8. Blood Vessels
advertisement

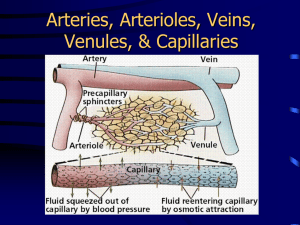
PHYSIOLOGY LECTURE OUTLINE The Vascular System: Control of Blood Flow and Pressure Blood Vessels Blood vessels are the 'tubes' that transport blood from the heart to the body and back again. All blood vessels contain an innermost lining called endothelium, a type of epithelial tissue. It plays an important role in regulating blood pressure, vessel growth and movement of substances into and out of vessels. All blood vessels except capillaries also contain vascular smooth muscle (VSM) in their walls. They can be arranged in circular or spiral layers. When they contract they cause vasoconstriction of the vessel, and when they relax they cause vasodilation of the vessel. These changes in blood vessel diameter have a significant impact on blood flow and blood pressure. Current research indicates that the various components of the wall of blood vessels play an active role in how the blood vessel behaves. The muscle cells of VSM are not electrically coupled (as in cardiac cells), so each muscle cell must be stimulated individually to contract. Graded contractions in VSM are achieved by gradual changes in membrane potential and their contraction depends on Ca2+ entry. There are both voltage-gated and chemically-gated Ca2+ channels in smooth muscle. VSM maintains a constant state of partial contraction, this is termed muscle tone. Many things, like neurotransmitters, hormones, paracrines, etc., affect muscle tone. Also, the endothelial cells of blood vessels can secrete vasoactive paracrines, factors that can alter vessel diameter and thus flow of blood. Briefly listed here are descriptions of the important blood vessels in the systemic circuit, going from arterial to venous systems: 1. Arteries: Thick walled (3 layers), elastic vessels for high pressure blood. 2. Arterioles: Resistance vessels, less elastic, more muscular, large changes in diameter. 3. Capillaries: Thinnest walled, smallest diameter vessels for exchange. Microcirculation 4. Venules: Drains capillaries, has endothelium and some VSM, participates in exchange. 5. Veins: Thinner walled (3 layers), large diameter vessels for returning low pressure blood back to heart. 1. Arteries Carry Blood away from the Heart Large arteries, like the aorta and other major arteries, are thick walled (3 layers), stiff and springy. They contain VSM with fibrous tissue and elastic tissue, so that they exhibit elasticity. They have 2 important roles: 1) they transport high pressure blood to the body; and 2) they help to maintain arterial pressure. The high-pressure blood in these vessels stretches the elastic fibers, and when pressure is reduced (as ventricles relax), they recoil to their original shape, thus not allowing the arterial pressure to fall too low before the next ventricular contraction begins. 2. Arterioles Arterioles are the Resistance vessels in the body. Their wall has only 2 layers (endothelium and VSM) and they can exhibit large changes in diameter due to the VSM. As we will see, even small changes in blood vessel diameter can cause significant changes in resistance to blood flow - which will impact blood pressure. Peripheral resistance is often defined as the resistance in arterioles (Rarterioles). As Rarterioles increases, the pressure gradient must also increase, in order to overcome this resistance. 2 3. Capillaries are the Vessels of Exchange Capillaries (and post-capillary venules) are where exchange of contents between blood and the tissues occur. The capillary walls are the thinnest of all vessels, made of flat endothelium that is only one-cell thick and supported on a basement membrane. There are leaky junctions between cells (except at the blood-brain barrier) to facilitate exchange. As we shall see later, there are different types of capillary beds in the body. Each has a slightly different arrangement to best suit its function. Blood flow through the capillaries is determined by a combination of the driving force mean arterial pressure (MAP) and the amount of resistance in the arterioles. The rate of blood flow within a single capillary bed is proportional to the MAP and inversely proportional to the resistance of the arteriole regulating flow into that capillary bed. See previous Cardiovascular notes regarding Flow = P/R. 4. Venules Blood flows from capillaries to venules. Small venules are distinguished from capillaries by convergent flow pattern, that is, they collect the blood exiting the capillary beds and become larger vessels. Venules have very thin walls and can participate in some exchange but some also have a little smooth muscle and are larger than capillaries in diameter. Venules drain into veins. 