1: Z Kinderchir
advertisement
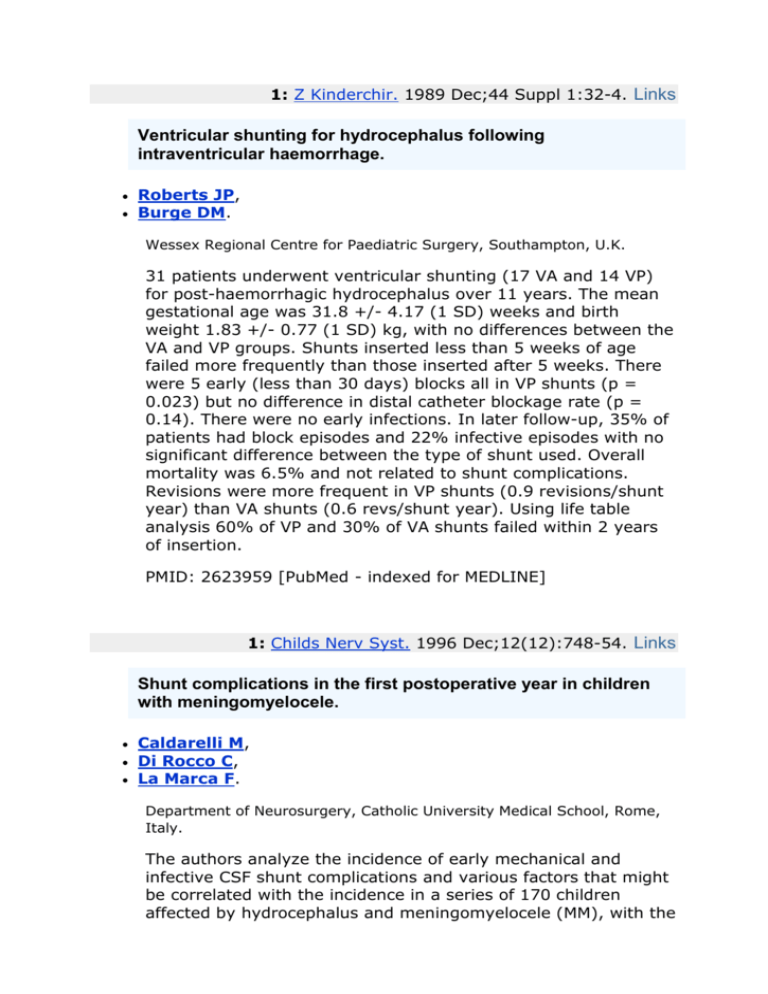
1: Z Kinderchir. 1989 Dec;44 Suppl 1:32-4. Links Ventricular shunting for hydrocephalus following intraventricular haemorrhage. Roberts JP, Burge DM. Wessex Regional Centre for Paediatric Surgery, Southampton, U.K. 31 patients underwent ventricular shunting (17 VA and 14 VP) for post-haemorrhagic hydrocephalus over 11 years. The mean gestational age was 31.8 +/- 4.17 (1 SD) weeks and birth weight 1.83 +/- 0.77 (1 SD) kg, with no differences between the VA and VP groups. Shunts inserted less than 5 weeks of age failed more frequently than those inserted after 5 weeks. There were 5 early (less than 30 days) blocks all in VP shunts (p = 0.023) but no difference in distal catheter blockage rate (p = 0.14). There were no early infections. In later follow-up, 35% of patients had block episodes and 22% infective episodes with no significant difference between the type of shunt used. Overall mortality was 6.5% and not related to shunt complications. Revisions were more frequent in VP shunts (0.9 revisions/shunt year) than VA shunts (0.6 revs/shunt year). Using life table analysis 60% of VP and 30% of VA shunts failed within 2 years of insertion. PMID: 2623959 [PubMed - indexed for MEDLINE] 1: Childs Nerv Syst. 1996 Dec;12(12):748-54. Links Shunt complications in the first postoperative year in children with meningomyelocele. Caldarelli M, Di Rocco C, La Marca F. Department of Neurosurgery, Catholic University Medical School, Rome, Italy. The authors analyze the incidence of early mechanical and infective CSF shunt complications and various factors that might be correlated with the incidence in a series of 170 children affected by hydrocephalus and meningomyelocele (MM), with the aim of the finding to this specific risk factors related to this particular type of hydrocephalus. Factors investigated for correlation with CSF shunt malfunction are the following: level of spinal malformation, age of the patient at MM repair, age at diagnosis of hydrocephalus, degree of ventricular dilatation, age at shunt implantation, modality of the surgical procedure, characteristics of CSF at operation. In the first postoperative year following CSF shunting, 45.9% of the patients presented one shunt malfunction, three-quarters of which were due to mechanical causes, and one quarter to infection. Age of the patient at diagnosis of hydrocephalus and at CSF shunt operation did not significantly influence shunt patency, nor did the surgical modality (programmed vs emergency procedure). On the other hand, MM level did influence the outcome of CSF shunting: a higher percentage of malfunctions (and in particular of infective complications) was observed among the patients with "high level" MMs than in the group with more caudal location of the spinal defect. Similarly, the degree of ventricular dilatation correlated with the incidence of complications (more severe ventricular dilatation was associated with the highest incidence of complications). The order in which MM repair and CSF shunting were carried out and the age of the patients at MM repair did not affect the occurrence of mechanical complications, whereas they had a significant effect on the incidence of infective complications. In fact, the rate of overall complications, and of infective complications in particular, was proportional the age at MM repair. Furthermore, the group of children who underwent to MM repair and CSF shunting simultaneously scored the lowest percentage of complications, although these were mainly infections; the highest incidence of complications (and in particular of infective ones) was observed in the children who underwent CSF shunting first. The most striking correlation, however, was found with the characteristics of CSF. While normal CSF values correlated with an overall incidence of complications of 39.2%, abnormal CSF values were correlated with a rate of complications of 90.9%; in particular, the rates of infective complications were 2.7% and 77.3%, respectively. On the grounds of these observations a protocol is proposed of temporary CSF external drainage in children requiring prompt relief of increased intracranial pressure but at risk for the presence of a leaking spinal defect or of a MM left unrepaired for more than 48 h. PMID: 9118142 [PubMed - indexed for MEDLINE] Acta Neurochir (Wien). 