Obstructive Sleep Apnoea
advertisement
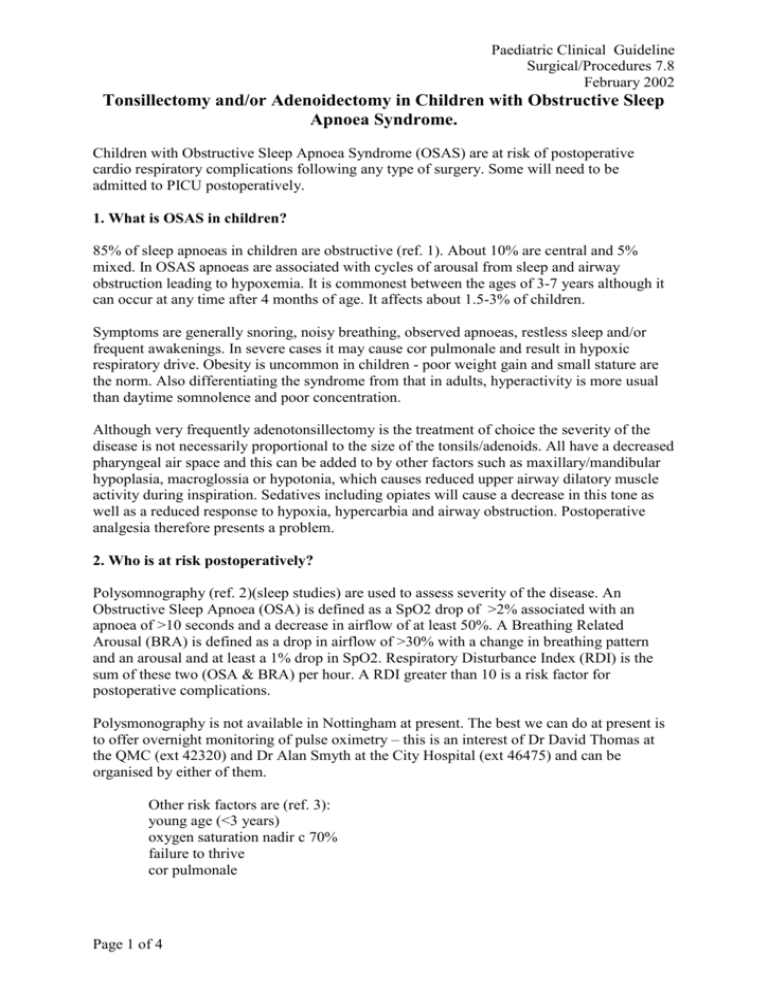
Paediatric Clinical Guideline Surgical/Procedures 7.8 February 2002 Tonsillectomy and/or Adenoidectomy in Children with Obstructive Sleep Apnoea Syndrome. Children with Obstructive Sleep Apnoea Syndrome (OSAS) are at risk of postoperative cardio respiratory complications following any type of surgery. Some will need to be admitted to PICU postoperatively. 1. What is OSAS in children? 85% of sleep apnoeas in children are obstructive (ref. 1). About 10% are central and 5% mixed. In OSAS apnoeas are associated with cycles of arousal from sleep and airway obstruction leading to hypoxemia. It is commonest between the ages of 3-7 years although it can occur at any time after 4 months of age. It affects about 1.5-3% of children. Symptoms are generally snoring, noisy breathing, observed apnoeas, restless sleep and/or frequent awakenings. In severe cases it may cause cor pulmonale and result in hypoxic respiratory drive. Obesity is uncommon in children - poor weight gain and small stature are the norm. Also differentiating the syndrome from that in adults, hyperactivity is more usual than daytime somnolence and poor concentration. Although very frequently adenotonsillectomy is the treatment of choice the severity of the disease is not necessarily proportional to the size of the tonsils/adenoids. All have a decreased pharyngeal air space and this can be added to by other factors such as maxillary/mandibular hypoplasia, macroglossia or hypotonia, which causes reduced upper airway dilatory muscle activity during inspiration. Sedatives including opiates will cause a decrease in this tone as well as a reduced response to hypoxia, hypercarbia and airway obstruction. Postoperative analgesia therefore presents a problem. 2. Who is at risk postoperatively? Polysomnography (ref. 2)(sleep studies) are used to assess severity of the disease. An Obstructive Sleep Apnoea (OSA) is defined as a SpO2 drop of >2% associated with an apnoea of >10 seconds and a decrease in airflow of at least 50%. A Breathing Related Arousal (BRA) is defined as a drop in airflow of >30% with a change in breathing pattern and an arousal and at least a 1% drop in SpO2. Respiratory Disturbance Index (RDI) is the sum of these two (OSA & BRA) per hour. A RDI greater than 10 is a risk factor for postoperative complications. Polysmonography is not available in Nottingham at present. The best we can do at present is to offer overnight monitoring of pulse oximetry – this is an interest of Dr David Thomas at the QMC (ext 42320) and Dr Alan Smyth at the City Hospital (ext 46475) and can be organised by either of them. Other risk factors are (ref. 3): young age (<3 years) oxygen saturation nadir c 70% failure to thrive cor pulmonale Page 1 of 4 Paediatric Clinical Guideline Surgical/Procedures 7.8 February 2002 neuromotor disease (hypotonia, cerebral palsy, seizures) craniofacial abnormalities (Down’s syndrome, achondroplasia) chromosomal abnormalities history of prematurity recent respiratory infection obesity (All the above at risk children should be admitted to PICU postoperatively for observation.) 3. Investigations 3.1 All children: FBC (? polycythaemia) ECG (?RVH/cor pulmonale (rare)) SpO2 at rest. It is good practice to carry out oximetry studies in all children. (see note earlier re Drs David Thomas (QMC) and Alan Smyth (City) who are willing to carry out these studies) NB no need for arterial gases! If RAH or RVH on ECG then a CXR (? Heart size; ?pul. oedema) If RVH then Echo (?RV function) Refer to cardiologist if ?pul HT. 3.2 Children with disturbed sleep: Polysomnography to: Assess number of episodes per hour Clarify diagnosis 4. Anaesthetic Management 4.1 Assessment: Sleeping habit and snoring history Hct; ECG; SpO2 If RVH or chronic low SpO2 then further investigations as above. 