Anatomy and Pathology of the Cerebellar Peduncle
advertisement

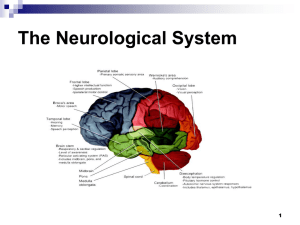
Anatomy and Pathology of the Cerebellar Peduncle Toshio Moritani MD, PhD, Akio Hiwatashi MD, Henry Z Wang MD, PhD, Yuji Numaguchi, MD, PhD, Leena Ketonen MD, PhD, Sven E Ekholm MD, PhD, Per-Lennart A Westesson MD, PhD, DDS Division of Diagnostic and Interventional Neuroradiology, Department of Radiology, University of Rochester Medical Center, Rochester NY E-mail: moritani2001@yahoo.com Introduction Lesions in the cerebellar peduncle include various pathological conditions: infarction, various primary or secondary degeneration, demyelinatiing disease, toxic metabolic disease, trauma, and benign and malignant tumors. Their differential diagnoses are occasionally difficult. We illustrate the anatomy, pathology and imaging findings of the cerebellar peduncle. Anatomy Gross anatomy (Figure 1A-F). The cerebellum is connected to the brainstem by three cerebellar peduncles: 1) the inferior cerebellar peduncle (restiform body and juxtrarestiform body) 2) the middle cerebellar peduncle (brachium pontis), and 3) the superior peduncle (brachium conjunctivum) (1). The wall and lateral roof of the 4th ventricle are formed by the inner surfaces of the cerebellar peduncles; the rostral portion by the superior peduncles; and the caudal portions by the inferior peduncles (Figure 1A-F). The middle cerebellar peduncle is lateral to inferior and superior peduncles and is not directly exposed to the cavity of the 4th ventricle. The middle cerebellar peduncle can be divided into three portions: brain stem portion, ventricular portion, and cerebellar portion (Figure 1E). This classification can be a useful application in surgery (2). Cerebellar connections (Figure 1G). The cerebellum is linked to other parts of the brain by numerous efferent and afferent fibers that are grouped together on each side of the cerebellum in three peduncles (1). Most of the afferent tracts enter the cerebellum via the inferior and middle cerebellar peduncles. A few enter via the superior cerebellar peduncle. Afferent fibers are far more numerous that efferent fibers by a ratio of 40:1 (3). The cortico-ponto-cerebellar pathway, composed of the corticopontine tract and the pontocerebellar tract, is major afferent fibers through the middle cerebellar peduncle. It arises from the cerebral cortex and enters the ipsilateral pontine nucleous and almost entirely crossed to the contralateral cerebellum. Olivocerebellar fibers form the largest component of the inferior cerebellar peduncle. Most of efferent tracts of the cerebellum are via the superior cerebellar peduncle. They mostly arise from dentate nucleus and decussate at the levels through the inferior colliculus. Most of the fibers enter the contralateral red nucleus and project the cerebral cortex via the thalamus. Symptomatology Lesions of the cerebellar peduncle result in variable clinical symptoms, ranging from vertigo or vomiting as the only clinical presentation to facial palsy, ataxia, nystagmus, diplopia, dysphagia, dysarthria, deafness, contralateral motor weakness, trigeminal sensory loss, dysmetria of the limb, loss of pain and temperature sense, Horner's syndrome, and "locked-in" syndrome (1,4,5). Imaging of normal anatomy (Figure 1F). The posterior fossa is difficult to evaluate on CT because of poor contrast resolution and artifacts. MRI more clearly demonstrates the anatomy and pathology of the middle cerebellar peduncle in the posterior fossa than does CT. FLAIR images occasionally show a slight increase in signal intensity in normal middle cerebellar peduncles (Figure 1F). Infarction (Figures 2-5) The inferior cerebellar peduncle is mainly supplied by the posterior inferior cerebellar artery (PICA). The middle cerebellar peduncle is supplied by the anterior inferior cerebellar