Cerebellar Signs
advertisement

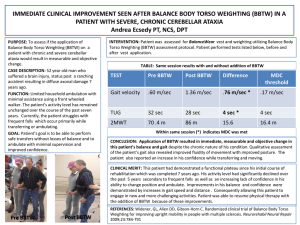
Cerebellar Examination Stem statement Giddiness, falls, unsteadiness Face, Speech, ULs and LLs Unilateral Upper limbs Screen for pronator drift, ensure patient can see your finger! Cerebellar signs Dysmetria with intention tremor Dysdiadochokinesia Dyschronometria Power for ataxic hemiparesis Sensory Temperature/Pain loss in syringomyelia and LMS Tone for cogwheel and leadpipe rigidity Skin for neurofibromatosis Pulse for AF Face Gaze evoked nystagmus (in the direction of gaze), INO, RAPD Speech (Count 1 to 20; British Constitution; West Register Street) Cerebellar speech – jerky, explosive and loud; irregular syllables CNs CPA LMS III nerve palsy in Benedikt’s syndrome Xanthelesma Lower limbs Dysmetria and intention tremor for toe to finger test Dyssynergia for heel-shin test Dysdiadochokinesia for foot tapping test DM dermopathy Sit up with hands folded and tests for pendular jerks Gait Broad based gait with veering towards the side of the lesion Request to test visual fields for hemianopia Bilateral Upper Limbs Cs of cerebellar (dysmetria, dysdiadochokinesia and dyschronometria) Sensory – loss of temperature/pain for syringomyelia Parkinsonism NF features Alcoholic features – dupytren’s contracture, stigmata of chronic liver disease Face CNs Bilateral CPA tumor Multiple sclerosis Eyes Gaze evoked nystagmus KF rings INO, RAPD Mouth Gingivial hypertrophy Macroglossia Telengiectasia Parotidomegaly Goitre Speech Cerebellar speech Hoarseness of voice Lower limbs Cerebellar signs Clawing of toes (Friederich’s ataxia) Sit – truncal ataxia and pendular jerks Gait – cerebellar gait Presentation Unilateral Sir, this patient has a right sided unilateral cerebellar lesion as evidenced by presence of a right dysmetria, dysdiadochokinesia and dyschronometria of the right upper limb. The right lower limb also demonstrates presence of right dyssynergia on heel shin test, with right dysmetria and intention tremor on toe-finger test and dysdiadochokinesia. This is associated with a gazed evoked nystagmus on rightward gaze with a broad based gait with veering towards the right. I did not detect any cerebellar speech or any truncal ataxia. There are no associated cranial neuropathies. In particular there was no evidence of any cerebello-pontine angle lesion with CN V, VI, VII and VIII intact. (There are also no signs of neurofibromatosis such as neurofibromas or café-au-lait spots.) There is also no evidence of lateral medullary syndrome or III nerve palsy to suggest Benedikt’s syndrome. There is also no pronator drift on the right to suggest a right ataxic hemiparesis. Patient is in sinus rhythm and not in atrial fibrillation with no xanthelesma or diabetic dermopathy. There are also no bruises to suggest overanticoagulation. There are no signs of Parkinsonism to suggest presence of multiple system atrophy. There are also no associated features of multiple sclerosis such as RAPD or INO. I would like to complete the examination by looking at 1. The patient’s temperature chart for fever (abscess in posterior fossa) 2. Visual fields for a left sided hemianopia, which can occur with a right posterior circulation stroke 3. I would also like to do a fundoscopy for papilloedema for a SOL in the right cerebello-pontine lesion as well as for optic atrophy from demyelinating disease. In summary, this patient has got an isolated right cerebellar lesion. The differential diagnoses include cerebral vascular infarction or haemorrhage or a space-occupying lesions such as a mitotic lesion or an abscess. Bilateral Sir, this patient has bilateral cerebellar lesions as evidence of dysmetria with intention tremor bilaterally associated with dysdiadochokinesia. Similar findings were also present on examination of the lower limbs. There is also presence of multi-directional gaze evoked nystagmus associated with a cerebellar speech, truncal ataxia and a broad based gait. There is no evidence of bilateral CPA lesion with no CN