Applications of CT scan and MRI in
advertisement
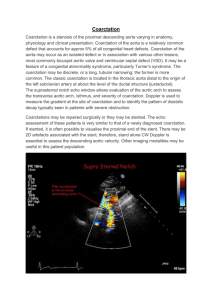
Applications of CT scan and MRI in Aortic and Peripheral vascular diseases Advances in cross-sectional imaging have revolutionized our ability to image the thoracic aorta. Historically, aortic imaging was performed with contrast angiography, which is clearly effective in the evaluation of aortic and Peripheral vascular diseases. However, because of its invasive nature, catheter angiography is not without complications, including arrhythmia, stroke, and hemorrhage. Now, with increasingly effective ultrasound (Doppler), CT and MRI, these techniques have largely replaced conventional angiography in the evaluation of aortic and peripheral vascular diseases. Ultrasound (US) is a safe, non-invasive, diagnostic tool with widespread applications in health care. Color Doppler has become the first imaging modality for suspected peripheral vascular diseases. The transesophageal echocardiogram is a relatively good test in the diagnosis of aortic disease. The main disadvantage of sonography is its inability to penetrate bone.Disadvantages of the TEE include the inability to visualize the distal ascending and the descending aorta. Sonography is completely dependent on the skill of the operator. The other non-invasive imaging techniques include computed tomography angiography (CTA) and magnetic resonance angiography (MRA). The main Advantages of CTA : rapid scanning, high special resolution imaging ,ability to visualize calcium The main disadvantage of CTA: ionizing radiation and nephrotoxic contrast The main Advantages of MRA: Even without using contrast material, MR angiography can provide high-quality images of vessels and non ionizing radiation The main disadvantages of MRA: longer scan times when CT, can not be used in patients with pacemakers, low special resolution and Claustrophobia CTA technique: test blues or blues tracking MRA techniques: Time-of-Flight( ToF) , Phase-contrast MR image and MRA with contrast Artifacts: motion artifact Indications: 1/ Congenital anomalies 2/ Aortic aneurysm 3/Aortic dissection 4/ Infection 5/ Traumatic aortic injury 6/ Atherosclerotic disease Aortic Arch Anomalies The standard branching pattern of the thoracic aorta is seen in only 75% of patients. The most common aortic variant is the so-called bovine arch, in which the right brachiocephalic artery and left common carotid artery have a common origin. The left aortic arch with an aberrant right subclavian artery is the most common aortic arch anomaly. In most cases, the aberrant right subclavian artery crosses posterior to the esophagus. Right aortic arch with mirror-image branching is commonly associated with congenital heart disease and is seen most often in patients with tetralogy of Fallot, ventricular septal defects, and truncus arteriosus. Coarctation of the Aorta Aortic Aneurysm A true thoracic aortic aneurysm involves all components of the vessel wall. Thoracic aortic aneurysms are most commonly located within the descending aorta at the level of the ligamentum arteriosum, just distal to the origin of the subclavian artery. CT can demonstrate the following characteristics of the aneurysm: Dilation of the aorta, calcification, intraluminal thrombi, displacement or erosion of adjacent structures and perianeurysmal thickening and hemorrhage. Identification of mural thrombus and calcification is common, because most aortic aneurysms are secondary to arteriosclerosis. Thoracic Aortic Dissection Dissection occurs from a tear in the wall of the aorta, with subsequent hemorrhage of blood into the media, creating a second or false lumen. CT has proved to be highly reliable for diagnosing or excluding aortic dissection. CT angiography can demonstrate the dissection flap more clearly than conventional CT can. MRI generally provides a definitive diagnosis of aortic dissection by demonstrating the two lumens and the intimal flap between them, similar to the criteria for CT. Thoracic Aortic Trauma 90% of thoracic aortic injuries occur within the proximal descending aorta Aottitis