PERIPHERAL NERVE
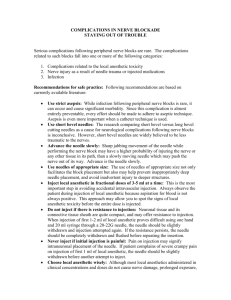
advertisement

LOWER EXTREMITY PERIPHERAL NERVE BLOCKS Compared to upper extremity, the lower extremity nerve blocks are technically more challenging because: Two plexuses (Lumbar and Sacral) supply innervation to lower extremity versus one (Brachial plexus) to upper extremity The neural elements are widely separated so one injection technique (as in upper extremity) does not provide complete block at the extremity. The plexuses lie deep under thick muscles more difficult to access than brachial plexus. Multiple nerves needs to be blocked for satisfactory anesthesia/analgesia. Advantages of peripheral peripheral nerve blocks: Advantages over general and central neuroaxial blocks are: i. Unilateral block of long duration ii. Ambulation with crutches possible. iii. No autonomic blockade, therefore: • No hemodynamic instability • No voiding difficulty iv. Minimal side effects – Nausea/vomiting, somnolence, Respiratory depression. Femoral Nerve Block OVERVIEW: Indications: Anterior thigh and knee surgery, below knee surgery in conjunction with sciatic nerve block, most reliable way to block saphenous nerve. Landmarks: Groin crease, femoral artery pulse. Nerve stimulation: Quadriceps twitch with patellar snap at 0.2-0.5 mA. Local anesthetic: 10 ml sufficient for femoral nerve block, 30-40 ml for ‘3-in-1’ block. ANATOMY: The femoral nerve (L2,3,4) emerges from the psoas muscle in a fascial compartment between the psoas and iliacus muscles . It enters the thigh posterior to the inguinal ligament. There it lies lateral and posterior to the femoral artery. This relationship to the femoral artery exists near the inguinal ligament, but not after the nerve enters the thigh. As the nerve passes into the thigh, it divides into an anterior and a posterior division and quickly arborizes. At the level of the inguinal ligament, there are dense fascial planes, the fascia lata, and fascia iliaca. The femoral nerve is situated deep to these fascial planes. The femoral artery, vein, and lymphatics reside in a separate fascial compartment medial to the nerve. The femoral nerve supplies the skin over the anterior surface of the thigh. It supplies motor innervation to the quadriceps muscle and the knee joint. The saphenous nerve, which is a branch of the femoral nerve, supplies the medial part of the calf down to the medial malleolus. Femoral nerve divides within 2 cm of of passing under the inguinal ligament. Also note that it is covered by fascial lata and fascia iliaca. Also note that femoral vessels and nerve lie in distinctly separate compartments. PROCEDURE: The patient is placed in the supine position. Femoral artery is palpated at the level of groin crease. With the fingers on the femoral artery a skin wheal is raised 1 cm lateral to the pulsations. A 5-cm nerve block needle is inserted through this wheal, and advanced cephalad at an angle of 45 to skin, looking for quadriceps twitch with patellar snap. Nerve stimulator is set to deliver an initial stimulus at 1-1.5 mA, which is gradually reduced while maintaining a twitch response. Goal is to maintain twitch at 0.5 mA., at which point local anesthetic is incrementally injected. The point of needle entry is 1 cm lateral to the femoral artery pulse, in the groin crease. Advance the needle cephalad, at an angle of 60 to skin, looking for patellar snap at < 0.5 mA. NEEDLE ADJUSTMENT: No response: redirect the needle by 10-15 in lateral direction. If still no response, move insertion point 0.5 cm more lateral. Sartorius contraction suggests stimulation of anterior division of femoral nerve. Withdraw the needle, reinsert 2-3 mm laterally to get posterior division in most cases. If lateral adjustment of needle tip does not get desired response, the posterior division may lie deep to anterior division. Withdraw the needle and reinsert with needle tip tilted medially to access posterior division. Muscle contraction and slight flexion of thigh suggests needle tip too deep – stimulation of iliopsoas muscle. Proximal sartorial contraction (just below anterior superior iliac spine) suggests