Ultrasound Needling Technique
advertisement
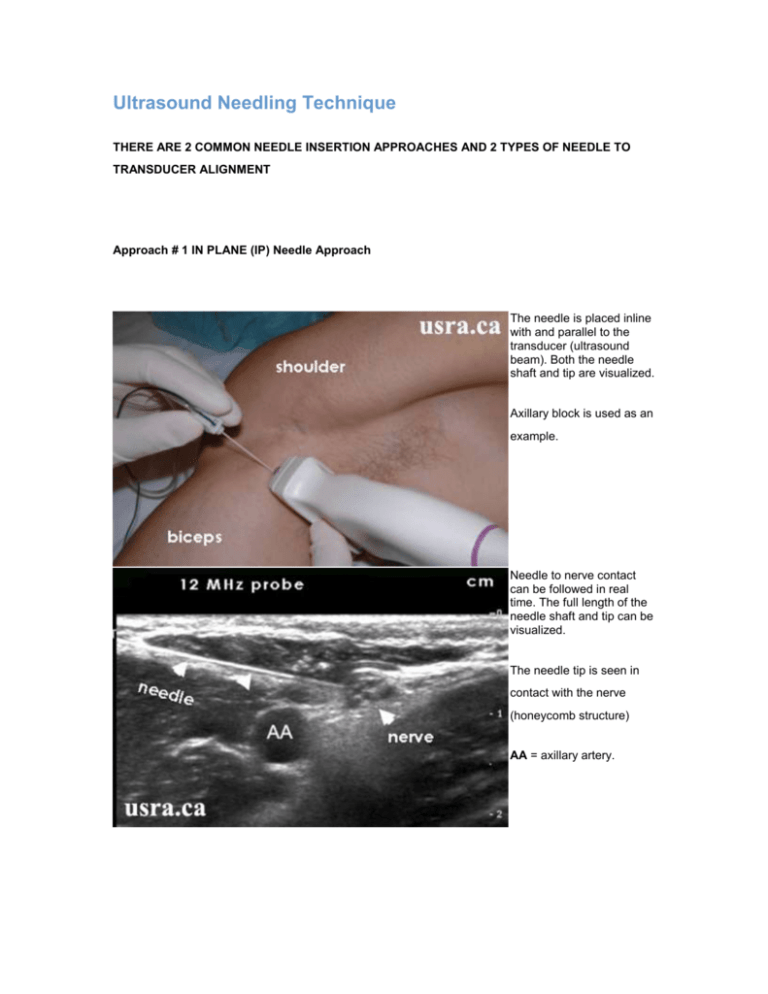
Ultrasound Needling Technique THERE ARE 2 COMMON NEEDLE INSERTION APPROACHES AND 2 TYPES OF NEEDLE TO TRANSDUCER ALIGNMENT Approach # 1 IN PLANE (IP) Needle Approach The needle is placed inline with and parallel to the transducer (ultrasound beam). Both the needle shaft and tip are visualized. Axillary block is used as an example. Needle to nerve contact can be followed in real time. The full length of the needle shaft and tip can be visualized. The needle tip is seen in contact with the nerve (honeycomb structure) AA = axillary artery. APPROACH # 2: OUT OF PLANE (OOP) NEEDLE APPROACH The needle is placed perpendicular to the transducer. The needle shaft and tip are visualized as a hyperechoic dot on ultrasound. The femoral nerve block is used as an example. In this case, needle, nerve and tissue movements are observed. The needle tip (NT) may be difficult to locate accurately without the use of echogenic tip needles. Actual needle to nerve contact can be confirmed by nerve stimulation and local anesthetic (LA) spread pattern. FA, FN & FV = femoral artery, nerve & vein; IPM = iliopsoas muscle NEEDLE HANDLING Proper needle handling skills are required for accurate and smooth needle insertion during ultrasound guided nerve blocks. If the operator is not ambidextrous, and prefers to use the dominant hand to handle the needle and inject local anesthetic, then the operator must choose a proper body location and orientation in relationship to the patient. This is an example of a right handed operator using the right hand to hold the needle for a left sided interscalene block. Note that the operator is standing on the left side of the patient below the clavicle. This is an example of a right handed operator using the right hand to hold the needle for a right sided interscalene block. Note that the operator is now standing on the right side of the patient above the clavicle. BODY ERGONOMICS Proper body ergonomics to handle the transducer and the needle, to view the screen, and to position the patient are essential for block success and to avoid operator fatigue and body injury. Below are some examples of proper and improper body ergonomics. Proper operator and screen orientation; note that the ultrasound machine is placed directly in front of the operator to provide a direct line of vision. Improper operator and screen orientation; note that the operator’s head is turned almost 90 degrees to view the ultrasound image on the screen. Proper body position and bed height for the procedure Improper body position; the bed is too low for the procedure Proper transducer holding skill; the hand is placed close to the transducer contact surface Improper transducer holding position; the hand is high up on the transducer Proper hand and arm positions; both hands and arms are comfortably supported Improper hand and arm positions; both the arm holding the transducer and the hand holding the needle are not supported NEEDLE TO NERVE CONTACT AND INJECTION STRATEGY 1. Perineural Injection The goal is to place the needle tip on each side of the target nerve (i.e., perineural) but not inside the nerve (i.e., intraneural). Avoid direct head-on needle to nerve contact (figure