5. Veins Veins are similar to arteries in that their walls have 3 layers, but the walls of veins are thinner than arteries. Veins are more numerous than arteries and have larger diameter (despite having thinner walls). They hold more than 1/2 of the circulating blood and as such veins act as a volume reservoir, often termed the Venous Reservoir. Veins are where the pressure of blood is the lowest. Blood flows down a pressure gradient, so if blood is to flow from arteries > arterioles > capillaries > venules > veins, then each next vessel must have lower pressure then the previous, thus veins must be the lowest. By definition, veins transport blood back to the heart. Due to the low pressure in these vessels, there are some strategies that the venous system uses to help get blood back to the heart. Mechanisms to Increase Venous Return 1) Venous Valves: Veins have venous valves. As in the heart, vales in veins are to prevent retrograde flow of blood. The segmentation of veins with valves means that once the blood in the next compartment, it cannot drop back to the one before it. In this way, blood in veins "inches" back to the heart at low pressure (but because the diameters are large, the flow is relatively high). 2) Skeletal Muscle Pump: Many veins are situated next to skeletal muscle. When this muscle contracts, it compresses the veins nearby, and because of the valves in veins, the blood can only move 'up', toward the heart when these vessels are compressed. Therefore, muscle contraction helps augment venous return of blood to the heart. 3) Respiratory Pump: Breathing in and out requires contraction of the diaphragm (a skeletal muscle). When we breath in (diaphragm contracts) the pressure in the thoracic cavity decreases. This small decrease helps blood flow from the venae cavae (this term means both the inferior and superior vena cava) into the right atrium. When we breath out (diaphragm relaxes) the pressure in the thoracic cavity increases, so flow is slowed a little, but each breath in helps flow more than the out breath hinders flow. 3 BLOOD PRESSURE Ventricular contraction creates the driving force of blood pressure (BP). The elastic recoil of arteries helps to sustain the high pressure in these vessels (arteries) that push blood forward. Because they are located close to the ventricle and they are elastic, arteries are high-pressure vessels in which blood moves with a pulsatile flow. If a person has been cut and is bleeding, you can distinguish a cut artery from a cut vein by looking for uneven flow that reflects the pulse. The major arteries of the body are located deep inside the tissues, where they are protected from superficial trauma. In contrast, the many veins are closer to the surface of the body. Although you cannot see the major arteries, you can feel them wherever you can find a pulse. Major pulse points of the body include the carotid arteries, which are found in the neck on either side of the trachea, the femoral arteries, which are found in the groin area, the brachial arteries, which are found on the inside of the arms just above the elbow, and the radial arteries, which are found on the lateral side of the wrists. In these locations the arteries emerge closer to the body surface in order to cross bones. Blood Pressure in the Systemic Circulation is Highest in the Arteries and Lowest in the Veins Pressure decreases moving from arteries to veins due to blood pressure resistance. Veins have no pulse. Systemic pressure is maximum in the aorta. Blood Pressure (BP) is expressed as Systolic pressure (the higher value) over Diastolic pressure (the lower value). Typical normal values for a 70 Kg man are 120/80 (where systolic pressure = 120 mm Hg and diastolic pressure = 80 mm Hg). Pulse occurs from rapid pressure increase that occurs when ventricles push blood into aorta. Pulse amplitude decreases over distance due to friction. Pulse pressure can be defined as the measure of the change in amplitude of the pulse pressure wave - and can be calculated with this formula: Pulse Pressure = Systolic - Diastolic (in e.g., 120 - 80 = 40 mmHg). Arterial Blood Pressure Reflects the Driving Pressure for Blood Flow Arterial blood pressure is estimated by using sphygmomanometer. Briefly, the process is as follows: Inflating the