needle tip too lateral lying in the sartorius muscle. Vascular puncture: needle too medial. Withdraw, reinsert 1-1.5 cm lateral to the initial point of insertion. CHOICE OF LOCAL ANESTHETIC: 10 ml of appropriate loal anesthetic (see below) is sufficient if only femoral nerve block is desired, 30-40 ml used for ‘3-in-1’ block. The choice of anesthetic depends on whether the objective is surgical anesthesia or postoperative analgesia. Avoid use of long acting drugs in ambulatory patient undergoing minor procedures as ambulation is affected by prolonged motor block of quadriceps muscle. SUGGESTED LOCAL ANESTHETIC AGENTS: Chloroprocaine 3%: 1 h anesthesia, 2 h analgesia Lidocaine or mepivacaine, 1.5-2%: 2-3 h anesthesia, 3-5 h analgesia, effect prolonged by addition of epinepherine. Ropivacaine 0.5%: 4-8 h anesthesia, 5-12 h analgesia Bupivacaine or l-bupivacaine 0.5%: 5-15 h anesthesia, up to 30 h analgesia Fascia Iliaca Block: OVERVIEW: Indications: Alternative approach to ‘3-in-1’ block. Typically used for postoperative analgesia. Landmarks: ASIS and pubic tubercle. Nerve stimulation: Typically not used. Local anesthetic: 30-40 ml. This blocked is used mainly for postoperative pain relief. Performance of this nerve block does not require a nerve stimulator. The block is performed at a point where there are no major vessels or nerves, but the local anesthetic diffuses to the femoral nerve and lateral femoral cutaneous nerves to provide pain relief PROCEDURE: The patient is placed in supine position. A line is drawn connecting ASIS and pubic tubercle. This line is trisected, and the junction of lateral and middle thirds is marked. Point of needle insertion is 2 cm caudad to this point. A blunt needle (17-20g Tuohy, or a pencil tip spinal needle) is advanced at 45-60 to the skin in a cephalad direction. 2 distinct pops are felt, as the needle is advanced. The first is the fascia lata and the second, often a more subtle ‘pop’, is the fascia iliaca. After this second, loss of resistance, the needle is advanced another half centimeter and firm distal pressure is applied to the leg to encourage rostral spread of the local anesthetic. The syringe is aspirated, and then 20-30 ml of local anesthetic is incrementally injected with aspiration. Trisect inguinal ligament. Needle entry site is 2 cm distal to the junction of middle and lateral third of above line. (also 1.5-2 cm lateral to femoral A). A blunt tip needle gives a discernible pop as the fascia lata, then the fascia iliaca, is traversed. NEEDLE ADJUSTMENT: If no clicks felt: use blunter needle. It may also help if you make small side-to-side oscillations as you advance the needle. CHOICE OF LOCAL ANESTHETIC: 30-40 ml. Identical to ‘3-in-1’ block Lateral Femoral Cutaneous Nerve Block- L2-3 OVERVIEW: Indication: Surgery/pain on lateral side of thingh/knee.. Landmarks: Anterior superior iliac spine. Nerve stimulation: Typically not used as it is pure sensory nerve. Can be used by eliciting paresthesia percutaneously at 5 mA. Local anesthetic: 15-20 mL. ANATOMY: The lateral femoral cutaneous nerve of the thigh is a sensory nerve (no motor component) and supplies the anterolateral and lateral aspect up to the middle of the thigh. It also provides a branch to the patella. This nerve pierces the fascia lata 3-4 cm below the inguinal ligament to innervate the lateral side of the skin of the thigh. PROCEDURE: A skin wheal is raised 2 cm medial and 2 cm inferior to the anterior superior iliac spine. A 22 g.. 3” needle is introduced superiorly and laterally through the skin wheal and toward the iliac crest until the needle approaches the inner side of the iliac crest. A fanwise injection of 5-7 ml of local anesthesia is performed in this area. Anesthesia of the lateral aspect of the thigh down to the knee area results from this block. Needle is insertect 2 cm. medial and 2cm. inferior to anterior superior iliac spine, and fan-wise injection is made in superior and lateral direction. Higher success is claimed when a nerve stimulator is used to locate the nerve by eliciting paresthesia in lateral thigh and knee area. 5 6 Lumbar