A). Aim to inject local anesthetic around the nerve and not inside the nerve (figures B and C). Perineural injection is visualized as an expanding collection of hypoechoic fluid around the nerve. Circumferential spread is generally a good indication of adequate local anesthetic spread (“donut sign”). Figure A shows needle in contact with nerve Figures B & C show local anesthetic injection around the nerve LA = local anesthetic White arrows = block needle Yellow arrowhead = nerve 2. Recognition of Improper Local Anesthetic Spread An Illustration of Local Anesthetic Spread During Femoral Nerve Block Figure A shows an improper injection outside the fascia iliaca (FI). Arrows show tissue expansion outside the fascia. Figure B shows a proper injection deep to the fascia iliaca (FI). Arrows show fluid expansion deep to the fascia. FA = femoral artery An Illustration of Proper and Improper Local Anesthetic Spread During Popliteal Sciatic Nerve Block Figure A illustrates improper injection and subsequent hypoechoic local anesthetic spread (asterisk) outside the fascial sheath of the sciatic nerve (hyperechoic structure) in the popliteal region. Figure B illustrates proper injection (asterisks) inside the fascia sheath of the sciatic nerve. An Illustration of Proper and Improper Local Anesthetic Spread During Supraclavicular Brachial Plexus Block Figure A illustrates improper injection and hypoechoic local anesthetic (LA) spread outside the brachial plexus sheath. Arrowheads = nerve trunks FR = first rib PL = pleura SA = subclavian artery Figure B illustrates proper injection (LA) inside the expanded brachial plexus sheath. 3. Recognition of Intraneural Injection Intraneural injection is manifested by an expansion of nerve diameter (yellow arrowheads) with as little as 1mL of injection (figure B). Another hint of an intraneural puncture is nerve movement towards the needle as the needle is withdrawn. The nerve should be moving away from the needle under normal circumstances. Ultrasonographic Appearance of An Intraneural Injection Pre-injection Post-injection 4. Hydro Dissection Technique The hydro dissection technique is most useful for “dissecting” out the intermuscular or interfascial plane in which a small nerve lies. Injection of 5-10 mL of fluid (saline or D5W) through the needle can distend and open up the narrow space so that the small nerve is more clearly visualized before local anesthetic injection. Hydro dissection is particularly useful for blockade of smaller nerves located between muscular planes e.g., 1) ilioinguinal and iliohypogastric nerves; 2) the rectus sheath block; 3) obturator nerve; 4) saphenous nerve and 5) transverse abdominis plane block. Figure A shows hypoechoic ilioinguinal/iliohypogastric nerves (arrowheads) within the plane between the internal oblique muscle (IOM) and the transverse abdominis muscle (TAM). Figure B shows needle (arrows) approaching the nerves using the in plane needle approach. It is difficult to tell if the needle tip is indeed inside the intermuscular plane. Figure C shows injection of a small amount of fluid (“hydro dissection”) to open up the narrow plane. A small hypoechoic fluid collection is now seen above the nerves. Retrieved on 12-10-2010 from www.usra.ca and content modified