artery (AICA) and partly by the superior cerebellar artery (SCA). The superior cerebellar peduncle is mainly supplied by the SCA. These arteries vary greatly in origin, size, course, and supply area, the aera of infarction are variable in extent and location, ranging from a small infarct localized into the cerebellar peduncle (Figure 2 and 3) to large involvement of the cerebellar hemisphere, and can be associated with the involvement of pons, midbrain, thalamus and occipital lobe (Figure 4) (4). Bilateral AICA territory infarcts are very rare (Figure 5), and can occur due to hypoperfusion in the watershed area between the AICA and the SCA (6). Wallerian degeneration of the pontocerebellar tracts secondary to pontine hemorrhage or infarction (Figure 6). Wallerian degeneration secondary to pontine hemorrhage or infarction is usually bilateral. Differentiating from infarction is important. This is because of damage to both ipsilateral pontine nuclei (which deliver axons to the contralateral cerebellar hemisphere) and the ipsilateral axons (which originate from the contralateral pontine nuclei and course into the ipsilateral cerebellar hemisphere) (Figure 6G) (3). The T2 prolongations were first recognized from 26 days to 4.5 months after insult Theoretically, the wallerian degeneration of the pontocerebellar tracts should extend out to the mossy fibers in the cerebellar cortex, as seen on the pathological specimen; however this is beyond the resolution of MRI (3). Hypertrophic olivary degeneration occasionally coexists with these lesions, because the lesion can also involve the area in the Guillain-Mollaret triangle (Figure 6H) (7). Osmotic myelinolysis (Figure 7). Symmetrical lesions in bilateral middle cerebellar peduncles without central pontine myelinolysis (CPM) was reported as cerebellar peduncle myelinolysis (8). However, in our case, bilateral cerebellar peduncle lesions accompanied by CPM (Figure 7). These lesions are presumed to be due to myelinolysis itself or secondary degeneration related to CPM. Solvent encephalopathy (Figure 8) There have been a few case reports of middle cerebellar peduncle lesions in solvent encephalopathy (chronic toluene intoxication) in which the cerebral and cerebellar white matter, thalamus, basal ganglia, internal capsule, and brain stem are also involved (9, 10) (Figure 8). These patients' symptoms are usually composed of pyramidal tract and cerebellar signs. The middle cerebellar peduncle lesions can be primary or secondary degeneration. Herpes encephalitis (Figure 9) Bilateral middle cerebellar peduncle lesions were present in a patient with herpes encephalitis with bilateral temporal lobe involvement (Figure 9). The cause of these lesions is unknown. Secondary transneuronal degeneration via bilateral cortico-pontocerebellar pathways may be one of the possible explanations for these lesions (Figure 6G) (11). Crossed cerebellar diaschisis and atrophy (Figures 10 and 11) Crossed cerebellar diaschisis and atrophy presumed to be associated with transneuronal metabolic depression in the cerebellum through cortico-ponto-cerebellar pathways (middle cerebellar peduncle) or other pathways such as cerebello-rubrothalamic tract (superior cerebellar peduncle) (Figure 10) (12,13) Unilateral atrophy of the middle cerebellar peduncle and cerebellar hemisphere occurs as a sequela of ischemic or destructive injury of the contralateral cerebral hemisphere (14). These findings are found in children with a history of extreme prematurity, perinatal intracranial hemorrhage, and recurrent seizures (Figure 11). Olivopontocerebellar atrophy (OPCA) and other primary degenerative diseases (Figure 12). OPCA is a degenerative disease characterized by atrophy of the pons, middle cerebellar peduncles, and cerebellar hemispheres. There are characteristic histologic changes, such as loss of