Plexus Block (Psoas Compartment Block): OVERVIEW: Indications: Hip, anterior thigh, knee surgery; Landmarks: Iliac crest, posterior superior iliac spine (PSIS). Nerve stimulation: Twitch of the quadriceps muscle at 0.5-0.7 mA. Local anesthetic: 25-35 mL. The psoas compartment block is a deep block of lumbar plexus from posterior approach. It generally provides consistent anesthesia in the distribution of all three elements of ‘3-in-1’ block, namely femoral, LCFN, and obturator nerve. Thus, it provides anesthesia or analgesia to the entire distribution of the lumbar plexus, including the anterolateral and medial thigh, knee, and the saphenous nerve below the knee. When combined with a sciatic nerve block, anesthesia of the entire leg can be achieved. Due to the placement of the needle in the deep muscle beds, the potential for systemic toxicity is greater than in many other techniques. In addition, the proximity of the lumbar nerve roots and epidural space carries a risk of an epidural spread. For these reasons, care should be taken when selecting the type, volume, and concentration of local anesthetic, particularly in elderly and frail patients. In addition, due to the depth of the needle placement, this block is best avoided in very obese patients. ANATOMY: Lumbar plexus is derived from anterior primary rami of L1-4 with a variable contribution from T12. The plexus lies within the substance of psoas muscle, and gives off six branches. Only the distal branches are important for lower extremity: Proximal Branches: 1. Iliohypogastric (T12-L1) 2. Ilioinguinal (T12-L1) 3. Genitofemoral (L1-2) Distal Branches: 1. Femoral (L2-4) 2. Lateral femoral cutaneous (L2-3) 3. Obturator (L2-4) Lumbosacral plexus. Anatomic depiction of the lumbosacral plexus with the major peripheral nerves of the lower extremity. 7 Psoas compartment block. (A) The sensory distribution of a psoas compartment block is shown on the right. The osteotomes blocked by the psoas compartment block are shown on the left. (B) Landmarks for the psoas compartment block. Intercrestal lime and a paramedian line passing through PSIS are drawn. Point of intersection of these lines is the point of needle isertion. (C) Psoas compartment deep landmarks observed from above. Post, posterior; Ant, anterior. (D) Psoas compartment block, final needle placement. Note the structures deep to the lumbar plexus including major vascular structures, kidneys, and abdominal contents. PROCEDURE: The patient is placed in lateral position with operative side up. Intercrestal lime and a paramedian line passing through PSIS are drawn. Point of intersection of these lines is the point of needle isertion. A 10-cm nerve block needle (21 OR 22 g for single injection, 18 g for catheter insertion) is advanced perpendicular to skin until it contacts transverse process, usually at a depth of 4-6 cm. The needle is then redirected cephalad or caudad to the transverse process, and advanced, usually no more than 2 cm further, while seeking a quadriceps twitch. If the twitch can be maintained to current level between 0.5-1 mA, 25-35 ml of local anesthetic is injected with frequent aspirations. If a catheter is inserted, bevel of the needle should be oriented down sheath. 8 NEEDLE ADJUSTMENT: Local paraspinal muscle twitch: needle too shallow stimulating paraspinal muscles, insert needle deeper. No response: withdraw the needle and redirect 5-10 cephalad or caudad. If still no response: move needle isertion point 0.5 cm medial. Caution: medial angulation increase risk of epidural spread. Contration of upper thingh: iliopsoas stimulation from a needle already within substance of psoas muscle. Further advancement of needle risks penetration through anterior surface of psoas & into adjacent structures. Withdraw needle and start again. Hamstring stimulation: needle is stimulating roots of sacral plexus which lies inferomedially to lumbar plexus. Withdraw needle to skin & re-direct needle supero-laterally to initial pass. SAFETY TIPS: The depth of needle insertion is extremely important because several complications can result from excessive needle