cuff cuts off blood flow as it exceeds the pressure in the vessel. Gradually deflating the cuff allows pressure to begin to fall. When blood pressure in the vessel is greater than the cuff, blood flows past. Turbulent flow makes the Korotkoff sound. Systolic pressure is detected as the pressure at which blood flow is first heard, i.e., highest pressure. Diastolic pressure is detected as the pressure at which all sound disappears (lowest pressure). We may test for these sounds in lab. If we assume that arterial blood pressure reflects ventricular pressure and that arterial pressure is pulsatile, then measure of mean arterial pressure (MAP) gives a single value that represents the driving pressure. The formula for MAP is: MAP = Diastolic P + 1/3 (Systolic P - Diastolic P) For a person with BP of 120/80, MAP = 93 mm Hg. Use the above formula to calculate this value. This formula applies for people with a resting heart rate range of 60-80 beats per minute (bpm). The heart actually spends more time in diastole (relaxation) than in systole (contraction) and this formula for MAP reflects that. If it were a straight mean, it would be calculated as: (120 + 80) divided by 2 = 100 mmHg. Abnormally high or low arterial blood pressure can indicate problems. Low pressure may indicate impaired blood flow and oxygen delivery. High pressure (hypertension) may increase the risk of hemorrhage. 4 WHAT ARE THE MAIN FACTORS INFLUENCING MEAN ARTERIAL PRESSURE (MAP)? 1) Cardiac Output (C.O.) 2) Peripheral Resistance (Rarterioles) 3) Total Blood Volume 4) Distribution of Blood in Body 1) Cardiac Output Mean Arterial Pressure (MAP) is the major determinant of blood flow. Then what determines MAP? It is a balance between blood flow into and out of arteries. If the flow into arteries is greater than the flow out, then there is an increased MAP. If the flow out of arteries is greater than the flow in, then there is a decreased MAP. Most simply put, MAP is a function of cardiac output (CO) and resistance of arterioles (or peripheral resistance). Cardiac Output (CO) determines blood flow into arteries and peripheral resistance determines blood flow out (e.g., greater R, less flow out). 2) Peripheral Resistance (Resistance in the Arterioles) More than any other type of vessel, the arterioles are the main site of varying systemic resistance. The Vascular Smooth Muscle (VSM) in their walls allows for large changes in diameter. VSM contraction leads to vasoconstriction and VSM relaxation leads to vasodilation. Remember, R 1/r4. As the result of tonic sympathetic stimulation, all arterioles except those of the brain and lungs maintain a tonic state of contraction, in other words, they are always a little constricted. The ANS has control of blood vessel diameter through sympathetic stimulation that maintains vascular tone. To constrict vessels further, sympathetic stimulation is increased; to get dilation, there is a reduction in sympathetic stimulation. Arteriole resistance is also influenced by local control. These factors usually act to match tissue blood flow to tissue's metabolic needs. For example, if some tissues have low O2 content, then blood flow to that region will increase (vessels dilate) to supply the tissues using up their O2. Conversely, if tissues have adequate O2 levels, then blood flow may decrease (vessels constrict) to that region. Reflex (long distance) vasoconstriction and vasodilation by the ANS and hormones is superimposed on the tonic control to ensure that arterial blood pressure remains adequate. Clinical note: Most cases of hypertension are associated with increased peripheral resistance. 3) Total Blood Volume Changes in blood volume affect blood pressure. As blood volume increases, blood pressure increases. The converse is also true; As blood volume decreases, blood pressure decreases. Therefore, blood volume and blood pressure (BP) are directly proportional, if volume increases (and all else remains constant) then BP will also increase. How is blood volume controlled? Blood volume adjustments are primarily the responsibility of kidneys. For example, if you drink large amounts of water, this will increase blood volume. In response, the kidneys will act to excrete more water. This way, the volume is decreased and BP is reduced, the response from the kidneys is integrated with the cardiovascular system. Kidneys can only conserve water, they cannot create more water when you are dehydrated. Therefore if you have low blood volume, this lost fluid must be replaced by drinking or IV infusions. The cardiovascular system compensates if you are experiencing decrease blood volume: As you will see, increased sympathetic activity causes vasoconstriction. 