Design of a neck brace for patients with ALS
advertisement

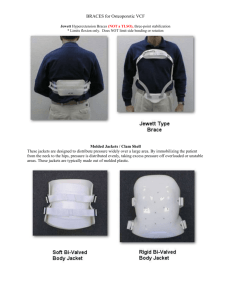
Design of a Neck Brace for Patients with ALS Sarah Calano1, Maneesha Kumar1, Amy McNeal1, Brooke Odle2 1 BS Bioengineering (April 2006), Department of Bioengineering, University of Pittsburgh, Pittsburgh, PA 15261, USA 2 BS Bioengineering (December 2006), Department of Bioengineering, University of Pittsburgh, Pittsburgh, PA 15261, USA Corresponding Author: Mark Gartner Phone: (412) 828-5209 ext. 200 Fax: (412) 828-5229 mgartner@enison.com 1 ABSTRACT “Dropped head syndrome” is a condition found in the elderly and individuals suffering from several neuromuscular degenerative disorders such as amyotrophic lateral sclerosis (ALS). Although they remain able to rotate their head laterally, weakened neck extensor muscles do not allow them to support their head, causing them to turn to neck brace support. ALS is a progressive disease and affects different parts of the body at differing points in time. Thus, an individual with dropped head syndrome may be functioning normally in nearly every other respect. No commercially available neck brace is customized for patients suffering from ALS – instead they are normally designed for victims of neck trauma. Thus, these braces are designed to completely immobilize the head and specifically not allow any lateral mobility. As a result of these shortcomings, an ALS specific neck brace was designed based on reviews of orthotists, clinicians, and patients. Our purpose was to create a neck brace with adequate vertical support, lateral mobility, and an open design for patients suffering from dropped head syndrome. Keywords: dropped head syndrome, amyotrophic lateral sclerosis, neck brace INTRODUCTION Amyotrophic lateral sclerosis (ALS), also known as Lou Gehrig’s disease, is a progressive, degenerative, fatal neuromuscular disease. The disease is caused by the degeneration of upper neurons in the motor cortex and lower motor neurons in the brainstem and spinal cord.1 The characteristic symptoms of this disease include muscle weakness and wasting, fasciculations, and increased reflexes. Eventually, those suffering from ALS lose motor function in their limbs, respiratory control as a result of diaphragm 2 weakness, or paralysis leading to issues with speech and swallowing. About 30,000 Americans have been diagnosed with ALS, a disease that typically affects older adults, with a peak age of onset between 55 and 75 years2. ALS occurs in three forms: bulbar, upper limb onset, and lower limb onset. For the purposes of our neck brace design and its treatment for dropped head syndrome, this paper will only address the upper limb onset. Dropped head syndrome is caused by neck extensor weakness, and is seen in the elderly and those suffering from one of many neuromuscular disorders such as myasthenia gravis and ALS.3 ALS patients that suffer from dropped head syndrome are unable to lift their chin off of their neck due to the extent of weakness in the extensors. Generally, there are tears in the extensors that lead to the weakness. Over time, the muscles in the front of the neck shorten, while the muscles in the back of the neck lengthen (“R Mawhinney, personal communication, 2005”). However, ALS does not have only physical effects, but it also affects patients emotionally since they have no knowledge of prevention or cure. To many patients, they feel that their condition makes them appear mentally disabled, when there has often been no effect on their sensory function or intellectual integrity. To promote a more normal lifestyle for the patients and to counteract social embarrassment, physicians have recommended that patients wear a neck brace (Figure 1). However, for many patients it is difficult to accept the fact that they need such support, and using one often means that they finally need to accept the fact that they suffer from the disease (“L Talmon, personal communication, 2005”). Initially, many patients 3 choose soft cervical collars, and wait to purchase more specialized neck braces like the Headmaster Wire Frame Collar (Figure 2) when the disease further progresses. However, none of the current neck braces out on the market are customized for ALS patients. Upon first fitting, most braces seem to be comfortable and supportive, but after a few hours, the patient often finds them extremely uncomfortable and takes them off. Not only do these braces cause discomfort, but they also do not provide adequate support for ALS patients. Therefore, the goal of our project was to create a neck brace that was capable of restoring proper head position