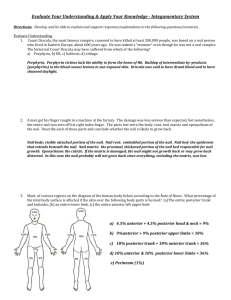
Nail bed deformities
advertisement

NAIL BED DEFORMITIES Anatomy common volar digital artery sends a large branch into the pulp of the tip at the level of distal phalanx and another branch parallel to the paronychium. There is a consistent branch to the proximal nail fold (superficial arcade) and then multiple small fine branches going into the nail bed (subungual arcade) as the vessel traverses distally small veins of the fingertip do not follow the volar digital artery as vena concomitants but progress proximally in a more random fashion. The distal arch is formed by veins running from the distal pulp and along the lateral nail wall onto the dorsum of the finger distal to the distal interphalangeal joint. All veins, even those less than 0.1 mm in diameter, have been found to have valves, except for the arches Although the artery at the level of the proximal nail bed is large enough to anastomose with the microscope, vein size is often not large enough for anastomosis until the DIP joint is approached Just proximal to the base of the nail fold the nerve splits, sending branches into the pulp of the finger and dorsally into the nail bed. Nail has a high concentration of glomus bodies Hyponychium plug of keratinous material situated beneath the distal edge of the nail where the nail bed meets the skin of the fingertip has been reported that there are more lymphocytes and polymorpholucocytes per area volume here than at any other site in the body Panonychium has no known anatomical function but may contribute to stability of the nail and its adherence to the fingertip. Nail production nail itself is made up of onchyn, which is a keratinous material and is produced by the death of the germinal cells as they are pressed upward into the nail nail grows 0.1 mm per day a 21-day delay in distal growth of the nail after injury, during which time it apparently thickens proximal to the injury site. The increased formation lasts 50 days and then is less (thinner nail) for a subsequent 30 days. This means that the nail growth is not normal in speed or thickness for approximately 100 days Nails, as a rule, grow four times more rapidly on the finger than they do on the toes. They grow faster in summer than in winter, more rapidly the longer the finger and more rapidly in nail biters Nail has portions produced in three areas of the perionychium Germinal matrix begins 1mm distal to the insertion of the extensor tendon to the lunula on the ventral floor Produces 90% of the nail volume The direction of the germinal matrix decides the direction of nail growth The process by which cells duplicate and become flattened and pressed upwards and forward while retaining nuclei is known as gradient parakeratosis. sterile matrix, (distal to the lunula) adds to the nail volume(making up for surface wear) and aids nail adherence, In the proximal portion of the dorsal roof, material is produced by macrocytosis and nucleolysis (similar to the sterile matrix) that flows onto the dorsum of the nail produced by the germinal matrix and produces the shine on the nail. If the dorsal roof is totally removed, the shine will be lost from the dorsum of the nail and an irregular surface may result If the eponychium is excised or traumatically avulsed, it may be replaced by eponychial tissue from a toe to restore shine and smooth surface to the dorsum of the finger. On the fingers the germinal matrix essentially extends into the nail fold at the same width as at the paronychium; however, on the toes (particularly the large toe) the germinal matrix becomes wider as it goes into the nail fold . The anatomical significance is evident when attempts are made to extirpate the large toenail or a side of it for ingrown toenail. Ganglions originating from the distal interphalangeal joint and encroaching on the germinal matrix may cause nail grooving or disruption. ACUTE INJURIES HISTORY AND EXAMINATON Mechanism of injury Sensation circulation tendon laceration and rupture X-rays Occupation and hobbies Handedness Personal preference of the patient ESSENTAILS OF NAIL BED REPAIR Accurate reapproximation of the matrix The sterile matrix should not be used for covering the defect of pulp skin The defect of the sterile matrix should be covered by a split thickness sterile matrix graft or full thickness graft The defect of the germinal matrix should be covered by full-thickness skin graft (these usually require secondary repair) Matrix graft from the toe Avoid adhesions b/w the proximal and lateral nail folds with the nail bed by inserting the original nail or an artificial stent HAEMATOMA WITHOUT NAIL DISLOCATION OR # Trephination - 18 gauge needle of heated paper clip treatment of subungual hematoma has been somewhat controversial. Up until recently, with subungual hematomas greater than 25% to 50%, recommendation has been to remove the nail plate and repair any underlying