1995;136(3-4):189-94. Links Frequency and causes of shunt revisions in different cerebrospinal fluid shunt types. Borgbjerg BM, Gjerris F, Albeck MJ, Hauerberg J, Borgesen SE. University Clinic of Neurosurgery, Rigshospitalet, Copenhagen, Denmark. Shunt complications and revisions are common in hydrocephalic patients treated with a ventriculo-atrial or a ventriculo-peritoneal shunt. The reported revision rate differs very much but the rate of revision is close to 50% in many papers. Data from 884 hydrocephalic patients treated with various shunt types in the period 1958-1989 were recorded retrospectively in order to evaluate the frequency of revision for various shunt types and secondly to analyse the specific reasons for the shunt revisions. The rate of shunt revision was 45%. The Pudenz shunt was revised more often (62%) than the remaining shunt types. The Hakim and the Orbis-Sigma shunts had fewer revisions (35% and 27%, respectively) than the other observed shunt types. A defect of or an obstruction in the ventricular catheters was a frequent cause of revision followed by a defect or an obstruction of the distal catheter, a displacement of the distal catheter and an acute infection. Because of the higher rate of revision for the Pudenz shunt the rate of the above mentioned specific complications is also higher in most of the subgroups for that specific shunt type. Driven by these experiences it is reasonable to seek to develop and introduce new shunt types in an attempt to reduce the complication rate. PMID: 8748853 [PubMed - indexed for MEDLINE] ORIGINAL ARTICLE Year : 2005 | Volume : 72 | Issue : 10 | Page : 843-847 Shunt revision in hydrocephalus Kumar Raj1, Singh Vinita2, Kumar Marakani V. K.3 1 Department of NeurosurgerySanjay Gandhi Postgraduate Institute of Medical SciencesLucknow, India 2 Neuroanaesthesiology King George's Medical University, Lucknow, India 3 Department of Neurosurgery Sanjay Gandhi Postgraduate Institute of Medical Sciences Lucknow, India Correspondence Address: Kumar Raj Associate Professor, Department of Neurosurgery, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Lucknow-226014, UP India rajkumar@sgpgi.ac.in » Abstract Objective : A retrospective analysis of 50 hydrocephalic children having a minimum followup of 6 months was carried out to see their etiology, clinical features, complications, incidence of shunt revisions, outcome and the variation from their Western counterparts. Methods : Clinical features, image findings and treatment of all the cases were recorded from their discharge summaries. Record of shunt revision complications and outcome was maintained by the principal author. The data of all the cases were analyzed. Results : The age of children varied from 1 month to 12 yr (mean 2.2 yr). The most common etiology of hydrocephalus was aqueductal stenosis in 18 (36%) children. Post infective hydrocephalus, either of post-tubercular meningitis (TBM) or following bacterial meningitis, remained the cause in 15 children (30%). Congenital TORCH infection was responsible for 3 cases of hydrocephalus making infective etiology as the cause in 18 (36%) cases. Intra 4th ventricular neurocysticercus cyst caused blockade of CSF pathway in 2 children. 