallel to each other o tested by having the patient look at a target and follow it towards their nose and then away from their nose GLOSSARY DIPLOPIA: double vision ESOTROPIA: a deviation of one eye toward the other; also known as internal strabismus, or crosseye EXTORSION: rotary movement of the eye in a lateral direction INTORSION: rotary movement of the eye in a medial direction EXOTROPIA: a deviation of the visual axis of one eye away from the other; also know as external strabisumus, or walleye STRABISMUS: a deviation of the eye that the patient cannot overcome A downward deviation of the eye is HYPOTROPIA; an upward deviation is HYPERTROPIA A REVIEW OF THE EXTRAOCULAR MUSCLES The names, positions and actions of the extraocular muscles are illustrated below. The main points to keep in mind are: (1) The medial rectus muscle of one eye and the lateral rectus muscle of the other work as a yoked pair to produce lateral eye movements. (The central mechanisms responsible for synchronizing these actions will be reviewed by Dr. Brown.) (2) The vertically acting superior and inferior rectus muscles are most effective when the eye is abducted (looking outwards) because, in this position, the line of pull of the muscles is along the vertical axis of the eye (3) The superior and inferior oblique muscles are maximally effective when the eye is adducted (looking inwards) because, in this position, their line of pull is along the vertical axis of the eye From a neurological standpoint, these are the most important points to remember. While it is true that all the muscles have secondary actions and torsional effects on the eyeball, worrying too much about these details often confuses the simple facts that you should know in order to perform an adequate examination of eyeball movements. RELATIVE ORIENTATIONS OF THE EYES IN THE ORBITS: when focused for far vision, the eye points straight ahead so that images land on the fovea (f). Because the lateral wall of each orbit is oriented 45 degrees from the sagittal plane, the axis of the orbit, along which the inferior and superior recti pull, is oriented about 23 degrees from the visual axis. TERMINOLOGY FOR EYE MOVEMENTS AROUND DIFFERENT AXES: different patterns of contraction of the six extraocular muscles rotate the eyes horizontally o adduction o abduction vertically o elevation o depression TORSION OF THE EYES RESULTS FROM MOVEMENT AROUND THE ANTERIOR-POSTERIOR AXIS OF THE EYE. In the figure above, the right eye is undergoing intorsion; the left, extorsion. The torsions are named in- or ex-, depending on whether the top of the vertical axis tilts in (medially) or out (laterally). ACTIONS OF THE MEDIAL AND LATERAL RECTUS MUSCLES OF THE RIGHT EYE: adduction and abduction are the only significant effects of the medial and lateral recti. ACTIONS OF THE RIGHT SUPERIOR AND INFERIOR RECTI AND OBLIQUES. Each has a primary action (large arrow) and two secondary actions (small arrows) when starting in primary position. The actions are determined by the direction of insertion of a muscle’s tendon and by the position of the insertion. For example, the superior rectus and superior oblique both insert on the superior surface of the globe. However, the superior rectus inserts anteriorly and pulls posteriorly, so it elevates the eye. In contrast, the superior oblique inserts posteriorly and pulls anteriorly so that part of its action is depression of the globe. CLINICAL MANIFESTATIONS OF EXTRAOCULAR NERVE LESIONS Diplopia is the single symptom that most often indicates damage to one of the cranial nerves that controls the movement of the eyeball (oculomotor –CN III; trochlear- CN IV; abducensCN VI). Under normal circumstances the eyes are positioned such that the image falls exactly on the same spot on the retina of each eye. The slightest displacement of either eye causes diplopia (double vision) because the image is shifted to a different position on the retina of the displaced eye. Usually the weak muscle (or muscles) resulting from nerve lesions can be detected by direct observation of eye movements. Before considering 3rd, 4th and 6th nerve palsies in detail, review how to test the individual action of each of the eye muscles. The diagram below shows the right eye viewed from the front. TESTING THE INDIVIDUAL EYE MUSCLES. Test each eye by using your finger or a pen and have the patient first follow it toward the nose, then up and down; now move out (laterally) and then up and down. What’s happening? When the eye is abducted, the superior rectus is now in an ideal position to elevate the eye and the inferior rectus is the main depressor of the eye. The actions of the medial and lateral rectus muscles are intuitively obvious. When the eye is adducted, the inferior oblique is the main elevator of the eye (due to its insertion in the lower back of the eyeball) and the superior oblique is the main depressor of the eye (due to its insertion which pulls the eyeball up and over from behind) THIRD NERVE PALSY Ptosis of the upper eyelid o a complete 3rd nerve lesion causes total paralysis