nail bed laceration. However, recently two studies have questioned this recommendation Nail bed repair not necessary for those with subungual hematoma if 1. nail plate is still partially adherent and is not displaced out of the fold 2. At most an undisplaced simple fracture 3. intact nail margin – no periungual skin laceration COMPLEX LACERATION Remove nail, reduce # and repair nail matrix 6.0 catgut 8.0 vicryl replace avulsed matrix as a graft can take split sterile matrix from the same finger or toe if >50%, consider split thickness matrix graft from large toe. if no suitable donor then use FTSG DEFECT OF THE GERMINAL MATRIX transverse defect o if distal defect then consider a split thickness sterile matrix from adjacent undamaged matrix o if middle part defective then the distal part of the germinal matrix can be transposed as a graft and the secondary defect SSG longitudinal defect o more then 2/3 the width of the matrix the nail fold, sterile matrix and fold should be extirpated and the defect covered by a flap o if less than 2/3 close then primary defect with a matrix flap and the secondary defect with a FTSG or SSG (matrix) o may require revision surgery Germinal matrix grafts need to be full thickness. Best donor = lateral sides of great toe. Donor site left to heal by secondary intention Nail deformities Aetiology 1. Nail biting 2. Trauma 3. Infection 4. Tumor a. Ganglion b. Paronychia 5. overzealous manicuring of the eponychium a. leads to loss of cells in the dorsal roof from trauma and allergic response to the glue b. process of adhering an artificial nail to the dorsum of the fingernail consists of cleaning the nail, partially elevating the nail vest or eponychial fold, and gluing the prosthesis onto the surface. Eponychial loss Nail loses shine Options 1. full thickness composite graft from great toe eponychium 2. local skin flap and placing a split-thickness sterile matrix graft on the deep surface of the flap to reestablish function of the fold. Eponychia pterygium insert silicon sheet under dorsal roof. If persistent, resurface with a SSM graft Onycholysis (nonadherence) Often due to an underlying scar which are transverse or diagonal and wide many causes, including macro- and microtrauma, irritation, dissolving of the eponychial plug (eg, with alkali, acid, liquids), increasing age, onychomycosis (ie, fungal infections), and overproduction of sterile matrix keratin Observation first – often improves. a nail requires three or four growth periods (about 1 year) to improve in shape, volume, and appearance If not, split thickness matrix graft from adjacent matrix or from toe. Ridged Nails occur longitudinally from scar buildup in or beneath the matrix, with the nail assuming the contour of the matrix. Transverse ridges are caused by regrowth after trauma or hypoxia (eg, pneumonia, long-duration arm tourniquets) – does not need treatment Treated by excision of the scar or smoothing the irregularity of the bone Split Nail longitudinal scar frequently causes a split in the nail because the scar tissue cannot produce a nail and the prying and pulling of the nail on either side causes the weakened nail to crack or split along the scar line. Treatment involves scar excision o Direct closure o split thickness sterile matrix and/or z-plasties o if in germinal matrix, need full thickness graft (split thickness does not produce nail) Double Nail Double nail (ventral and dorsal) from scar in germinal matrix A horizontal scar in the germinal matrix can create a double nail volumes of the dorsal and volar portions are determined by the location of the scar The farther proximal the scar is, the thinner the dorsal fragment of the nail. If the dorsal portion is thin, then the germinal matrix that produces it should be excised, leaving behind the volar portion as the new nail If the dorsal portion is thin, then the germinal matrix that produces it should be excised, leaving behind the volar portion as the new nail If both portions are equal or if the dorsal is thicker, the scar must be excised and grafted to reestablish a single nail unit. Hyponychial barrier loss Nonadherence due to dissolution of the hyponychial plug by alkali, acid, or fluid that allows bacteria, fungus, or dirt access to the subungual space, is treated by eliminating the cause and allowing the nail to re-adhere. If this does not occur, the nail should be removed to a point just proximal to the area of nonadherence, the nail bed surface should be scraped to remove the keratinous material and the nail allowed to grow distally and to re-adhere. Removal and scraping may need to be performed more than once until the attached nail reaches the desired length. Pterygium of the hyponychia area may occur with SLE or dermatomyositis pad of finger becomes atrophic and hyponychial attachment painful/tender Treat by removing 3-4mm of distal nail and nail bed, resurface with SSG/FTSG Bone