for individuals with decreased neck muscle strength, allowing normal interaction with their environment. A special attempt was made to ensure that the neck brace was comfortable and allowed lateral mobility. METHODS To determine the essential performance requirements of an ideal ALS specific neck brace, clinicians and patients were consulted about important requirements and features. Patients were interviewed about their current neck brace, the amount of time per day that they wore the brace, the issues with their current brace, and their idea of an ideal neck brace. Based on their suggestions, initial sketches were drawn and taken to Hanger Orthotics and Prosthetics (Pittsburgh, PA) to be prototyped. After several design iterations based on the feedback of Hanger personnel and ALS clinicians, prototypes were created. In order to evaluate the effectiveness of our design solution, the prototype was reviewed by an orthotist, multiple clinicians, and ALS patients. No prototype was reviewed or worn by a patient until it had received approval from the clinicians. 4 Design Considerations: Clinicians find that ALS patients who currently wear neck braces encounter five main hazards: suffocation, skin irritation, overheating, difficulty swallowing, and neck soreness/pain. Suffocation can occur when the collar material is either collapsible or too stiff. In the first case, the head drops over the brace constricting the neck, while in the second case, the head falls down into the brace blocking the nose and mouth. In some cases, patients were found slumped over and their brace had cut off their air circulation thus causing suffocation (“L Talmon, personal communication, 2005”). Skin irritation becomes an issue when patients wear the neck brace on a daily basis. Because the neck brace is used constantly, it tends to rub against the skin, causing breakdown. Overheating occurs when there is a lack of ventilation in the design of the neck brace. Soft cervical collars and closed designs completely cover the neck. Difficulty swallowing can be a result of the chin being positioned too high or because of pressure applied to the neck area. Positioning errors can be caused by patient use errors or by the inherent non-adjustability of the design. Pressure on the neck area is due to neck braces that lack girth adjustability in their design and do not accommodate larger patients. The additional neck soreness and pain encountered is due to the improper positioning of the neck brace. Our goal was to create a neck brace that would minimize all of these problems. Human Factors Considerations: Because patients wear the brace while walking, driving, and during most daily activities, it was important to consider the effects on the user using human factors analyses. For example, a neck brace that allows for lateral rotation of the head is very beneficial to patients who walk with the aid of a cane. Since 5 current neck braces immobilize the neck, it is difficult see when they are walking. Because the amount of time that the brace is worn greatly depends upon how it feels, special considerations for comfort were necessary. In order to create a brace that is durable, effort was made to include washable or easily replaceable components. Regulatory Considerations: This neck brace would be classified as a Class I device and considered a “cervical orthotic”. The current neck braces, and specifically those with wire frame designs, possess the same classification. Patent and patent application searches were performed to make sure that no feature of the brace would infringe upon any other product. Patients would receive access to this device through physician recommendations and orthotic companies. According to Medicare reimbursement protocols, patients would most likely not have to pay for the device, as it would be covered by insurance. Design Equipment & Materials: In addition to hand sketches, SolidWorks 2005, a 3-D solid modeling computer aided engineering (CAE) software program, was used to generate final drawings. This allowed for modeling the sketches in three-dimensions, so that each prototype could be analyzed from different views. A VICON motion tracking system was used to three-dimensionally locate a point on the chin. Signals from a reflective marker on the chin were recorded as the head was laterally rotated. These points were then used to trace the chin’s path of motion during head rotation. 