5 4) Distribution of Blood in the Body Blood distribution to the tissue depends on metabolic needs and this is governed by a combination of local and reflex control. For example, at rest skeletal muscle gets 20% of cardiac output (CO); when exercising it gets 85%. The blood distribution depends partly on number and size of arteries feeding an organ. The kidneys, digestive tract, liver, and muscles together receive over 2/3 of the CO. Blood flow variations are possible because arterioles are arranged in parallel. Remember that total blood flow through all arterioles = CO. Flow through individual arterioles depends on their resistance. As resistance increases, blood flow decreases. Blood diverted from high-resistance arterioles flows through low-resistance arterioles -blood flow takes the path of least resistance. In other words, blood flows into dilated blood vessels more easily than constricted ones. Within a tissue, capillary blood flow can be regulated by pre-capillary sphincters. At rest, the relative distribution of blood in the vasculature of the body is as follows: Arteries about 11 % total blood; Veins at least 60%, they are the blood reservoir of the body. If arterial pressure falls, the sympathetic division of the ANS causes venous constriction, literally squeezing blood from the veins back into the heart (increases venous return) and this results in an increase in arterial blood volume. Myogenic Autoregulation Automatically adjusts Blood Flow Myogenic autoregulation means that vascular smooth muscle can regulate its own state of contraction. For example, if there is an increase in blood pressure, this leads to an increase arteriolar blood flow. However, the arteriole walls are stretched due to the increase in pressure and this triggers constriction of the arteriole wall, leading to a decrease in blood flow. The exact mechanism is unclear, but it is hypothesized that there are stretch sensitive Ca2+ channels on VSM. The signal may also consist of vasoconstrictive paracrines (endothelins) from endothelial cells themselves. Paracrines alter Vascular Smooth Muscle Contraction Tissue and endothelial paracrines locally control arteriole resistance. In the body, nitric oxide (NO), previously known as endothelial-derived relaxing factor (EDRF) causes relaxation of VSN and hence vasodilation of blood vessels in the body. The heart drug used for angina (pain from cardiac ischemia) nitroglycerin is metabolized in the body to NO and causes systemic vasodilation and a large drop in blood pressure. The amino acid arginine is a precursor to NO, and is converted into NO by the enzyme NO synthase. In the body, NO is broken down in seconds. There is a family of signal molecules called Prostaglandins which have been known to have an effect on blood vessels. The vasoactive substance histamine is often released by defense cells in times of an inflammatory response. Like NO, histamine can cause local or systemic vasodilation and decrease BP. Adenosine acts as a vasodilator in myocardial tissue. Myocardial hypoxia causes the release of adenosine which causes vasodilation. Not all vasoactive paracrines reflect changes in metabolism: Kinins and histamine are potent vasodilators that play a role in inflammation. Serotonin can act as a vasoconstrictive paracrine released by activated platelet cells to slow blood loss. Sumatriptan is a vasoconstrictive serontonin agonist used to treat migraines. The Sympathetic Division is Responsible for Most Reflex Control of Vascular Smooth Muscle Neural and hormonal signals affect smooth muscle contraction. As we have seen, most systemic arterioles are innervated by sympathetic neurons. The exceptions include: the brain arterioles and erectile arterioles of penis and clitoris. Sympathetic neuron activity: Tonic norepinephrine (NE) helps maintain myogenic tone. NE acts on -receptors on smooth muscle causing vasoconstriction. An increase in NE release means increases in constriction. A decrease NE release causes a decrease in constriction (i.e., causes 6 vasodilation). Epinephrine (E) from adrenal medulla also binds to -receptors, these -receptors respond to NE more greatly than they respond to E, but both NE and E cause vasoconstriction. The -receptors respond primarily to circulating E, when they are bound by E they cause