EPIDURAL ANALGESIA & ANESTHESIA
advertisement

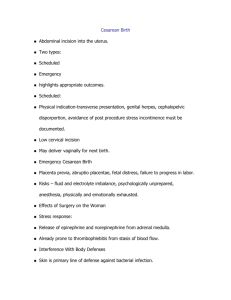
EPIDURAL ANALGESIA & ANESTHESIA What is it? Epidural anesthesia & analgesia is: pain control using opioids (analgesia), and opioids with a local anesthetic (anesthesia). Where is it? The epidural space is a potential space located between the vertebral column & the dura mater. It contains fat, veins, lymphatics & the spinal nerves. Usually placed at the L2-L3 or L3-L4 intervertebral spaces as the spinal cord ends at L1L2. What is the difference between spinal and epidural? Epidural: is in the epidural potential space. Spinal: is in the intrathecal space (subarachnoid space). This is where the CSF fluid is located. The dose of drugs required in the intrathecal space is 1/10 of that required epidurally. So, if the epidural catheter is in intrathecally, & the amount of drug that would be given epidurally is given intrathecally, it can have profound detrimental effects (sudden profound motor weakness or sensory block, severe hypotension, respiratory arrest, circulatory collapse, seizures, arrythmias, cardiac arrest). How does it work? Epidural narcotics block the transmission of pain impulses to the brain at the level of the spinal cord. Because of this, excellent pain control can be achieved with little CNS side effects. The patient can move more freely and cough more readily postoperatively. Epidural opioids have no effect on motor function, therefore pain control is achieved without loss of mobility. Epidural anesthetics block pain impulses just before they enter the dorsal horn of the spine. The extent of the block depends on the dose. Low dose blocks can provide pain relief without loss of motor and minimal or no loss of sensation. With the low doses of combined opioids & local anesthetics now used, it is possible to get a very segmental analgesia/anesthesia with catheters even placed in the thoracic spine for surgeries in that area. The smaller the nerve fiber, the faster and less local anesthetic it takes block conduction. Pain fibers are one of the smallest. Temperature sensation is similar in size to pain (thus we check dermatomes with ice or alcohol swabs), next is sensitivity to touch and motor function is largest. That is why it is possible to have pain control with motor function left intact even when local anesthetics are used. What medications are used? Narcotics Epimorph, Fentanyl, Demerol, & Sutentanil. Preservative free morphine is used as the preservative in regular morphine is neurotoxic. Narcotics slowly difffuse from the epidural space across the dura and arachnoid membranes into the CSF. They do not get systemically absorbed. Narcotic Onset Peak Duration of Bolus Dose Infusion Rate min min Action Epimorph 30-90 906-24 hrs 3-5mg 0.2-1.0 mg/hr 120 Fentanyl 5-15 10-20 4-6 hrs 50-200mcg 50-100mcg/hr Sufentanil 5-10 10 2-4 hrs 10-60 mcg 5-15 mcg/hr Meperidine 5-10 10-20 6-8 hrs 10-40mg 5-20 mg/hr Local Anesthetics Bupivicaine (Marcaine) and Ropivacaine Local Anesthetic Concentration Rate / Hr Bupivicaine 0.5 – 1 mg/ml 5-15 ml / hr Ropivicaine 0.5 – 1 mg/ml 5-15 ml / hr Ropivicaine is a newer local anesthetic, similar to bupivicaine, with less urinary retention, easier on the heart, less motor nerve involvement & has a longer duration of action. Only epidural morphine & demerol are to be administered via intermittent bolus doses by epidural certified nurses. No local anesthetics are to be administered by nurses. Fentanyl & Sufenta are lipophilic, or fat loving and have a limited ability to spread in the CSF. This allows them to have a segmental effect at their injection site and have a rapid onset of action. Morphine is hydrophilic or water loving, allowing it to readily spread in the CSF producing analgesia in dermatomes far removed from the initial site of injection, and have a slower onset of action. Any drug used for epidural analgesia / anesthesia if drawn up from a glass ampule, should be drawn up through a fitered needle or given through a filter on the epidural catheter to prevent introducing small particles of glass into the epidural space. These drugs may be given as bolus doses or as continuous infusions. Continuous infusions are run on special epidural pumps that limits the rate of infusion to the lower epidural rates. Naloxone (Narcan) reverses opioid effects. There is no reversal for local anesthetics. Naloxone & Ephedrine should be readily available on the unit. Ephedrine increases BP, is a vasopressor & acts like epinephrine. On