of the eyelid o inactivation of the levator palpebrae superioris muscle and subsequent unopposed action of the orbicularis oculi o compensation for the ptosis by contracting the frontalis muscle to raise the eyelid on the affected side The affected eye is deviated laterally (exotropia; lateral strabismus) and downward (hypotropia) o the resulting diplopia (double vision) only occurs when the lid is held up o severe diplopia occurs in all directions of gaze, except on lateral gaze to the side of the third nerve lesion Pupillary dilation due to decreased tone of the constrictor pupillae muscle o preganglionic parasympathetic fibers from the Edinger-Westphal nucleus travel in the 3rd nerve Paralysis of accommodation This diagram shows a complete left 3rd nerve palsy. The lesion can be incomplete of course, in terms of ptosis, pupil dilation, or weakness of eye movements. Oculomotor ophthalmoplegia is the clinical term used to describe the collection of neurologic signs described above. Possible causes of lesions of the 3rd nerve include: Aneurysms of the posterior cerebral or superior cerebellar arteries between which the oculomotor nerve emerges from the brainstem Tentorial herniation of the temporal lobe can displace the cerebral peduncle to the opposite side and stretch the oculomotor nerve The 3rd nerve travels in the wall of the cavernous sinus and is vulnerable to lesions in this area Syphilitic and tuberculous meningitis tend to localize between the chiasma, pons and temporal lobes where the 3rd nerve emerges from the brainstem and can therefore affect it FOURTH NERVE PALSY Results in weakness of the superior oblique muscle, producing a subtle diplopia and weakness in downward gaze Extorsion (outward rotation of the eye) is present in the affected eye, and is attributable to the unopposed action of the inferior oblique muscle Paralysis or weakness of the superior oblique muscle is tested by having the patient look “in and down” Patients will tilt the head to compensate for the paralyzed superior oblique muscle. Under normal conditions when the head tilts, the eyes rotate in the opposite direction around the anteroposterior axis to maintain a vertical image on the retina. Patients with 4th nerve palsies often tilt their head to the unaffected side, thereby causing the normal eye to intort and line up with the extorted, affected eye. Possible causes of lesions to the 4th nerve include: Compression resulting from aneurysms of the posterior cerebral and superior cerebellar arteries Pathologic lesions of the cavernous sinus or superior orbital fissure Damage during surgical procedures because of its long intracranial course and its position, just inferior to the free edge of the tentorium cerebelli SIXTH NERVE PALSY Deficit in abduction due to paralysis of the lateral rectus muscle Internal strabismus (esotropia) due to unopposed action of the medial rectus muscle Causes the greatest problem for the patient since there is no ptosis to obliterate the diplopia which persists in nearly all directions of gaze except away from the affected side Patients may shut the affected eye to prevent diplopia; can be misinterpreted as ptosis Test by having the patient “look to the left (or right)”. Possible causes of lesions to the 6th nerve include: Aneurysms of PICA or basilar arteries; occlusion of paramedian branches of basilar artery A cerebellar tumor growing into the 4th ventricle may compress the abducens nucleus The 6th nerve is vulnerable to fractures of the base of the skull because of its close association with the floor of the posterior cranial fossa Increased intracranial pressure can compress the 6th nerve as it crosses the ridge of the petrous temporal bone Lesions in the cavernous sinus can damage the 6th nerve which lies lateral to the internal carotid artery CLINICAL TESTS & SIGNS: VOLUNTARY HORIZONTAL SACCADES Clinical Test: Ask patient to look at object (pencil, your finger) in extreme left and right areas of his/her visual fields. Look for simultaneous conjugate eye movement in the appropriate direction. Clinical Signs of Supranuclear Lesions of voluntary horizontal saccades (clinical term = horizontal gaze palsy): Specific features vary with location of lesion along the path. The most common locations: [SEE DIAGRAM ON THE NEXT PAGE] -- in cortex - frontal eye field or FEF (Lesion “A” below). If acute, as in stroke, signs often include: early responses (minutes to hours after insult): -- patient “looks to side of lesion” at rest (loss of tonic outflow from the injured FEF releases tone of opposite, functional FEF) -- patient cannot look to side opposite the lesion (“paralysis” of lateral gaze) after hours to days: -- acute gaze symptoms usually disappear (compensatory circuitry through superior colliculus) -- in pons – PPRF (Lesion B): causes paralysis of lateral gaze toward side ipsilateral to lesion Clinical Signs of Internuclear Lesions of horizontal gaze path: -- in MLF (Lesion C; clinical term = internuclear ophthalmoplegia or INO) : loss of adduction (medial rectus contraction) during