15 out of 50 children required shunt revision, either due to infection (8,16%) or shunt obstruction (7, 14%). Multiple shunt revisions were required in 2 children only. These revisions were required due to infection, obstruction or malfunction of the shunt. Conclusions : Infective etiology is responsible for hydrocephalus in significant number of children (36%). The possibility of TORCH infection, as a cause of hydrocephalus should be considered even amongst the children of screened mothers during antenatal check-up. Pure intra 4th ventricular neurocysticercus cysts (without intraparenchymal cyst), though rare, can manifest with outlet obstruction. Incidence of shunt revision using Chhabra's medium pressure shunt is very high in children at an average follow up of 1.6 yr. Post infective hydrocephalus is a major cause of delayed milestones, contributing to mental retardation. Keywords: Hydrocephalus; Etiology; Complication; Shunt revision How to cite this article: Kumar R, Singh V, Kumar MV. Shunt revision in hydrocephalus. Indian J Pediatr 2005;72:843-847 How to cite this URL: Kumar R, Singh V, Kumar MV. Shunt revision in hydrocephalus. Indian J Pediatr [serial online] 2005 [cited 2006 Aug 9];72:843-847. Available from: http://www.ijppediatricsindia.org/article.asp?issn=00195456;year=2005;volume=72;issue=10;spage=843;epage=847;aulast=Kumar Hydrocephalus has been the focus of more dedicated study and investigation than perhaps any other condition afflicting the human nervous system. For many centuries patients with hydrocephalus had limited expectations for survival. With the development and refinements of modern cerebrospinal fluid (CSF) shunt, normal learning and intelligence is now possible and patients are able to enjoy full participation in all facets of life. CSF shunt diversions though have many complications, the most common being shunt obstructions and infection which require the attention of neurosurgeons. The frequency of shunt revisions in the 1st year and in the 10th yr have been studied in detail amongst the hydrocephalic children harbouring spinal dyspraphism[1], where 30-40% children require at least one shunt revision during first years of life; of these 15 to 20% require multiple revisions and 85% undergo at least one shunt revision during first 10 yr.[1] However, the incidence of shunt revision is not known in other hydrocephalic children. The present study is a retrospective analysis of hydrocephalic children who had undergone CSF shunt diversion. The etiology, clinical profile and complication of shunt procedures are studied in the Indian children. The frequency of shunt revisions and their outcome has also been studied. » Materials and Methods Analysis of a cohort of 50 children of hydrocephalus retrospectively, who underwent a ventriculoperitoneal shunt insertion during 1997 to 2001 in the Neurosurgery Department at Sanjay Gandhi Post Graduate Institute of Medical Sciences, India was done. The following details were ascertained from the case record files, discharge summaries and follow-up register maintained by a pediatric neurosurgeon : name, age, sex, etiology, clinical profile, imaging and treatment. Record of shunt revisions, complications and outcome at follow-up of each case was maintained in the computer database and follow-up register. Children having a minimum follow-up of 6 months were included in this analysis and those with an adequate follow-up but inadequate records (etiology, procedure, complications and follow-up) were excluded. Children with active signs of meningeal irritation, and tumors as the cause of hydrocephalus were also excluded. Children included in the analysis underwent medium pressure Chhabra's shunt, either by the principal author himself or under his direct supervision, particularly when the procedure was performed electively. Chhabra's shunt is made up of implant grade silastic material and has a ventricular end, a chamber and a peritoneal end. The chamber has a spring in slit. The CSF flow is pressure regulated and flow rate type. There are around 40 holes in the 1.5cm length of the radio-opaque ventricular end. The peritoneal end is also radio-opaque. It is an economically sound shunt used widely throughout India as well as in the neighboring countries. The clinical features of children in study are summarized in [Table - 1]. » Results The fifty children included in the study