specific fiber tracts and the presence of gliosis in the pons, middle cerebellar peduncles and cerebellum (15). The fibers affected in the pons are the transverse pontine fibers, while the pyramidal tracts and tegmentum are spared (Figure 12). Increased hyperintensity in the middle cerebellar peduncles are also reported in other multiple system atrophy, autosomal dominant spinocerebellar atrophy (16), Wilson’s disease, non-Wilsonian hepatocerebral degeneration (17), and fragile X syndrome (18). Leukodystrophy and leukoencephalopathy (Figure 13). Some kinds of leukodystrophy and leukoencephalopathy can also involve in the cerebellar peduncles. This leukoencephalopathy with vanishing white matter is an autosomal recessive disorder with chronic and progressive episodes of rapid deterioration, provoked by fever and minor head trauma. This is primarily an axonopathy, with myelin being secondarily affected (19) (Figure 13). Demyelinating disease: multiple sclerosis (MS), acute disseminated encephalomyelitis (ADEM) and progressive multifocal leukoencephalopathy (PML) (Figures 14-16) Brain stem and cerebellar involvement including cerebellar peduncles is common in patients with MS and ADEM. Cerebellar symptoms and signs are commonly seen in 50-80% in MS patients. On MRI brainstem lesions in 68% and cerebellar lesions in 49%-88% were detected (20). These lesions in MS or ADEM are often bilateral but asymmetric (Figures 14 and 15). In PML involvement of the posterior fossa including the cerebellar peduncles is also common (32%). Isolated disease in the posterior fossa is in 10% of PML patients (21) (Figure 16). Tumor (Figures 17 and 18). Benign tumors such as astrocytoma or cavernous angioma can involve in the cerebellar peduncle (Figures 17). An extra-axial tumor such as benign acoustic schwannoma occasionally displaces the middle cerebellar peduncle (Figure 18). Malignant tumors such as metastasis or glioblastoma multiforme also occur in the cerebellar peduncle. Tumors involving the ventricular portion or the cerebellar portion of the middle cerebellar peduncle can be removed by surgery (3). Neurofibromatosis (Figure 19) Hamartomatous lesions are observed in 80% of all patients with neurofibromatosis type 1. Multiple lesions in the basal ganglia, optic radiation, brainstem, and cerebellar peduncles are common (Figure 19). Pathologically, these lesions are foci of hyperplastic or dysplastic glial proliferation and considered malformations rather than neoplasms. Diffuse axonal injury (DAI) (Figure 20) The gray-white matter interface, the corpus callosum, and dorsal aspect of the upper brainstem including the superior cerebellar peduncle are three specific areas for the occurrence of DAI. Other less frequent locations include the caudate nuclei, thalamus and internal capsule. Cerebellar involvement including the middle cerebellar peduncle is uncommon (Figure 20). Conclusion Lesions in the middle cerebellar peduncle include various pathological conditions, ranging from infarction, tumor, infection, trauma and demyelination to primary and secondary degeneration. Understanding the anatomy, pathology, imaging characteristics is important for the differential diagnosis of lesions in the middle cerebellar peduncle. References 1)) 2) Carpenter MB. Cerebellum. In, Core Textbook of Neuroanatomy. 5th edition. Baltimore, MD: Williams &Wilkins, 1996; 583-623. Tomita T. Surgical management of cerebellar peduncle lesions in children. Neurosurgery 1986; 18:568-575. 