vasodilation in this tissue being supplied by blood vessels with -receptors. These -receptors are found in vascular smooth muscle of heart, liver, skeletal muscle, so this means that blood supply to these organs increases when -receptors are stimulated. Remember the fight-or-flight response? Generally speaking, NE has a greater affinity (binding power) for -receptors and E has a greater affinity (binding power) for receptors. Exchange at the Capillaries Exchange between the plasma of blood and the cells occur at capillaries. Capillaries have thin walls and pores to allow passage of gases, water, dissolved solutes. Proteins and blood cells are too large to pass through the capillary wall. Molecules move from the blood to the interstitial space by diffusion and are aided by hydrostatic pressure. Most cells are within 0.1 mm of nearest capillary, this means that rapid diffusion is possible. Capillary density is directly related to metabolic needs of tissue, the higher the metabolism – the more capillaries. The total adult capillary exchange surface area is about 6300 m2 (nearly 2 football fields). Remember, the greater the surface area, the greater the rate of diffusion?!? There are three types of capillaries (or capillary beds): 1. Continuous capillaries: these are closely joined cells with tight junctions holding together adjacent endothelial cells. Small molecules cross through pores and larger molecules cross in vesicles via transcytosis. 2. Fenestrated capillaries: Have fenestrations, which mean “pores”. Molecules can pass rapidly. These are found in the kidney and intestine, associated with absorptive epithelia. The bone marrow has fenestrated capillaries with the ability to temporarily open gaps wide enough for proteins and blood cells to squeeze through to enter the blood. 3. Sinusoidal capillaries: The most permeable of all capillary beds. They have large gaps in the endothelial lining and are highly convoluted (twisted) capillaries. Found in the liver and the spllen The Velocity of Blood Flow is Lowest in the Capillaries Low velocity allows diffusion to go to equilibrium. The total cross-sectional surface area of all capillaries determines the velocity of blood. A large total capillary cross-sectional area gives a low velocity of blood flow. The fastest flow of blood is seen in the arterial system, where no exchange (diffusion) occurs. Most Capillary Exchange Takes Place by Diffusion and Transcytosis Diffusion rate for permeable solutes is determined by concentration gradient between plasma and interstitial fluid (ISF). O2 and CO2 diffuse out freely. Concentrations reach equilibrium by the venous end of the capillary system. Blood cells and most plasma proteins are too large to leave. Lymphatic system returns those proteins that do escape. Protein hormones and cytokines enter ISF by: Large pores in certain capillaries. Transcytosis in others Capillary Filtration and Reabsorption take Place by Bulk Flow Bulk flow is the mass movement of water and dissolved solutes between blood and the interstitium as the result of two forces: Hydrostatic Pressure (HP) and Colloid osmotic pressure (COP). Remember from the beginning of semester, HP is the force of a fluid on the walls of its container. HP is the driving force for filtration, which is the net movement of fluid from the capillary into the interstitium. 7 Colloid osmotic pressure is a force generated by protein in solution. COP is the driving force for reabsorption, which is the net movement of fluid back into the capillary from the interstitium. In most capillaries, net filtration occurs at the arterial end and net reabsorption occurs at the venous end. HP forces water and solutes out of capillary through pores but it decreases along length of capillary (from arterial to venous) as energy is lost to friction. Colloid osmotic pressure remains constant along capillary length. The overall flow is determined by the difference between hydrostatic and colloid osmotic pressures. The bulk flow filters out a volume of about 3 L/day (entire plasma volume) into the interstistium. This represents about 10% of the total fluid that is not reabsorbed, the lymphatic system returns this lost fluid to the cardiovascular system. THE LYMPHATIC SYSTEM Lymphatics interact with 3 systems: 1) Cardiovascular system – where it returns filtered fluid and proteins from the tissue spaces (interstitium) back to the circulatory system. 2) Digestive system – where it transfers (absorbs) fat from the small intestine to circulatory system. 