the unit, when anorder for Ephedrine is received from anesthesia, a physician is to be paged STAT to administer the drug. On L&D the nurses may administer the ephedrine upon the order of a physician on their way to the unit. Only the anesthetist responsible for the epidural should order other narcotics or CNS depressants by another route. What are the advantages of epidurals? Smaller amounts of narcotic can reduce pain for long periods of time with fewer CNS side effects. Motor function can be left intact (walking epidural). Patients mobilize earlier, breathe & cough easier. Who should not have an epidural? Patients who refuse Patients that have coagulopathies (platelet count < 100,000 or elevated PT, PTT, or INR) Local infection / rash at insertion site Allergy / sensitivity to drugs used Septicemia Shock / hypotension Spinal surgery / fractures Anticoagulation (relative contraindication) Who can give epidural bolus doses? Anesthetists, specially trained nurses on 4N, ICU, & Recovery Room. L&D NURSES ARE NOT ALLOWED TO GIVE BOLUS DOSES (AWHONN Guidelines) What should be done prior to epidural insertion? The patient should understand the epidural & have proper teaching. On L&D there is an “epidural information sheet” that should be read. It is the anesthetists responsibility to obtain “informed consent” prior to insertion and explain complications and answer any questions. The patient should have baseline vital signs done (& EFM x 20 min for L&D) The patient is bolused with 500-1000ml Ringers Lactate just prior to insertion. This is done because the epidural causes decreased sympathetic tone & the blood tends to pool in the periphery causing hypotension. (L&D patients on fluid restriction, Indocid, MgSO4 or Ritodrine need to have the bolus amount specifically ordered.) The patient should void prior to insertion. Emergency equipment should be set up &functional in the patient’s room (ie. Suction, O2, Bag-Valve Mask on L&D) How is the epidural put in? The patient in placed in the side lying with legs flexed and head chin to chest “fetal position” or sitting at the edge of the bed, feet resting on a chair with wlbows on knees and head flexed. Alternate arm position – rest arms on over-bed table, head on arms. (Provides maximal interrvertebral spaces) The site is cleansed with proviodone iodine. The anesthetist injects local anesthetic to the skin. A needle is inserted between the vertebrae, through the ligamentum flavum into the epidural space. An epidural catheter is inserted usually a few cm up the epidural space. The injection cap is attached to the catheter. The catheter is secured only by taping it up the length of the patient’s back with waterproof tape. Label the catheter with the “epidural” label on the insertion tray. Tape connections (and ports if present). How can you tell you’re in the right spot? The anesthetist can feel a sudden change in pressure when he goes through the ligamentum flavum into the epidural space. There should be <0.5 ml of clear fluid or air in the epidural catheter. Presence of more than 0.5 ml may be CSF and indicate intrathecal (spinal) placement. Blood may indicate catheterization of a blood vessel. (Blood vessels are present in the epidural space). A test dose of drug containing epinephrine should always be given. Watch for an increase of 20-30% in heart rate. This would indicate intravascular injection. The catheter placement should ALWAYS be checked prior to Bolus doses by attaching an empty 12 cc syringe to the epidural catheter and gently aspirating. (Expect to see < 0.5 cc clear to pale yellow fluid). If there is any suspicion of blood or fluid return, DO NOT INJECT THE BOLUS DOSE & NOTIFY THE ANESTHETIST. Does the patient feel anything when the epidural medication is administered; They may feel a warmth or tingling down their legs Why does my patient shiver uncontrollably after epidural medication & what can I do? This is the body’s vasoconstriction response to the vasodilation that occurs with an epidural. Provide warm blankets and explain to the patient what is going on. Is there any special positioning required? If the block is unilateral or patchy, have the patient lay with the unaffected side down. Gravity may improve the block. It this has not worked after 20 min, anesthesia should be notified and more medication may need to be administered. Obstetrical patients: elevate HOB slightly, position in left or right lateral tilt of only 2030 degrees x 5-10 min during initial epidural dose. This allows for