3) 4) 5) 6) 7) 8) 9) 10) 11) 12) 13) 14) 15) 16) 17) 18) 19) 20) O'uchi T. Wallerian degeneration of pontocerebellar tracts after pontine hemorrhage. Int J Neuroradiol 1998; 4:171-177. Amenco P, Rosengart A, DeWitt D, Pessin MS, Caplan LR. Anterior inferior cerebellar artery territory infarcts. Mechanisms and clinical features. Arch Neurol 1993; 50:154-161. Milandre L, Rumeau C, Sangla I, Peretti P, Khalil R. Infarction in the territory of the anterior inferior cerebellar artery: report of five cases. Neuroradiology 1992; 34:500-503. Akiyama K, Takizawa S, Tokuoka K, Ohnuki Y, Kobayashi N, Shinohara Y. Bilateral middle cerebellar peduncle infarction caused by traumatic vertebral artery dissection. Neurology 2001; 56:693-694. Kitajima M, Korogi Y, Shimomura O, Sakamoto Y, Hirai T, Miyayama H, Takahashi M. Hypertrophic olivary degeneration: MR imaging and pathologic findings. Radiology 1994; 192:539-543. Mangat KS, Sherlala K. Cerebellar peduncle myelinolysis: case report. Neuroradiology 2002; 44:768-769. Aydin K, Sencer S, Demir T, Ogel K, Tunaci A, Minareci O. Cranial MR findings in chronic toluene abuse by inhalation. AJNR Am J Neuroradiol 2002; 23:1173-1179. Uchino A, Kato A, Yuzuriha T, Takashima Y, Heijima S, Murakami M, Endoh K, Yoshikai T, Kudo S. Comparison between patient characteristics and cranial MR findings in chronic thinner intoxication. Eur Radiol 2002; 12:1338-1341. Thajeb P, Shih BF, Wu MC. Crossed cerebellar diaschisis in herpes simplex encephalitis. Eur J of Radiol 2001; 38:55-58. Pantano P, Baron JC, Samson Y, et al. Crossed cerebellar diaschisis: further studies. Brain 1986; 109:677-694. Chung HD. Retrograde crossed cerebellar atrophy. Brain 1985; 108:811-889. Rollins NK, Wen TS, Dominguez R. Crossed cerebellar atrophy in children: a neurologic sequela of extreme prematurity. Pediatr Radiol 1995; 25:S20-25. Savoiardo M, Strada L, Girotti F, Zimmerman RA, Grisoli M, Testa D, Petrillo R. Olivopontocerebellar atrophy: MR diagnosis and relationship to multisystem atrophy. Radiology 1990; 174:693-696. Nakagawa N, Katayama T, Makita Y, et al. A case of spinocerebellar ataxia type 6 mimicking olivopontocerebellar atrophy. Neuroradiology 1999; 41:503-505. Lee J, Lacomis D, Comu S, et al. Acquired hepatocerebral degeneration: MR and pathologic findings. AJNR AM J Neuroradiol 1998; 19:485-487. Brunberg JA, Jacquemont S, Hagerman RJ, et al. Fragile X premutation carriers: Characteristic MR imaging findings of adult male patients with progressive cerebellar and cognitive dysfunction. AJNR Am J Neuroradiol 2002;23:1757-1766 van der Knaap MS, Barth PG, Gabreels FJ, et al. A new leukoencephalopathy with vanishing white matter. Neurology 1997; 48:845-855. Ormerod IE, Miller DH, McDonald WI, du Boulay EP, Rudge P, Kendall BE, Moseley IF, Johnson G, Tofts PS, Halliday AM. The role of NMR imaging in the assessment of multiple sclerosis and isolated neurological lesions. A quantitative study. Brain 1987; 110:1579-1616. 21) Whiteman ML, Post MJ, Berger JR, Tate LG, Bell MD, Limonte LP. Progressive multifocal leukoencephalopathy in 47 HIV-seropositive patients: neuroimaging with clinical and pathologic correlation. Radiology 1993; 187:233-40. Figure Legends Figure 1. Normal anatomy. A. Coronal FLAIR image. B,C,D. Sagittal T1WI. E. Axial T2WI. F. FLAIR image occasionally shows slightly high signal intensity in the normal superior (not shown), inferior and middle cerebellar peduncles. Middle cerebellar peduncle (m), superior cerebellar peduncle (s), inferior cerebellar peduncle (i), brain stem portion (B), ventricular portion (V), and cerebellar portion (C) of the middle cerebellar peduncle. G. Cerebellar connections. The cortico-ponto-cerebellar pathway (corticopontine tract and pontocerebellar tract) is major afferent fibers through the middle cerebellar peduncle. Olivocerebellar fibers (afferent fibers) are through the inferior cerebellar peduncle. Efferent fibers mainly arise from the dentate nucleus to the red nucleus through the superior cerebellar peduncle (cerebello-rubro-thalamic tract). Figure 2. An infarct in the inferior cerebellar peduncle. 72-year-old man with vertigo. A, B. FLAIR image and DWI show a hyperintense lesion, representing a small acute infarct in the left inferior cerebellar peduncle. Figure 3. An infarct in the inferior cerebellar peduncle. 