3) Immune system – where it traps pathogens for the immune system to deal with. In terms of interaction with the circulatory system, the most important function of the lymphatic system is its role as a one-way pump, moving ECF from the tissues and returning it to the circulatory system. The closed-ended lymph capillaries are closely associated with blood capillaries, in fact they are found almost everywhere that blood vessels are found. Lymph vessels have thinner walls than capillaries and are anchored to surrounding connective tissues and fibers so the vessels are held open. The large gaps allow bulk flow of fluid, proteins and bacteria into the lymph capillary, thus they are considered highly permeable vessels. The fluid inside the lymphatic system is called lymph (Gk, meaning ‘milk’). Lymph capillaries join to form larger lymph vessels and pass through lymph nodes. Lymph nodes are nodules containing immunologically active cells. They act to filter lymph along its route to return to the heart. The largest lymph vessels (thoracic and right lymph duct) empty into large veins just under collarbones. Lymph flow depends on several things. For one, there are contractile fibers in their endothelial cells and the smooth muscle in the walls of larger vessels also contract rhythmically, creating a sort of automated lymph pump. Larger vessels also have one-way valves, as do vein, to ensure unidirectional flow. Just as in veins, external compression by skeletal muscle also assists the return of lymph to the cardiovascular system. Inhibition of the muscle pump results in edema (see below). The lymphatic system is pivotal in recycling plasma proteins and keeping the low interstitial protein concentration that is critical in maintaining homeostasis. The force of colloid osmotic pressure opposes capillary hydrostatic pressure. If hydrostatic pressure were unopposed, it would result in excess fluid movement into interstitial space (edema). For example, during an inflammatory response, histamine makes capillary walls leakier, more fluid and proteins move into the interstitium and causes edema. What is Edema? Edema is an increase in interstitial fluid volume. It usually has one of two causes. It’s either due to inadequate drainage of lymph or capillary filtration greatly exceeds capillary reabsorption Let’s examine both causes. Inadequate lymph drainage can be due to obstruction of lymph flow. Parasites, cancer, fibrotic tissue growth can block lymph movement. In some surgeries for breast cancer, the lymph 8 nodes along the arm are removed in order to assess the spread of the disease. Removal of the lymph drainage in the arm may then result in edema of the arm. Edema can also be the result of alterations in capillary exchange. Here are some of the factors that disrupt normal capillary filtration-absorption balance: Increase in capillary hydrostatic pressure. Usually from increased venous pressure, e.g. Heart failure. Decrease in plasma protein concentration from liver failure or severe malnutrition. Also, if there is an increase in interstitial proteins, perhaps due to excessive leakage of proteins into interstitial fluid. Patients are instructed to keep immobilized injured limbs elevated (above the heart) so that gravity will aid lymph flow. Physical and massage therapists will use gentle massage toward the heart to help force lymph past the one-way valves. This can decrease edema in an arm or leg. Imbalances can cause your body to attempt to compensate. For example, hemorrhage or severe dehydration can lead to a drop in arterial pressure. This causes a drop in capillary hydrostatic pressure which in turn will cause increases in reabsorption. REGULATION OF BLOOD PRESSURE Located in medulla oblongata, the medullary cardiovascular control center integrates neural control of blood pressure. The Baroreceptor Reflex is the Primary Homeostatic Control for Blood Pressure Baroreceptors are stretch-sensitive mechanoreceptors that are located in the walls of the carotid artery and aorta. As you may recall, these are tonic receptors, so they do not adapt even if the signal being sent remains the same (they are slow to adapt). The Baroreceptor reflex is illustrated below: BP Action potential firing to M.O. baroreceptors BP Action potential firing to M.O. If we use the standard blood pressure of 120/80 as “normal”, then the baroreceptors in the aorta and carotid arteries will constantly fire AP’s to the integration center, which is the cardiovascular control center in the medulla oblongata. 