6 Material choices for the final design were based upon low weight, high strength, and the ability to be molded. For prototyping purposes, a stereolithography (SLA) rapid prototyping system was used to create the sliding track mechanism from resin. The other components of the prototype were fabricated at Hanger Orthotics and Prosthetics; however for mass production, a casting process would most likely be used. RESULTS After five design iterations, our final prototype resulted in a wire frame base and sliding track mechanism (Figure 3). Vertical support bars were place in the front, but as far to the sides as possible. The sliding track allowed a chin piece to move within a tgroove over a total range of 60 degrees (30 degrees of head rotation to each side). The outer chin piece was made with closed cell polyethylene foam and lined with open cell foam (memory foam) to shape to the anatomical contours of individual users. The posterior neck support was made from closed cell foam and was supported with low density polyethylene plastic to prevent buckling and breakdown. Padding was placed along the wire frame to cover the sternum and to distribute the forces evenly. Materials chosen for the prototype were based upon availability and do not necessarily represent final production materials (Table 1). Throughout the design progression, clinicians and patients were interviewed on the design and gave input and suggestions. For the two prototyped designs, formal surveys were given to clinicians and patients to quantify the success of the design and to clarify what features required improvement. The brace was ranked on comfort, 7 functionality, appearance, and overall design and the results are represented in Tables 2 and 3. DISCUSSION Design Solutions Hazards: To provide a comfortable patient interface, padding was made from non-abrasive, non-allergenic material to prevent skin breakdown. Additionally, all padding was designed to be easily replaceable or washable. To prevent overheating, an open design was incorporated and the weight of the brace was minimized to less than one pound. Non collapsible materials and adjustability were incorporated to prevent suffocation and additional neck soreness/pain. Human Factors: The 60 degree range of motion allowed the users to accomplish daily activities by permitting them to rotate their head while walking or eating. To allow easy maintenance of the device, the soft goods were designed to be replaceable or washable every six months, resulting in a very durable design. Design Evolution The design progression of the ALS specific neck brace can be seen in Figure 4. Initially, the lateral mobility was incorporated through ball and socket pivot joints at the base of the brace (Figure 4a). However, it became clear that pivot joints do not provide adequate support as they tend to collapse from side to side. Through the use of the VICON motion tracking system, we were able to determine that the chin’s arc of motion was constant and circular for 60 degrees. This circular motion led to the design based upon a simple pivot joint at the chin (Figure 4b). 8 However, the radius required for this pivot was 3.25 inches and was therefore too large to fit underneath the chin. Instead of the pivot design, the chin’s path of motion was used to create a tracking system (Figure 4c). In this iteration, a chin support piece was designed to move along a recessed track, providing up to 60 degrees of rotation. This track was attached to the wire frame base through height adjustable bars. However, the design was deemed unfeasible since the bars were slanted, and any adjustment would cause the chin piece to move outward and protrude from the neck. Design four, also our first prototype, maintained the concept of the chin track for lateral motion (Figure 4d). The t-groove track system was instead supported through non-adjustable front supports. Alternatively, we decided that height adjustability could occur through various device sizes and heights of the chin piece itself. However, the stability of this brace was an issue since the Velcro straps attached to the front supports at an angle and pulled back at an upward angle. This angle destabilized the brace and did not allow proper girth adjustment. Additionally, the entire pressure of the brace and head concentrated on one point at the sternum. The pressure on this bony prominence was unbearable for long periods of time and the brace did not have enough padding to distribute the load. The fifth design iteration was created after receiving the feedback of the clinicians. In this final design, the support bars in the front of the brace were positioned vertically and further to the sides (Figure 5). Thus, the Velcro straps attached vertically, and pulled back directly, stabilizing the brace. At the point of pressure on