4.2 Premedication No sedation ?? antisialogues 4.3 Induction Anticipate difficult intubation if craniofacial abnormalities Anticipate cardiac decompensation if RVH Standard monitoring Preoxygenate if possible Inhalational induction with Sevoflurane (esp. if difficult airway) Tracheal intubation under deep Sevoflurane (or relaxant if no difficulty with ventilation) IPPV (deep volatile/SV causes respiratory and myocardial depression and potentially failure) Page 2 of 4 Paediatric Clinical Guideline Surgical/Procedures 7.8 February 2002 4.4 Analgesia (NB this section is to be used in theatre - anaesthetic management - not paediatric management): Paracetamol 30-45mg/kg pr to a maximum of 90mg/kg/day NSAIDS if platelet count normal (Brufen/Voltarol) Avoid opiates if possible but: codeine 1mg/kg im/pr is next stage ?morphine (up to 0.1mg/kg iv) in theatre, recovery or on PICU with close monitoring ?? laryngeal airway to pharynx (but loss of sensation can risk airway obstruction) 4.5 Extubation: Extubate light, fully reversed, on side, slightly head down in case of bleeding. If not in at risk group (see above) then no need for intensive postoperative monitoring. Normal postoperative TPR hourly decreasing to 4 hourly when stable. 5.0 Intensive postoperative monitoring if in at risk group: 1:2 nurse: patient ratio preferably on PICU. NB It is our policy for a medical escort to return with the patient to PICU 5.1 Monitor: respiratory rate respiratory effort (?obstruction) End tidal PCO2 (?obstruction) SpO2 Inspired oxygen concentration ECG NB Most improve over several days. Need to be kept on PICU for 12 hours at least – preferably 24 hours A J Matthews Monday, 25 June 2001 Revised Monday, 19 November 2001 References 1. Obstructive sleep apnoea syndrome in children. Warwick JP and Mason DG. Anaesthesia 1998, 53, 571-579. 2. Postoperative respiratory compromise in children with obstructive sleep apnea syndrome: can it be anticipated? Rosen MD et al. Pediatrics 1994, 93, 784-788. 3. Cardio respiratory sleep studies in children. Establishment of normative data 4and polysomnographic predictors of morbidity. American Thoracic Society. Am J Resp Crit Care Med 1999, 160, 1381-1387. Page 3 of 4 Paediatric Clinical Guideline Surgical/Procedures 7.8 February 2002 PAEDIATRIC CLINICAL GUIDELINES ISSUE: VERSION: FINAL Title: Sleep Apnoea guideline Author: Job Title: Dr Andy Matthews Consultant Paediatric Anaesthetist First Issued: Date Revised: February 2002 Review Date: February 2005 Document Derivation: i.e. References: Consultation Process: Included in document Ratified By: Paediatric Clinical Guidelines Committee Chaired By: Consultant with Responsibility: Dr Stephanie Smith Distribution: Training issues: All wards QMC and CHN Included in Induction Programme Audit: This guideline has been registered with Nottingham City Hospital NHS Trust and QMC Clinical Guidelines Committee. However, clinical guidelines are ’guidelines’ only. The interpretation and application of clinical guidelines will remain the responsibility of the individual clinician. If in doubt contact a senior colleague or expert. Caution is advised when using guidelines after the review date. MANUAL AMENDMENTS RECORD (please complete when making any hand-written changes/ amendments to guideline and not processed through guideline committee) Date Page 4 of 4 Author Description