depth. The distance from skin to lumbar plexus vary with patient’s body habitus, mean values being about 8.5 cm for men and 7 cm for women. The distance from transverse process to the lumbar plexus is extremely consistent at less than 2 cm. To ensure the proper position of the needle and avoid excessive needle insertion, it is highly recommended that the trnasverse process be intentionally sought . Lumbar plexus block carries a higher risk of local anesthetic toxicity due its deep location and vicinity of muscles. Avoid high concentrations of long-acting local anesthetic with this block. Epidural spread occurs in 9-16% of adult and >95% pediatric patients. Total spinal anesthesia has also been reported. Vigilance must be maintained to guard against this complication. Retroperitoneal hematoma is a rare complication, and it can be easily missed early in its course. ASRA guidelines should be followed while considering this block for patients who may be candidates for thromboprophylaxis. CHOICE OF LOCAL ANESTHETIC: Lumbar plexus blockade requires a relatively large volume of local anesthetic to achieve anesthesia of the entire plexus. Due to highly vascular nature of the area, epinephereine can be added to the local anesthetic as a marker for inadvertent intravascular injection. SUGGESTED LOCAL ANESTHETIC AGENTS: Smaller volumes and concentrations can be used successfully for analgesia (e.g., 20 ml of 0.25% bupivacaine); however, surgical anesthesia requires larger volumes, typically 3035 ml of more concentrated solution. Lidocaine or mepivacaine, 1.5-2%: 2-3 h anesthesia, 3-5 h analgesia, effect prolonged by addition of epinepherine. Ropivacaine 0.5%: 3-5 h anesthesia, 5-12 h analgesia Bupivacaine or l-bupivacaine 0.5%: 4-6 h anesthesia, 12-18 h analgesia Consider using a less toxic local anesthetic (2% chloroprocaine) or lower concentration (0.5% lidocaine) for skin infiltration to avoid a large cumulative dose of local anesthetic. 9 The Sciatic Nerve Block, Classic Labat Approach OVERVIEW: Indication: Surgery on knee, or below the knee. Landmarks: Greater tronchater (GT), PSIS, and sacral hiatus Nerve stimulation: Hamstrings, calf, foot, or toes twitch at 0.2-0.5 mA Local anesthetic: 15-20 mL. ANATOMY: The nerve becomes superficial at the lower border of the gluteus maximus muscle. The sciatic nerve exits the thigh between the greater trochanter and the ischial tuberosity. It is motor to the hamstring muscles and all muscles below the knee. The sciatic nerve supplies sensory innervation to the posterior thigh and entire leg and foot from just below the knee except for medial aspect, which is supplied by saphenous nerve. The nerve lies beneath a point 5 cm caudad along the perpedicular line that bisects the line joining PSIS and greater trochanter. The point of needle insertion should lie along a third line drawn between the greater trochanter and the sacral hiatus. PROCEDURE: The patient is placed in the lateral position, with the operative side nondependent. The operative extremity is flexed 45 at the hip and 90 at the knee and rests against the dependent lower extremity. PSIS and superior aspect of greater trochanter are identified and a line is drawn connecting the two points. This line is bisected. A perpendicular is dropped inferiorly 35 cm from the midpoint of this line to the point of needle insertion. The point of needle insertion should lie along a third line drawn between the greater trochanter and the sacral hiatus. A 10-15 cm nerve block needle is advanced perpendicular to the skin. Stimulation 10 intensity is initially set at 1.5 mA and adjusted downward as the evoked motor response increases. Optimum needle position would be associated with a twitch response maintained down to current level of 0.2-0.5 mA. As the needle is advanced, twitches of the gluteal muscles are observed first. These twitches merely indicate that the needle position is still too shallow. Once the gluteal twitches disappear, brisk response of the sciatic nerve to stimulation is observed (hamstrings, calf, foot, or toe twitches). This typically occurs at a depth of 5-8 cm. Since the