1) If there is an increase in blood pressure, then the rate of signaling of the barorecptors to the MO will increase. Then there may be a change in the body directed by the MO to alleviate or oppose the increase in BP, e.g., vasodilation and reduction of heart rate. 2) If there is a decrease in blood pressure, then the rate of signaling of the barorecptors to the MO will decrease. Then there may be a change in the body directed by the MO to oppose the decrease in BP, e.g., vasoconstriction and increase heart rate and stroke volume. 9 What is Shock in Terms of the Cardiovascular System? Shock is the failure of the cardiovascular system to adequately perfuse the body. In class we’ll discuss four major ways that shock can arise in the body. 1. Cardiogenic Shock This type of shock is characterized by a failure of the heart to provide the driving force for blood flow, in other words, this is when the central pump fails. An example of this is cardiac arrest (when the heart has stopped beating). If the heart is no longer beating, then the blood pressure will quickly fall and fail to adequately perfuse the tissue. Another example of this is congestive heart failure, when one side of the heart cannot maintain the pumping ability of the other side of the heart. Again, the heart cannot generate adequate pressure to perfuse tissues. The act of cardiovascular pulmonary resuscitation (CPR) is done in emergencies when you believe that someone’s heart is no longer pumping. Compression of the chest above the heart is an attempt to continue the pumping role of the heart until medical assistance arrives. 2. Volumetric Shock The normal blood volume of a 70 Kg man is about 5 L. As we have seen earlier (page 4 above), the total blood volume will have an impact on MAP. Volumetric shock will occur if you loose a significant volume of blood (decrease in blood volume => decrease in MAP). For example, if a person is injured and hemorrhaging occurs (blood loss), there is a chance of going into shock due to the reduction in vascular volume. Even if a person is bleeding internally, this is still a loss of blood from the vascular system and shock will ensue if blood loss is substantial. This is why inhibiting further blood loss (by compression and elevation of affected area) is so important. Another part of restoring vascular volume is to give fluids to a person suffering from volumetric shock. 3. Septic Shock If a person has a specific bacterial infection, this may lead to septic shock. When certain bacterial gain access to the blood stream (for example from an open cut or through the G.I. tract) they illicit an appropriate immune response, and defense cells like masts cells and basophils release histamine. Histamine is a potent vasodilator. If histamine is released systemically, then systemic vasodilation will occur and this will lead to a rapid and dramatic drop in MAP. The body naturally counters this response with the release of vasoconstrictors, namely NE and E ( receptors stimulation = vasoconstriction). HOWEVER, the bacterial releases blockers and these inhibit the body from being able to cause vasoconstriction. The result is a continued drop in MAP that may lead to septic shock. Often treatment will involve the administration of several vasoconstrictors in order to remedy the drop in MAP. 4. Anaphylactic Shock An allergy is an inappropriate immune response, in that the immune system responds aggressively to a substance in your body that is not a real danger. Anaphylactic shock involves an allergic inflammatory response that results in the systemic release of histamine (the potent vasodilator). A common example is if someone were allergic to bee stings. The bee venom, which is harmless, elicits a major inflammatory response, histamine is released systemically and MAP drops significantly. Typically, the bodies attempt to counteract this with vasoconstrictors is overwhelmed by the massive vasodilation. This is why those who know they are allergic to bees or peanuts carry an “epi-pen” with them. This is a supply of epinephrine which is injected intramuscularly (IM) to commence systemic vasoconstriction in an attempt to restore MAP. 10 CARDIOVASCULAR DISEASE Diseases of the heart and blood vessels account for nearly 1/2 of all deaths in the US. Coronary artery disease (coronary heart disease) is the leading cause of death for men and women. This occurs when coronary vessels become blocked with cholesterol and Ca2+. Risk