the sternum, memory foam padding was added to distribute the weight of the brace. This greatly 9 increased the comfort of the device, and removed the direct pressure point on the bone. Lastly, the chin piece was lined with memory foam to fit the anatomical contours of the user, and to provide a more comfortable and stable support for the chin. Conclusion Thus, overall this neck brace design provides full vertical support while allowing for lateral mobility. Design features including an open design, non-collapsible material, nonabrasive skin contact surfaces, and adjustability were incorporated to prevent hazards and provide ease of use. This customized design will allow patients with amyotrophic lateral sclerosis (ALS) and other neuromuscular degenerative diseases to participate in normal daily activities and increase their quality of life. 10 ACKNOWLEDGEMENTS The authors would like to thank Mr. Robert Mawhinney of Hanger Orthotics and Prosthetics, Inc for his assistance in the design and prototyping process of the neck braces, Ms. Linda Talmon of the ALS Society of Pittsburgh for serving as our mentor and presenting us with our design problem, Dr. Sandeep Rana and Dr. Barbara Swan of the ALS Clinic at Allegheny General Hospital in Pittsburgh, PA for allowing us to meet with their patients and giving us a clinician’s point of view regarding our designs, Mr. James Joyce, an ALS patient who provided us with ample feedback on our prototype, Mr. Mike Rose of the ALS Society of Pittsburgh for his neck brace design insight, Mr. Mark Gartner, Professor of the University of Pittsburgh’s Bioengineering Senior Design Course, for his continuous feedback on the progress and documentation of our project, and the Bioengineering Department at the University, Dr. Hal Wrigley, and Dr. Linda Baker for their generous financial gift used to fund this project. REFERENCES 1. Charles T, Swash M. Amyotrophic lateral sclerosis: current understanding. Journal of Neuroscience Nursing 2001; 33(5): 24553.[PubMed] 2. Walling, A, MD. Amyotrophic Lateral Sclerosis: Lou Gehrig’s Disease. American Family Physician March 15, 1999:59(6). Retrieved November 28, 2005 from http://www.aafp.org/afp/990315ap/1489.html. 3. Gourie-Devi M, MD, Nalini A, Sandhya S. Early or late appearance of “dropped head syndrome” in amyotrophic lateral sclerosis. Journal of Neurology and Psychiatry 2003; 74: 683-686.[PubMed] 11 Note: This appendix page will not appear in the actual article. It’s just here for reviewing purposes because the tables, figures, and figure legends must be on separate pages, but referenced in the article. Appendix 1. 2. 3. 4. 5. 6. 7. Figure 1 Figure 2 Figure 3 Figure 4 Figure Legend Table 1 Table 2 12 (a) (b) (c) Figure 1. Current Neck Braces used by ALS patients. (a) Philadelphia C-Breeze Collar (b) Executive Collar (c) Aspen Cervical Collar Figure 2. Headmaster Cervical Collar. 13 (a) (b) (c) (d) Figure 3. Final Prototype of the ALS Neck Brace. 14 (a) Design Iteration 1 (b) Design Iteration 2 (c) Design Iteration 3 (d) Design Iteration 4 Figure 4. Neck brace design progression 15 Figure Legend Figure 1. Current Neck Braces used by ALS patients. (a) Philadelphia C-Breeze Collar (b) Executive Collar (c) Aspen Cervical Collar Figure 2. Headmaster Cervical Collar. Figure 3. Final Prototype of the ALS Specific Neck Brace. (a) Front view of the final prototype (b) Side view of the final prototype (c) View of the posterior support of the neck brace (d) View of the chin piece of the neck brace Figure 4. Evolution of the Neck Brace (a) Design Iteration 1 of the neck brace (b) The results of the motion test (left); Design Iteration 2 of the neck brace (right) (c) The track mechanism (left); Design Iteration 3 of the neck brace (right) (d) Front view (left) and side view (right) of the first prototyped neck brace 16 Table 1. Materials used for the current prototype and ideal materials for manufacturing Brace Component Wire Frame Base Prototyped Brace Steel Actual Brace Aluminum wire or High Density polyethylene Track WaterShed 11120 Resin Any material with a low coefficient of friction that can be cast Padding Temperfoam, Plastazote, Closed cell foam, Surgical tubing Temperfoam, Plastazote, Closed cell foam, Surgical tubing 17 Table 2. Clinician survey (n=2) results for Design 4 (Prototype 1) Topic Functionality Comfort Appearance Overall Design Clinician Score 19/20 17/20 9.5/10 10/10 Table 2. Clinician (n=3) and patient (n=1) survey results for Design 5 (Prototype 2) Topic Functionality Comfort Appearance Overall Design Clinician Score 19.7/20 19.7/20 9.5/10 10/10 Patient Score 20/20 20/20 7/10 10/10 18