nerve trunk is large, onset time and efficacy may be improved by injecting local anesthetic in more than one location, such as both laterally (peroneal component) as well as medially (tibial component). After negative aspiration for blood, 15-20 ml of local anesthetic is slowly injected. NEEDLE ADJUSTMENT: No response: redirect needle by 15° increment If no piriformis response (subtle contraction like a ripple under the skin) is seen, adjust insertion point by 1 cm back along perpendicular. Hamstrings rather than foot twitch: acceptable. Inject local anesthetic. Aspiration of blood: superior & inferior gluteal lie on either side of sciatic nerve - does not help with identification process. If patient complains of 'electric shocks’ in the penis or vagina area: Pudental nerve stimulation which lies medial to sciatic. Redirect needle more laterally. CHOICE OF LOCAL ANESTHETIC: This is a low volume block, and the duration of this block is longer than any other peripheral nerve block. Therefore, addition of epinepherine to local anesthetic is seldom necessary. Moreover, epinepherine may increase the risk of nerve injury. SUGGESTED LOCAL ANESTHETIC AGENTS: Chloroprocaine 3%: 2 h anesthesia, 2.5 h analgesia Lidocaine or mepivacaine, 1.5-2%: 4-5 h anesthesia, 5-8 h analgesia Ropivacaine 0.5%: 6-12 h anesthesia, 6-24 h analgesia Bupivacaine or l-bupivacaine 0.5%: 8-16 h anesthesia, up to 48 h analgesia Bupivacaine 0.25%: excellent for analgesia, duration almost as long as with 0.5% 11 Sciatic Nerve Block, Supine (Raj) approach: PROCEDURE: The patient is placed in the supine position; the hip is flexed to 90° and the knee to 90° . The leg can be placed on a padded stand to maintain this position. Greater trochanter, and ischial tuberosity are identified. Midpoint between these two, somewhat closer to the ischial tuberosity, is the point of needle insertion. A 10-15 cm nerve block needle is inserted through this point and advanced perpendicular to the skin, parallel to the floor. Stimulation intensity is initially set at 1.5 mA and adjusted downward as the evoked motor response increases. Stimulation of tibial (plantar flexion, inversion) or common peroneal (dorsiflexion, eversion) is acceptable response. At this level, the branch to hamstring may have already separated from the sciatic nerve, and therefore, hamstring twitch is not a reliable sign of sciatic stimulion. 15-20 ml of local Supine approach sciatic nerve block. Needle is inserted anesthetic is injected.. between ischial tuberosity and greater trochanter and advanced. Needle is kept parallel to table. NEEDLE ADJUSTMENT: No motor response: ‘Fan’ in a plane parallel to the floor. Still no response: Re-insert needle 1-3 cm caudal to the initial point of insertion.. CHOICE OF LOCAL ANESTHETIC: Same as for classic approach described above. 12 Sciatic Nerve Block, Anterior Approach: OVERVIEW:: Indications: Alternative approach when lower extremity cannot be moved Landmarks: ASIS, pubic tubercle, greater troachanter (GT) Nerve stimulation: Foot or toe twitch at 0.5 mA. Local anesthetic: 15-20 ml PROCEDURE: A line is drawn from ASIS to pubic tubercle. Another line is drawn parallel to this line from GT. A perpendicular line is dropped from the junction of medial ⅓rd and lateral ⅔rd of the first line to second line. The point of intersection of the perpendicular and the second line is the point of needle insertion. A 15-cm needle is inserted in a perpendicular fashion until it contacts the femur at the level of the lesser trochanter. The needle is then redirected off the femur in a more medial direction The needle is advanced 1-2 cm while stimulating until the maximal twitch response is obtained at the lowest current When the maximum twitches are obtained at the lowest current, 15-20 ml of local anesthetic is injected. A line is drawn from ASIS to pubic tubercle. Another line is drawn parallel to this line from GT. A perpendicular line is dropped from the junction of medial ⅓rd and lateral ⅔rd of the first line to second line. At the point of intersection, needle is inserted in a perpendicular fashion. NEEDLE ADJUSTMENT: Quadriceps stimulation: Needle too shallow, continue advancing the needle. Hamstring twitch: Unreliable, as it may indicate stimulation of branch to hamstring, or direct stimulation. Redirect needle medially or laterally. Needle deep but no bony contact or twitch: Needle probably too medial, redirect needle slight laterally. CHOICE OF LOCAL ANESTHETIC: as for classic approach described above. 