comprised of 42 males and 8 females with a ratio of 5.25: 1. The age at the time of shunt insertion for the first time ranged from 1 month to 12 yr (mean 2.2 yr). Follow-up ranged from 6 months to 2 yr (mean 1.6 yr). Each child had undergone an initial CT scan. MRI was performed in cases where there was a suspicion of a structural lesion causing hydrocephalus. The causes of hydrocephalus amongst the children in this study are mentioned in [Table - 2]. The children of TORCH infection were diagnosed by presence of periventricular calcification [Figure - 1]. The diagnosis was confirmed by serum and CSF ELISA. Both the children of neurocysticercus cyst had history of tonic clonic seizures along with raised intracranial pressure (ICP). Emergency shunt was inserted in one of these as he presented acutely with altered sensorium and features of raised ICP, the cyst was enucleated at a later date in this child [Figure - 2]. An elective shunt was performed in the other child, where the cyst could not be defined at the first presentation on CT scan. The 4th ventricular cyst was enucleated when the child had a suspected shunt malfunction at 9 months, when CTscan also confirmed the diagnosis. A single premature baby of 7 months gestational age having a birth weight of 1500gm was diagnosed to have hydrocephalus 1 month following birth due to intraventricular hemorrhage. An elective ventricular tap revealed xanthochromic CSF, suggesting an old bleed, further confirmed by biochemical and cytological analysis. Within a period of 4 months, shunt revision was required twice due to shunt blockade on him. The child remained mentally deprived at 1-year follow-up. Two of four children with Dandy Walker malformation had mental retardation at follow-up, though there was no evidence of structural anomalies of the cortex. Complications Fifteen of the fifty cases required shunt revisions during a mean follow-up of 1.6 yr due to one or the other reason. Two of these 15 cases required multiple shunt revisions (1 child of meningomyelocele had 5 shunt revisions in a period of 8 months and 1 with an intraventricular hemorrhage had two shunt revisions in a period of 4 months). Shunt infection was the first and foremost cause of shunt revisions in 8 (16%) children (0.16 per case and 0.14 per procedure). Shunt obstruction was the second cause in 7(14%) children (abdominal end of the shunt getting blocked in 2 and ventricular end in 5). Three of 8 shunt infections developed wound dehiscence at 9 weeks in one child and at 2 months in the other 2 children. Scalp wound demonstrated growth of staphylococcus epidermidis and the peritoneal wound showed E. coli and pseudomonas on culture. Two of the 8 children developed infection of subdural hygroma along with shunt infection. Three of the 8 children presented with meningismus and fever for a few days to weeks duration. Features of raised intracranial pressure and pericatheteral CSF filling due to occult leak from ventricular end were the manifestations in two other children. One of these two had episodic tonic posturing of the body for a month along with left hemiparesis. Loss of bilateral vision and secondary optic atrophy was noted in another child of aqueductal stenosis who had undergone ventriculoperitoneal shunt 1.8 yr ago. All the 8 children were treated either by exteriorization of shunt or by installing omaya reservoir, followed by intermittent tapping. External ventricular drainage was maintained till CSF cytochemical analysis, microscopy and culture sensitivity proved an absence of infection. Antibiotics were given for 4-6 weeks (even if CSF was sterile) on the basis of culture and sensitivity of CSF, shunt tubes or wound swabs. Both ends of the removed shunt tube were subjected to culture and sensitivity in all cases of shunt removal. In the event of sterile CSF, broad spectrum antibiotic like cefotaxim/amikacin and metronidazole were given in an injectable form for 2 to 3 weeks, followed by broadspectrum oral therapy for further 