bilateral diffusion of medication while preventing aortocaval pressure causing hypotension. Then full lateral position. This ensures uterine displacement and prevents further hypotension. A SYSTOLIC BP < 90 mm Hg IS NOT CONSIDERED ADEQUATE TO MAINTAIN UTERINE BLOOD FLOW AND FETAL OXYGENATION. Turn & position q 30 min – l hr to promote even blockade and promote progress of labor. Wedge R hip for all procedures, including vaginal exams. At 8-9 cm dilated, elevate the HOB 45 degrees to promote downward movement of the sensory blockade. In stage l, labor pain sensation travels along sympathetic nerve fibers at T10-T12 and L1-L4. In stage 2 labor pain sensation travels along sympathetic nerve fibers at L2-L4 and S2-S4. So the analgesia / anesthesia needs to be lower for delivery. In stage 4, pain sensation is back to T10-T12 and L1-L4. Notify anesthetist when patient is fully dilated, as he may decrease or stop the infusion gtt, or give a bolus of low dose narcotic to facilitate pushing during stage 2. Prior to each ambulation, the patient’s BP must be taken in the laying, sitting and standing position. To rule out postural hypotension. The patient must be accompanied by the nurse for the first ambulation. Motor Blockade + Sensory Blockade + V/S = Ambulation 0 T8-10 Stable Have the patient do a deep knee bend at the bedside prior to ambulation. Motor & sensory blockade, V/S, (FHR) should be done prior to each ambulation. (Motor & sensory function can change and be different from one side to the next) What happens if the epidural catheter comes apart? If it has been disconnected for < 8 hrs and the fluid level is within 12 cm from the catheter end, obtain a sterile epidural connector, cleanse 25 cm of the outside of the epidural catheter with betadine, wipe with a sterile 2x2, cut 12 cm from the catheter end with sterile scissors & attach the new sterile connector. Tape the connection. What patient monitoring is required? On L&D: 1) upon initiation: BP, P, R, EFM q3min x 20 min or until stable. Check pulse oximetry with vital signs NURSE IN CONSTANT ATTENDANCE 2) after a bolus (includes increased continuous rate) q 5 min x 20 min or until stable 3) for the duration of the epidural q 15-30 min 4) stage 4 q15min x l hr if stable 5) sensory & motor blockade q 30 min 6) intake & output q1h 7) pain scale & sedation q 30 min call if sedation: somnolent, sudden motor / sensory weakness, respiratory depression rate < 8 min, shallow resps, BP < 100 systolic, change in heart rate > 20-30%, any untoward effects Per ward: Opioids only 1) BP &P q15min x 2, q30minx2, q1hx2, q4h 2) respiratory depression (rate & depth) q1h x4, q2h x 20, q4h x12 hr after last dose 3) Sedation q1h x 4, q2h x 20, q4h x 12hr after last dose 4) Pain level q1h x 4, q2h x 20, q4h x 12hr after last dose Local anesthetics: As above and 1) motor function q 15min x 4, q1h x4, then q4h for duration 2) sensory level q15min x 4, q1h x4, then q4h for duration Who can remove the epidural catheter? A current epidural certified RN& the anesthetist. How? A Dr. order from the anesthetist is required. Place the patient in fetal position side laying or at the edge of the bed with elbows on knees with head flexed or using the alternate arm position. Using universal precautions, remove the tape. Watch for signs of bruising, leakage of fluid, infection. Slowly remove the catheter. Observe the catheter tip for a black marking to make sure the catheter has not sheared off. Apply sterile 2x2 drsg. Check dressing q12h x 24h Dressing may be removed after 24 h Document procedure & how patient tolerated & condition of site & drainage. A PATENT IV MUST BE INSITU X 24 HR AFTER EPIDURAL REMOVAL What if my patient is on heparin? Do not remove an epidural catheter for 8-12 hr after LMWH (low molecular weight heparin) or sc is given Do not give LMWH or sc Heparin for 2 hrs after removing an epidural catheter Do not start on IV heparin for 6 hrs after an epidural catheter has been removed Patients receiving low dose warfarin must have their prothrombin time & INR checked prior to removal. Notify anesthesia of results. An RN may NOT remove an epidural on a fully anticoagulated patient (IV Heparin) Check dressing site and assess for epidural hematoma q2h x 24h Epidural hematoma is a surgical emergency characterized by: Back & abdominal pain Change in sensation & motor function to legs Change in bowel and / or urinary incontinence The hematoma may occur on insertion or removal What are the complications? See attached sheets