13 Popliteal Block: OVERVIEW: Indication: Surgery on ankle or foot. Landmarks: Popliteal fossa crease, biceps femoris and semitendinosus tendons (prone approach); vastus lateralis and biceps femoris tendons for the lateral approach.. Nerve stimulation: Foot or toe twitch at 0.2-0.5 mA. Local anesthetic: 30-40 ml. ANATOMY: The popliteal block is a block of the sciatic nerve at the level of the popliteal fossa. The popliteal fossa is bounded medially by semtendinosus and semimembranosus muscles and laterally by biceps femoris muscle. The sciatic nerve divides into its tibial and peroneal nerves about 5-12 cm proximal to the level of popliteal crease. Tibial nerve, the larger of the two divisions, runs in the middle of popliteal fossa and passes inferiorly though two heads of gastrocnemius muscle. Peroneal nerve follows tendon of biceps femoris along the lateral margin of popliteal fossa. The sciatic nerve in the popliteal fossa is about midway between the skin and the bone. It is lateral and superficial to the popliteal artery and vein and it is not enveloped by the same tissue sheath (neurovascular sheath). Popliteal block can be performed in prone, lateral or supine position. PROCEDURE, PRONE POSITION: The patient is placed in prone position. Outlines of popliteal fossa - the inner borders of biceps femoris tendon laterally, and semitendinosus tendon medially are drawn . In obese patients, patient may be asked to flex the knee allowing the muscles to become prominent. The point of needle insertion is 7-10 cm superior to the popliteal crease, 1 cm lateral to a 14 point midway between the tendons of semitendinosus and biceps femoris. A 5-cm nerve block needle is advanced 60-90 to the skin. The nerve stimulator is set initially to 1.5 mA at 2 Hz, and foot/toe twitch is sought which can be maintained to current level of 0.2-0.5 mA.. In patients with neuropathy, it may be difficult to obtain twitch response at low current. Once appropriate twitch response is obtained, 30-40 ml of local anesthetic is incrementally injected. PROCEDURE, LATERAL POSITION: The patient is placed in supine position and knee is flexed by placing pillow under the calf. Upper border of patella is marked and line is extended laterally. The groove between the tendon of Biceps femoris and Vastus lateralis is marked. Asking the patient to flex the knee against resistance on calf muscle will make the groove prominent. The point of needle entry site is at the junction of the groove and patellar line, and is about 7 cm proximal to knee crease. A 10-cm nerve block needle is advanced until its tip encounters the femur. If no contact is made, the needle entry site is moved up towards patella. Once the femur is contacted, the needle is withdrawn and redirected 20°-30° posteriorly. Foot (not calf muscles) twitch is sought – Inversion, eversion, plantar or dorsiflexion. Once appropriate twitch response is obtained, 30-40 ml of local anesthetic incrementally injected. NEEDLE ADJUSTMENT: Local twitch of vastus lateralis: Point of insertion too anterior. Withdraw, and reinsert needle posteriorly Contraction of biceps femoris suggests needle tip is too shallow and posterior. Vascular puncture: Needle too deep and anterior. Redirect posteriorly. 