57-year-old man with ataxia and diplopia. A, B. T2WI and DWI show a hyperintense lesion, representing an acute infarct in the right middle cerebellar peduncle. Figure 4. infarcts involving the superior cerebellar peduncle. 58-year-old man with loss of consciousness. A, B. FLAIR image and DWI show hyperintensity lesions in the left cerebellar hemisphere, and the midbrain including the left superior cerebellar peduncle. Figure 5. Bilateral infarcts in the middle cerebellar peduncle. 80-year-old man with ataxia and vertigo. A,B. T2WI and DWI at 24 hrs after onset clearly reveal homogenous round hyperintensity areas representing acute infarcts in the bilateral middle cerebellar peduncles and both cerebellar hemispheres. Figure 6. Wallerian degeneration in the middle cerebellar peduncle. 50-year-old man with quadriparesis and loss of consciousness after chiropractic. A, B. DWI and T2WI shows hyperintense lesions in the right cerebellar hemisphere and the left side of the pons at 10 days after onset, which represents subacute hemorrhagic infarcts. C, D. On follow-up MRI at 8 months after onset, old infarcts show very high intensity on T2WI and low intensity on FLAIR image as CSF. Symmetrical round hyperintense lesions in bilateral middle cerebellar peduncles are seen on T2WI and FLAIR image (red arrows). These lesions represent wallerian degeneration of the pontocerebellar tracts secondary to pontine infarction. E. T2WI at the level of the medulla demonstrates symmetric hyperintense lesions corresponding to the bilateral olivary nuclei, representing hypertrophic olivary degeneration (red arrows). F. On the pathological specimen of another patient, wallerian degeneration of the pontocerebellar tracts is recognized as symmetric rounded lesions (arrows) in bilateral middle cerebellar peduncles and extends out to the mossy fibers in the cerebellar cortex (open arrows) (Ref. 3. Int J Neuroradiol 1998;4:171-177. Toshihiro O'uchi MD with permission). G. Wallerian degeneration in bilateral middle cerebellar peduncles. The lesion involving the pontine nucleus can also involve the pontocerebellar tract from the contralateral pontine nucleus, which results in wallerian degeneration in bilateral middle cerebellar peduncles. H. Guillain-Mollaret triangle and hypertrophic olivary degeneration. The lesion involving the pontine nuclei can extend into the areas within the GuillainMollaret triangle, which causes hypertrophic olivary degeneration. Figure 7. CPM. 50-year-old female presenting with loss of consciousness after rapid correction of hyponatremia. A. B. T2WI shows a hyperintense lesion in the central pons representing CPM. T2WI also shows symmetrical round lesions in the bilateral middle cerebellar peduncles (red arrows). These lesions maybe due to myelinolysis itself or secondary degeneration. Figure 8. Solvent encephalopathy. 38-year-old man presenting with blurred vision, ataxic speech and bilateral pyramidal signs. T2WI shows diffuse hyperintense lesions in the white matter of both temporal lobes and mildly hyperintense lesions in the pons and bilateral middle cerebellar peduncles (red arrows). Figure 9. Herpes encephalitis. 40-year-old male presenting with a seizure. A. T2WI shows diffuse hyperintense lesions in the cortex and white matter in bilateral temporal lobes, which represents herpes encephalitis. B. Coronal FLAIR image shows hyperintense lesions in the bilateral middle cerebellar peduncles (red arrows) and the temporal lobes. Figure 10. Crossed cerebellar diaschisis. 