horizontal gaze to opposite side. TAKE HOME MESSAGE: Most horizontal gaze palsies are due to lesions in the cortex, pons, or MLF. Cortical horizontal gaze palsies are usually transient; pontine & MLF signs are often enduring. EXAMPLE: LESIONS IN PATH FOR VOLUNTARY HORIZONTAL GAZE TO RIGHT LESIONS A & B (supranuclear) PARALYSIS OF RIGHT HORIZONTAL GAZE LESION C (INO) PARALYSIS OF ADDUCTION DURING RIGHT HORIZONTAL GAZE NOTE: A lesion of the MLF (INO) will interrupt fibers from both: - opposite PPRF (via abducens interneurons), causing a paralysis of adduction - vestibular nuclei, sometimes causing a nystagmus of the abducting eye BELOW: DIAGRAM SHOWING BASIS FOR PARALYSIS OF ADDUCTION AND RIGHT NYSTAGMUS DURING RIGHT LATERAL GAZE VOLUNTARY VERTICAL GAZE: CLINICAL TESTS AND SIGNS OF DYSFUNCTION Clinical Test for Voluntary Vertical Saccades: Ask patient to look at an object (pencil, your finger) in upper and lower areas of his/her visual fields. Look for synchronized movements of both eyes that are equal in magnitude and duration. Clinical Signs of Supranuclear Lesions in Voluntary Vertical Saccade Path (called vertical gaze palsy): defects in initiating voluntary upgaze and/or downgaze Most common location of lesions that cause a clinically-detectable vertical gaze palsy: rostral midbrain (especially tectum & periaqueductal area); pineal body, causing dysfunction of upgaze or downgaze premotor centers. CLINICAL TESTS & SIGNS FOR TRACKING (SMOOTH PURSUIT): Clinical Test: Ask patient to visually follow object that is moved slowly in different directions. Clinical Sign of Supranuclear Dysfunction: Inability to initiate smooth pursuit of an object fixed on the foveas. This is most commonly caused by a lesion of the parietal (posterior) eye field, which results in loss of pursuit of objects moving to the same side as the lesion. Example: lesion of left parietal eye field loss of pursuit to the left. Clinical signs may be transient. CLINICAL TESTS & SIGNS FOR CONVERGENCE Clinical Test: Ask patient to keep focused on an object (examiner’s finger, pen) that is brought from feet away (in midline) to inches away (in midline). Clinical Signs: Inability to initiate eyeball convergence. CLINICAL TESTS & SIGNS FOR VESTIBULO-OCULAR REFLEXES (VOR) Clinical test for maintaining stable eyeball position during head movement: Ask patient to look at a specific object in space for the entire test. Rotate the patient’s head & look for compensatory eyeball adjustments (e.g., eyes continue to look at same object in space). NOTE: In an unconscious person, stability of eyeball position during head movement is called “doll’s eyes” (dolls with weighted eyeballs keep a stable eyeball position). Doll’s eyes indicate functional VORs in the patient. Clinical signs of supranuclear dysfunction in the VOR during head movement: inability of eyes to maintain fixation on desired object during head movement. ABNORMAL NYSTAGMUS Abnormal nystagmus (oscillation of eyeballs) includes: - spontaneous nystagmus (eye oscillations that occur in the absence of patterns of stimulation that induce normal nystagmus) - absent or abnormal nystagmus following vestibular stimulation that normally induces nystagmus Abnormal nystagmus: - is usually caused by dysfunction of vestibular and/or cerebellar paths Spontaneous (abnormal) nystagmus can occur: - continuously, even when eyes are ”at rest” - in response to initiation of an eye movement (e.g., nystagmus on lateral gaze to right) CLINICAL TESTS FOR VESTIBULAR NYSTAGMUS Clinical tests for vestibular nystagmus (VOR + corrective saccades): 1) Thermal Stimulation (Caloric Test): Inject warm or cold fluid into the external ear to change temperature of fluid in the inner ear. This thermally-stimulates vestibular receptors of one side only, causing an unbalanced input into the left & right vestibular nuclei. Normally, a nystagmus results, having a direction that varies for cold versus warm water stimulation. Nomenclature for direction of eye movements during caloric test: Normal response to introduction of cold water in one auditory canal: -- nystagmus with fast component to side opposite the one injected with water Normal response to introduction of warm water in one auditory canal: -- nystagmus with fast component to same side as one injected with water Mnemonic: C O W S (cold-opposite-warm-same) 2) Visual examination for abnormal nystagmus during non-testing situations (when eyes are “at rest”) and during eye movement tests. CLINICAL TESTS & SIGNS FOR VISUAL (OPTOKINETIC) NYSTAGMUS (OKN) Clinical test for optokinetic nystagmus: Place a drum with repeating stripes in front of the patient and rotate it. With the head fixed, the patient’s eyes will normally follow a single stripe to the limit of vision, then saccade back to a new stripe, etc. NOTE: The test for OKN is useful in examining for malingering. Because the OKN is involuntary (does not involve the frontal eye fields), individuals with adequate vision to see the stripes (and a normal VOR path) will exhibit optokinetic nystagmus. This proves that they can see.