V, VI, VII and VIII abnormalities. Patient is in sinus rhythm and not in AF with no xanthelesma or diabetic dermopathy. There is no evidence of KF rings to suggest presence of Wilson’s disease. There is also no RAPD or INO to suggest multiple sclerosis. There is also no gingival hypertrophy to suggest chronic phenytoin use. Patient has no goitre or features of hypothyroidism such as a cream and peaches complexion, no hoarseness of voice or macroglossia. There are also no features of chronic ethanol ingestion such as Parotidomegaly, dupytren’s contracture or stigmata of chronic liver disease. There is no associated Parkinsonism signs to suggest multiple system atrophy such as presence of cog-wheeling or leadpipe rigidity. There are also no neurofibromas present to suggest presence of NF type 2. Patient is also not cachexic looking and there is no clubbing to suggest underlying malignancy. I did not detect any telengiectasia to suggest presence of Ataxia telengiectasia and there is pes cavus to suggest Friederich’s ataxia. (Think of Wilson’s, MS, Phenytoin, Hypothyroid, Alcohol, Parkinsonism, NF, paraneoplastic, telangiectasia and FA) I would like to complete the examination by 1. Looking at the temperature chart for fever 2. Performing a neurological examination of the lower limb to look for spastic paraparesis 3. I would also like to do a fundoscopy for Optic atrophy, which may suggest demyelinating disease. In summary, this patient has bilateral cerebellar syndrome. Possible causes include drugs such as phenytoin, metabolic conditions such as hypothyroidism, chronic ethanol ingestion, paraneoplastic conditions and infection such as enteroviruses and bilateral cerebellar strokes. Questions What are the differential diagnoses for a unilateral cerebellar syndrome? Isolated Cerebrovascular accident – infarction or haemorrhage SOL in posterior fossa – abscess or mitotic (primary vs secondary) Associated CN CPA and/or neurofibromatosis Lateral medullary syndrome Jugular foramen (Arnold-Chiari or Dandy-Walker) Benedikt’s syndrome Ataxic hemiparesis (lacunar stroke) Parkinsonism in Multiple system atrophy Demyelinating such as Multiple sclerosis What are causes of bilateral cerebellar syndrome? Acquired Infection Viral – HIV, Enteroviruses Spirocheatal – Lymes and Tabes dorsalis Others – Toxoplasmosis and CJD Metabolic Wilson’s disease Hypothyroidism Drugs Phenytoin and Carbamazepine Lithium Alcohol Causes bilateral cerebellar signs Causes isolated lower limb cerebellar signs Affects the anterior vermis Due to thiamine deficiency Multiple system atrophy Neurofibromatosis type 2 with bilateral CPA tumor Bilateral Strokes Paraneoplastic – Ca lung or ovary Hereditary Ataxia telangiectasia Autosomal recessive Childhood with death by 20s or 30s Ataxia, choreathetosis and telengiectasia on the face, eras and conjunctiva and skin crease Low IgA with recurrent chest infections and lymphoreticular malignancy Friederich’s ataxia Scoliosis, pes cavus Spastic paraparesis, dorsal column loss, absent ankle jerks What are the signs of a midline lesion (cerebellar vermis) and what are the causes? Signs : truncal ataxia, abnormal heel-toe walk test, cerebellar speech Causes : Midline tumor, paraneoplastic What are the causes of cerebellar signs with spastic paraparesis? Friederich’s ataxia Spinocerebellar ataxia Arnold-Chiari Malformation Lesion at the craniospinal junction eg meningioma Syringomyelia Multiple sclerosis Syphilitic meningomyelitis How are cerebellar signs located? Limb ataxia = cerebellar lobes Gait ataxia = anterior vermis Truncal ataxia = posterior vermis What are the differences between cerebellar and sensory ataxia? Cerebellar Sensory Site Cerebellar Posterior column, nerves Tone Reduced Normal Reflexes Normal or pendular Reduced Sensory Normal Reduced Sphincter disturbance Nil Affected when posterior column involved; overflow incontinence How would you investigate? Imaging – MRI brain Blood tests according to the causes How would you manage? Depends on underlying cause