3 - 4 weeks. In severe infection of CSF, intraventricular gentamicin was given on alternate days. Reinstallation of a new shunt assembly was done only after two consecutive CSF samples came out to be normal biochemically and cytologically. Outcome Thirty-five of the 50 children had no complication following shunt insertion and improvement was noted in neurological/functional status of the subjects at follow-up. Analysis of the neurological/functional outcome revealed that 15 of the 50 cases continued to have delayed milestones at follow-up and they required some sort of functional assistance in their day-today activities. On the basis of etiology, 3 of these 15 had a congenital infection, 5 with posttubercular meningitis, 2 with nontubercular bacterial infections, 2 with Dandy walker syndrome, 2 had an associated spinal dysraphism and 1 had an intraventicular hemorrhage. Results reveal that children with an infectious etiology (post-infective n=15, congenital infection n=3) had a higher incidence of dependence on their families for their day-to-day activities in comparison to other etiologies of hydrocephalus (10 of 18 infective etiology were dependent, 55.6%). » Discussion Most infants presenting with progressive hydrocephalus are treated either with ventriculoperitoneal shunt CSF diversion or 3rd ventriculostomy. Although the risk in performing a shunt is low, complications related to shunt diversion are many, hence each child needs to be assessed individually, weighing the risk of surgery vs no treatment. The outcome of shunt diversion depends on a number of factors which include concomitant medical problems, the degree of neurologic compromise at the time of surgery, the nature, etiology, duration and severity of hydrocephalus, status of cortical mantle, structural anomalies, timing of shunt etc[1]. Etiological Factors and Their Relation to the Outcome Amongst the etiological factors, congenital aqueductal stenosis accounts for 10% of all hydrocephalus cases in children.[1] Aqueductal stenosis remained the most common cause of hydrocephalus amongst children in the present study as well (n = 18, 36%). A higher incidence can be explained on account of the exclusion criteria in the present study, where idiopathic cases, tumors etc as a cause of hydrocephalus were excluded. None of these children showed mental retardation. All children of school age attended school normally and were not dependent on their families for their day-to-day activities. Tuberculosis is a serious health problem in the developing countries. Most patients with central nervous system tuberculosis have an identifiable systemic disease. Hydrocephalus develops more frequently in these patients and almost always manifests itself within 4 - 6 weeks of the disease[2],[3]. In the present cohort of hydrocephalic children, 10 (20%) had post TBM hydrocephalus. All cases responded well to antitubercular therapy with CSF diversion. The older children manifested with mental retardation or delayed milestones, probably due to extensive involvement of brain parenchyma and delayed shunting in them, and they lagged behind their siblings in school at follow-up. Hydrocephalus is an uncommon complication of childhood bacterial meningitis but occurs more frequently in neonates recovering from meningitis. In most cases, the complication develops insidiously over weeks to months. Severe neurologic sequelae such as hemiplegia/quadriplegia, hyperactivity and mental retardation are relatively uncommon in these patients (less than or equal to 4% of all children recovering from bacterial meningitis), although such sequelae are relatively more frequent after neonatal meningitis[1]. Five of the 50 children in the present study had nontubercular meningitis as the cause for their hydrocephalus. One of these patients had hemiplegia and 2 showed mental retardation at follow-up even after shunting. Cytomegalovirus, rubella, mumps, varicella, and parainfluenza virus can cross the placenta and have been implicated as a cause of congenital hydrocephalus. Congenital infection (TORCH) was the cause of hydrocephalus in 3 children in the present study (6%). All these children showed delayed milestone at follow-up. Neurocysticercosis is a leading cause of seizures, hydrocephalus and learning disability in children and adults.