Response to Reviewers MS: 5790191321126825 Risks of
advertisement

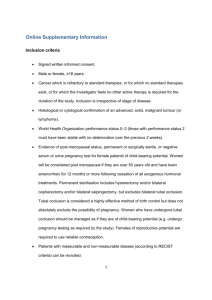
Response to Reviewers MS: 5790191321126825 Risks of Postoperative Paresis in Motor Eloquently and Non-Eloquently Located Brain Metastases Thomas Obermueller, Michael Schaeffner, Julia Gerhardt, Bernhard Meyer, Florian Ringel and Sandro M Krieg REVIEWER COMMENTS TO AUTHOR: Reviewer #1 Dear Professor Schaller, Thank you for your important comments. We carefully revised our manuscript according to your input. Concerns: Concern 1: It is not clear from the manuscript, if their patient series included patients with single cerebral metastases only - and if so, of which size. The presence of multiple metastases may have influenced the outcome, and the inclusion of small single metastases should have triggered a reflex toward radiosurgical treatment as an option as well. Answer: As outlined in table 1, 57% and 56.7% of all patients suffered from single brain metastases (page 27). Unfortunately, we do not have data on tumor size. In our hospital all patients with cerebral metastases are discussed in an interdisciplinary tumor board (neurosurgeons, medical oncologists, radiation oncologists) and surgery is only indicated in consent with this board (page 5). Concern 2: The term "eloquent" doesn't apply to motor function only. They use this term as synonymous with lesions located in motor regions only. Answer: You are right. We therefore changed this term to „motor eloquent“ throughout the manuscript as already mentioned in the title. Concern 3: How come that the rate of new motor deficits in patients with non-eloquently located metastases is similarly high as in those located in motor regions. They should try to explain - maybe on the basis of the postoperative MRI studies in their patients. What is the meaning of coining a term "eloquent" for motor location if there is no difference to the non-eloquently located lesions? Answer: You are right. But as shown in Fig. 4, there is a trend towards a higher deficit rate in motor eloquently located metastases (page 25). We evaluated all postoperative MRI scans in our patients. On page 14 and 15 we tried to explain the similar deficit rates with these data and wrote: „In the motor eloquent group, four patients suffered secondary hemorrhages causing permanent motor deficits. Ischemia only occurred in one case. When operating especially near or within the rolandic cortex, our department rarely uses the bipolar cautery, to avoid consecutive ischemia. Even in the non-motor-eloquent group, we had two cases of new permanent motor deficits (1.3%) after surgery due to ischemia and secondary hemorrhage. This tells us that even such tumors carry the risk of postoperative paresis, and we have to bear this fact in mind when we counsel our patients.“ Concern 4: How do they explain the high rate of residual tumor? This is a very surprising finding. Don't they adhere to the principle that resection of metastases should include aspiration of surrounding tissue whenever possible (as "supramarginal resection" in gliomas)? Are they changing their habits now? Could intraoperative fluorescence help to improve? Would they propose their patients to be taken back to the OR, as one does in case of residual tumor following glioma surgery, because extent of resection translates in survival clearly? Answer: We do not perform routine supramarginal resections of metastases. On page 13 we provide an explanation for our high rate of residual tumor. One explanation could be the two cited recent studies, which provided some data that metastases might have an infiltrative growth pattern (Kamp MA, Dibue M, Santacroce A, Zella SM, Niemann L, Steiger HJ, Rapp M, Sabel M: The tumour is not enough or is it? Problems and new concepts in the surgery of cerebral metastases. Ecancermedicalscience 2013, 7:306; Baumert BG, Rutten I, Dehing-Oberije C, Twijnstra A, Dirx MJ, DebougnouxHuppertz RM, Lambin P, Kubat B: A pathology-based substrate for target definition in radiosurgery of brain metastases. Int J Radiat Oncol Biol Phys 2006, 66(1):187-194). On the other hand, residual tumor in this study was defined as any case of contrast enhancement, which can therefore result in considerable overestimation of real residual tumor due to reactive postoperative changes. But you are right: intraoperative imaging or repeated resection have to be discussed and we added this important issue to the discussion section (page 14). Concern 5: On p14 "small lung cancer" should become "small cell lung cancer". Answer: This was changed on page 14. Reviewer #2 Dear Professor Duffau, Thank your for your review. We think that your comment increased the value of our manuscript significantly. Minor essential revisions However, the authors should be cautious by speaking about "non-eloquent areas". Indeed, they did not take into consideration language or visual functions: how many metastasis involved the left dominant hemisphere? It seems that 15.3% of tumors were located in the occipital lobe, but the rate of visual filed deficit was not given, etc... Answer: You are right. As mentioned in the title we strictly analyzed motor function. However, this was not clearly mentioned in the manuscript. We therefore changed „eloquent“ to „motor eloquent“ throughout the manuscript.