irregularities Irregularities of the distal phalanx cause disruption of the flat surface of the dorsal bone and nail bed, which results in nail deformities o Trauma o Tumors 1. Osteophytes 2. ganglions 3. enchondromas Aim to smoothen the bone Fish-mouth incision distal to hyponychia fold and eleveta nail matrix off the phalanx Nail absence Congenital or acquired microvascular transfer o the most reliable method of replacement Nonvascularized composite grafts o less reliable but require less time and expense and produce less scarring osseointegrated fixation of an artificial nail Camouflage o area that is similar in shape and size to the missing nail may be deepithelialized and replaced with a split thickness skin graft o An arc of full-thickness skin graft placed distally (hyponychium) and proximally (lunula) may be used Hooked nail – parrot beaked deformity Due to a volar curvature of the nail bed distally Often due to tight closure of a fingertip amputation and/or loss of distal nail support Options 1. shorten the bone and/or add tissue to tip o cross finger flap o composite pulp graft from toe 2. add support o tip bone graft with soft tissue flap – tends to resorb and thus recur o free vascularised pulp and bone flap used – complex o antenna technique (Tonkin, J Hand Surg Br 2004) i. free tethered pulp ii. free tethered nail bed and splint it with longitudinal K-wires inserted into the terminal phalanx iii. reconstruct the pulp by covering the defect with a cross-finger flap. iv. K wires removed at 3 weeks Pincer Nail deformity /Trumpet nail Exact cause unknown - but have been attributed to trauma, tight shoes, and heredity. characterized by a progressive transverse tubing of the nail 60% of individuals have eventual pain in the nail and fingertip, and the nail bed may become vascularly compromised as the nail tubes transversely. thumb or great toe is the most commonly involved digit, and the deformity may be unilateral or bilateral. May be due to curvature of the germinal matrix over the narrow part (waist) of the distal phalanx Xray should be done of the distal phalanx surface to eliminate ganglion, osteophytes, or tumors as causes of the tubing. Excision of the paronychium bilaterally, as is done with ingrown nails, can be effective; however, most individuals do not want their nails significantly narrowed Best option o freeing the paronychium from the periosteum of the bone, elevating it into normal lateral position, and maintaining it with autograft or allograft dermis (Alloderm) Chronic paronychia chronic inflammatory condition of the lateral nail fold and eponychium predisposing conditions- repetitive paronychial trauma and exposure to moisture or contact irritants. Bartenders, housewives high risk More common in diabetics, psoriasis fingers of the dominant hand are more commonly involved Inflammation results, the seal between the nail plate and nail fold becomes broken, and the nail bed cul-de-sac becomes inoculated with various organisms, most significantly Candida albicans usually nonpurulent and associated with candida (found in 70% of cases), gramnegative organisms, or both Progressive fibrosis, recurrent infections and nail deformity (grooving, thickening, nail plate waves) can result if the germinal matrix is involved Treatment i. Prevention o Avoidance of trauma, moisture, or irritants, particularly at work, o wear light cotton gloves under heavy waterproof gloves o Cosmetic nail products of all kinds should be avoided. o Avoid manicures ii. Antifungals o Topical antifungals effective against Candida, such as clotrimazole and ketoconazole should be applied twice a day in the groove between the nail plate and proximal nail fold o Oral antifungals such as terbinafine, itraconazole, and ketoconazole may be necessary in cases that are resistant to topical therapy. iii. Surgery o When thickened fibrotic diseased tissue does not allow adequate delivery of topical or systemic antifungal o two most commonly used procedures used for chronic paronychia are marsupialization of the nail fold (Keyser-Eaton procedure) and complete excision of the entire nail fold. Keyser-Eaton procedure crescent excision of the proximal nail fold from 1 mm proximal to the nail fold at a maximal width of about 6 mm; the cuticle is preserved uninjured germinal matrix remains exposed, allowing adequate drainage as dressing changes continue for about two weeks until re-epithelialization occurs. 6% recurrence rate Complete excision of nail fold Will result in dull nail and relative lengthening of the lunula Nail bed tumors Benign 1. pyogenic granuloma o usually due to perforations through the nail 2. subungual nevi 3. subungual fibroma (tuberous sclerosis) 4. inclusion cysts 5. glomus tumor 6. ganglion 7. viral warts 8. giant cell tumors Malignant 1. BCC- very rare 2. SCC a. most common malignant tumor of the perinychium b. mostly secondary to radiation 3. subungual melanoma