[4],[5] In the present study, 2 of 50 children, had 4th ventricular outlet obstruction due to neurocysticercus cysts. Enucleation of the cyst from the 4th ventricle was done in 1 child who had undergone an emergency VP shunt at presentation, while in the other the cyst was enucleated 9 months later, when he presented with shunt malfunction. At followup both of them were doing well in school and showed no mental retardation or neurological compromise. The influence of the etiology of hydrocephalus on outcome has been studied by various authors with differing conclusions, which no doubt reflects the heterogenesity of the underlying conditions.[6],[7] In this analysis etiology did influence the outcome significantly, as the children with hydrocephalus secondary to infections were more than 3 times likely to require assistance in their day to day activities (55.6% vs 15.6%), as compared to the other diagnostic categories (as shown in literature[8]. The present results, however, did not confirm the finding of a higher incidence of poor intellectual outcome in aqueduct stenosis or noncommunicating hydrocephalus.[6] Complications of Shunt Shunt obstruction has been found to be one of the important causes of shunt failure requiring revision. The most common shunt malfunction was found to be at the ventricular catheter as reported in literature[9]. In the present study mean follow-up period of 1.6 yr, 5 of 7(71%) shunt obstruction cases had a proximal block of ventricular end. Distal obstruction is seen principally if the distal end is placed in the pre-peritoneal space. Low-grade infection with intra-abdominal loculation or pseudocyst formation, disconnection, ingestion and withdrawal of the catheter from the peritoneum are the other causes of distal malfunction[10]. Two children in the present analysis demonstrated block at the peritoneal end, most probably with mental tissue, where the distal tubes started to drain once the peritoneal tips were cut. Most centers report infection rates in the order of 5 to 10%.[1] These infections usually present within two months of shunt insertion, suggesting that most of these occur during the surgery itself.[11] The infection rate in the present study is 16% (n=8), (0.16 per case and 0.14 per procedure) in the mean follow-up period of 1.6 yr. This is quite disappointing by the present standards[12] and reflect that the children under 6 months (n=21, 42%) are significantly at risk for infective complications. According to etiology and clinical presentation the shunt infection has been divided into external and internal type. Though the manifestations of both are different, a few of them may present with atypical manifestations not coinciding with either of the two. Two children in the present study presented with atypical manifestations of shunt infection like diffuse pericatheteral swelling and globular swelling at the ventricular end[13]. Organisms of low virulence generally cause infection of CSF shunts. Staphylococcus epidermidis is the most commonly found organism in most series[14]. Staphylococcus aureus, Gram-negative bacilli, and mixed infections are the next most common agents encountered. In the present analysis, 6 out of the 8 children showed shunt infection due to staphylococcus species and the rest 2 had infection due to pseudomonas and E. coli species. Infection was managed by the removal of the infected shunt assembly and placement of omaya reservoir (for regular tapping of CSF) or external ventricular drainage if need arose. A course of 4 to 6 weeks antibiotics was chosen on the basis of culture and sensivity of CSF, shunt tubes or wound swabs, and broad-spectrum antibiotics were administered