15 CHOICE OF LOCAL ANESTHETIC: This is a high volume block (30-40 ml). Lower volumes may be sufficient if the two branches are individually stimulated. The choice of anesthetic depends on whether the objective is surgical anesthesia or postoperative analgesia. SUGGESTED LOCAL ANESTHETIC AGENTS: Chloroprocaine 3%: 1 h anesthesia, 2 h analgesia Chloroprocaine with epinepherine: 1.5-2 h anesthesia, 2-3 h analgesia Mepivacaine 1.5%: 2-3 h anesthesia, 3-5 h analgesia Mepivacaine 1.5% or lidocaine 2% with epinepherine: 2-5 h anesthesia, 3-8 h analgesia. Ropivacaine 0.5%: 4-8 h anesthesia, 5-12 h analgesia Bupivacaine or l-bupivacaine 0.5%: 5-15 h anesthesia, up to 30 h analgesia Bupivacaine 0.25%: excellent for analgesia, duration almost as long as with 0.5% Ankle Block OVERVIEW: Indication: Surgery on foot. Landmarks: Medial and later malleoli, posterior and anterior tibial arteries, extensor hallucis tendon. Nerve stimulation: Typically not used Local anesthetic: 20-30 ml. ANATOMY: An ankle block involves blocking the five nerves that provide innervation below the ankle. The Deep Peroneal Nerve: Lies adjacent to the anterior tibial artery on the anterior surface of the distal tibia at the level of the malleolus, lateral to the tendon of the extensor hallucis longus. The Sural Nerve: Descends on the lateral aspect on the ankle midway between the lateral malleolus and the calcaneous toward the lateral side of the small toe. The Saphenous Nerve: This is a branch of the femoral nerve, it rnns~in the superficial fascia in front of the malleous, innervates the medial side of the foot. Superficial Peroneal Nerve: Lies in a superficial fascia and divides into branches supplying the dorsum of the foot and toes between the areas supplied by the sural nerve and deep peroneus nerves. Posterior Tibial Nerve: Lies between the medial malleous and the tendon achilles on the medial aspect of the ankle under the flexor retinaculum. Lies posterior to the pulsation of the posterior tibial artery. It innervates the skin and muscle of the plantar aspect of the foot. 16 Ankle block anatomy. Posterior tibial nerve is blocked between medial malleoltis and Achilles tendon. Sural nerve is blocked lateral to Achilles tendon. Landmarks The major landmarks for the ankle block are the medial and lateral malleoli. Ankle block. (A) Block of deep peroneal and saphenous nerves. (B) Block of superficial nerves. These nerves are very superficial and are blocked by infiltrating skin 17 Sural nerve and posterior tibial nerve block Deep Peroneal Nerve Block Landmarks Extensor hallucis longus tendon- at level of medial and lateral malleoli Anterior tibial artery- at level of medial and lateral malleoli Procedure A skin wheal is raised on anterior aspect of the ankle lateral to the extensor hallucis longus tendon at the area of the pulsation of the anterior tibial artery. A 25 ga. needle is inserted through this wheal and it is directed in a perpendicular fashion until it hits the bone. Inject 5 ml of local anesthetic after aspiration. Do not use epinephrine. Superficial Peroneal Nerve The superficial peroneal nerve is blocked by laying a wall of anesthesia in the subcutaneous tissue in a medial and lateral dicection from the site of the injection of the deep peroneal nerve. Sural Nerve A skin wheal is raised midway between the lateral malleolus and the calcaneous. Through this wheal a needle is passed and 5 ml of local anesthetic solution are injected in the skin between the lateral malleous and calcaneous. Saphenous Nerve A skin wheal is raised in the area of the medial malleolus. Through this wheal a needle is passed subcutaneously and 5 ml of local anesthetic solution are injected around the great saphenous vein in front of the medial malleous. 18 NOTE: All the superficial nerves can be blocked by extending the anesthesia from the area of the deep peroneal nerve by placing a wall of anesthesia in a medial and lateral direction. Posterior Tibial Nerve A skin wheal is raised midway between the medial malleolus and the calcaneous adjacent to the tendon achilles. Through this wheal a needle is passed toward the pulsations of the posterior tibial artery. Twitching of the sole of the foot is detected when a nerve stimulator is used. 5-6 ml of local anesthetic solution is injected after careful aspiration. 19 References: 1. Enneking et al. Lower Extremity Peripheral Nerve Blockade: Essentials of Our Current Understanding. Reg. Anesth. Pain Med. 2005, 27:4-35 2. Bernstein RL, RosenbergAD; Manual of Orthopedic Anesthesia and Related Pain Syndromes. Churchill Livingstone 1994 3. www.nysora.com 20