27-year-old male, presenting with status epilepticus. He has a history of recurrent generalized seizures. A. FLAIR image shows hyperintensity lesions in the right cerebellar hemisphere (red arrows) and contralateral diffuse cerebral hyperintensity associated with status epilepticus. B, C. FLAIR images at the level of the brain stem show a hyperintense lesion in the right superior cerebellar peduncle (red arrows). These findings suggest that crossed cerebellar diaschisis of this case is related to retrograde transneuronal degeneration through the cerebello-rubro-thalamic tract. Figure 11. Crossed cerebellar atrophy. 19-year-old female. She had a history of recurrent seizures and perinatal intracranial hemorrhage. A. T2WI shows right cerebral atrophy with ventricular dilatation representing a sequela of perinatal intracranial hemorrhage. B. T2WI through the posterior fossa shows atrophy of the contralateral cerebellar middle cerebellar peduncle (blue arrow) and hemisphere. Wallerian degeneration of ipsilateral brain stem is also seen (red arrow). Figure 12. Olivopontocerebellar atrophy (sporadic type). 54-year-old woman presenting with dysarthric speech and dizziness. A, B. Axial and sagittal FLAIR images show hyperintensity in the middle (red arrows) and inferior cerebral peduncles (blue arrows). C. Axial FLAIR image also shows cruciform hyperintensity in the transverse pontine fibers on the anterior and lateral aspect of the pons. The tegmentum (light blue arrows) and the pyramidal tracts (green arrows) are spared. Figure 13. Leukoencephalopathy with vanishing white matter. An 11 year-old boy. A. T2WI shows diffuse white matter signal abnormalities similar to CSF intensity. B. T2WI also shows hyperintense lesions in the central tegmental tracts (blue arrows), pyramidal tracts (teal arrows), and inferior and middle cerebellar peduncles with atrophy (red arrows). Figure 14. MS. 40-year-old woman with multiple sclerosis, presenting with speech disturbance and ataxia. A, B. T2WI shows multiple asymmetric hyper-intense lesions in the pons, middle cerebellar peduncles (red arrows) cerebellar hemispheres, and in the deep white matter, which is characteristic of MS. Figure 15. MS. 57-year-old man presenting with speech disturbance and ataxia. A, B. T2WI and FLAIR image shows hyperintense lesions in the pons, and inferior cerebellar peduncles (red arrows), and in the callosomarginal interface in the deep white matter, which is characteristic of MS. C, D. Hyperintense lesions are also seen in the midbrain, and the superior cerebellar peduncle (red arrows). Figure 16. PML. 25-year-old man presenting with right-sided weakness and headache. He has had a history of HIV infection. A. T2WI shows an isolated hyperintense lesion in the right middle cerebellar peduncle extending into the cerebellar hemisphere. B. Gd-enhanced T1WI shows this lesion as hypointensity with no enhancement. Figure 17. Low grade astrocytoma. 4-year-old boy presenting with autism. A, B. A mass lesion is located in the ventricular portion to the cerebellar portion of the left middle cerebellar peduncle. It is high signal on T2WI and low signal on T1WI and with no enhancement (not shown). This lesion can be removable by surgery. Figure 18. Acoustic schwannoma. 17-year-old female presenting with hearing loss and progressive ataxia. A, B. Axial T2WI and sagittal T1WI show an extra-axial cerebellopontine angle mass lesion which deviates the left middle cerebellar peduncle posteriorly and superiorly (red arrows). Figure 19. Neurofibromatosis type 1. 4-year-old girl presenting with developmental delay. A, B. T2WI and FLAIR image show multiple asymmetric lesions in the pons, middle and inferior cerebellar peduncles, and cerebellum. Figure 20. DAI. 29-year-old woman with DAI, presenting with loss of consciousness after motor vehicle accident. A. FLAIR image shows a hyperintense lesion in the left middle cerebellar peduncle to cerebellar hemisphere due to DAI. B. DWI shows hyperintense lesions in the corpus callosum and bilateral internal capsules, which is typical findings of DAI.