if cultures failed to reveal any pathogen. Intraventricular antibiotics were also administered in severe infections. A new shunt assembly was installed once the CSF became clear biochemically and microscopically on two consecutive testing. If the CSF is flowing through the shunt more quickly, the ability of the brain to expand, the cortical mantle, may remain unexpanded and subdural fluid collections may develop. In the present study, two children had subdural hygroma due to overdrainage of CSF. This incidence might have been higher in the present series but we could document only two symptomatic cases mainly because of adventitious infection. Being a retrospective analysis, the study suffers from its own set of limitations. A short follow-up is an unacceptable compromise to the ideal situation of a prospective study. The validity of this study could also be improved by recruiting large number of patients. But practically, this was possible only in a multicenter study, as follow-up is a real problem in the developing milieu. » Conclusion The development of effective cerebrospinal fluid (CSF) shunts represents a landmark in neurosurgery. Apart from congenital aqueductal stenosis, post-infective hydrocephalus remains the commonest cause of hydrocephalus in developing countries. Treatable cause like TORCH infection in the mother may manifest with hydrocephalus in the newborn and this is accountable to inappropriate antenatal screening, immunization and ignorance. Intra 4th ventricular neurocysticercus cyst may rarely contribute to the blockade of CSF pathway without the evidence of any other cyst in parenchyma or ventricular system. Complications of shunt, like infection and obstruction are quite disappointing and have a high incidence of around 30% to warranting shunt revisions. Delayed milestones, mental retardation and dependence for day-to-day activities are more marked with the infective etiology of hydrocephalus. » References 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. Mark S. Dias. Myelomeningocele. In Maurice Choux, Concezio DI Rocco, AD Hockley, ML Walker, eds. Text book of Pediatric Neurosurgery. 1st edn, Churchil Livingstone 1999; 43; 253- 269. Farinha NJ, Razali KA, Holzel H, Morgan G, Novelli VM. Tuberculosis of the central nervous system in children : A 20 year survey. J Infect 2000; 41 : 61-68. [PUBMED] [FULLTEXT] Faulhauer K, Schmitz P. Overdrainage phenomena in shunt treated hydrocephalus. Acta Neurochir 1978; 45 : 89-101. [PUBMED] Lowichik A, Siegel JD. Parasitic infections of the central nervous system in children : I. J Child Neurol 1995; 10 : 4 - 17. [PUBMED] Lowichik A, Siegel JD. Parasitic infections of the central nervous system in children : II. J Child Neurol 1995; 10 : 77-87. McCullough DC, balazer-Martin LA. Current prognosis in overt neonatal hydrocephalus. J Neurosurg 1982; 57 : 378-383. Renier D, Saint-Rose C, Pierre-Kahn A, Hirsch JF. Prenatal hydrocephalus : outcome and prognosis. Childs Nerv Syst 1998; 4 : 213-222. Gasey ATH, Kimmings EJ, Kleinlugtebeld AD, Taylor WAS, Harkness WF, Hayward RD. The long-term outlook for hydrocepahlus in childhood. A ten-year Cohort Study of 155 patients. Pediatr Neurosurg 1997; 27 : 63-70. Drake JM, Kestle J, Milner R et al . Randomized trial of cerebrospinal fluid shunt valve design in pediatric hydrocephalus. Neurosurgery 1998; 43 : 294 - 305. Ginsberg HJ, Sum A, Drake JM et al. Ventriculoperitoneal shunt flow dependency on the number of patent holes in a ventricular catheter. Pediatr Neurosurg 2000; 33 : 7-11. Pople IK, Quinn MW. Morbidity and outcome of shunted hydrocephalus. Z Kinderchir 1990; 45 (Suppl I) : 29. Choux M, Genitori L, Lang D, Lena G. Shunt implantation : Reducing the incidence of shunt infection. J Neurosurg 1992; 77 : 875-880. [PUBMED] Raj Kumar. Uncommon manifestations of shunt infection. Indian J Pediatr 2003; 70(1) : 21-24. Bayston R. Epidemiology, diagnosis treatment and prevention of CSF shunt infection. Nuerosurg Clin Am 2001; 12 (4) : 703- 707.