Factors for Cardiovascular Disease Include Gender, Age, and Inheritable Factors It is possible to predict a person's likelihood of developing cardiovascular disease by examining controllable and uncontrollable risk factors. The uncontrollable risk factors include: Gender: Men are 3-4x more likely than women to develop coronary artery disease. Age: After 55, deaths from coronary heart disease in men and women (not on hormone replacement) are nearly equal. In general, risk increases with age. Heredity: Close relatives with coronary artery disease increase risk. Diabetes mellitus: Diabetes mellitus increases risk because it contributes to fatty deposits in the blood vessels. Controllable risk factors include: Cigarette smoking; obesity; sedentary lifestyle; elevated serum cholesterol and triglycerides; untreated high blood pressure; and diabetes mellitus (to some extent). Smoking: Nicotine is a poison. Organic gardeners soak cigarette tobacco in water overnight and spray the resultant nicotine solution on bugs to kill them. Nicotinic receptors stimulate sympathetic neurons at preganglionic synapses – remember that ACh is the NT released in the ganglion by the pre-ganglionic neurons. As a result of activation of sympathetic pathways, there is vasoconstriction that increases blood pressure. Smoking also increases the risk of atherosclerosis (hardening or arteries). Finally, cigarette smoke contains significant amounts of carbon monoxide, which binds to hemoglobin and decrease the oxygen carrying capacity of blood. If decreased blood flow due to narrowing of the coronary vessels is compounded by less oxygen being carried in the blood, the heart muscle is likely to be damaged even if flow is not totally occluded. The role of elevated cholesterol in development of coronary artery disease is critical. Cholesterol isn't soluble in plasma (lipids are hydrophobic), so they need carriers in the blood. The two types of cholesterol carriers High-Density Lipoprotein, HDL the "Healthy" type of cholesterol carrier and the Low-Density Lipoprotein, LDL, the "Lethal" type of cholesterol carrier. The HDL transports cholesterol from the body to the liver. This is more desirable because it's associated with lower risk of heart attacks. Normal LDL levels are necessary for cells to uptake cholesterol. In the cells, cholesterol is used to make cell membranes and steroid hormones. However, excess cholesterol gets carried around the body by LDL’s and deposited into arterial walls. The macrophages then ingest LDL-cholesterol and this contributes to the formation of fatty streaks just under the endothelial lining of larger arteries. Macrophage paracrines attract smooth muscle cell migration and reproduction. The streaks grow into bulging plaques (containing Ca2+) that narrow the lumen of the vessels. These plaques harden into calcified regions and fibrous collagen caps. Plaques can be divided into two groups: stable plaques and vulnerable (unstable) plaques. Stable plaques have thick collagen caps that separate the core from the blood. Vulnerable plaques have thin caps that are likely to rupture and trigger formation of blood clots (thrombi). One theory suggests that macrophages release enzymes that dissolve collagen and convert stable plaques to vulnerable plaques. If a thrombus blocks blood flow to the heart muscle, a heart attack (myocardial infarction) results. Blocked blood flow decreases heart muscle's O2 supply which can cause heart damage. This can lead to electrical conduction disruption and irregular heartbeats (arrhythmia), cardiac arrest and death. 11 Hypertension Represents a Failure of Homeostasis Hypertension is chronically elevated blood pressure (BP), with systolic greater than 140 mmHg and diastolic greater than 90 mmHg (140/90). It is the single most common reason for a visit to a physician and use of prescription drugs in the USA. Over 90% of the cases have what is termed essential or primary hypertension, in which there is no clear cause of the elevated BP. Typically cardiac output (CO) is normal and the elevated blood pressure is from an increase in peripheral resistance. This could be from a lack of nitric oxide (NO), which causes vasodilation and reduces BP. In about 5-10% of hypertension cases the cause is known and is due to some underlying pathology, this is called secondary hypertension, because it is a secondary condition to another causing it. For example, it is possible that an endocrine disorder may cause fluid retention, thus elevating BP.