UPPER RESPIRATORY TRACT INFECTIONS
advertisement
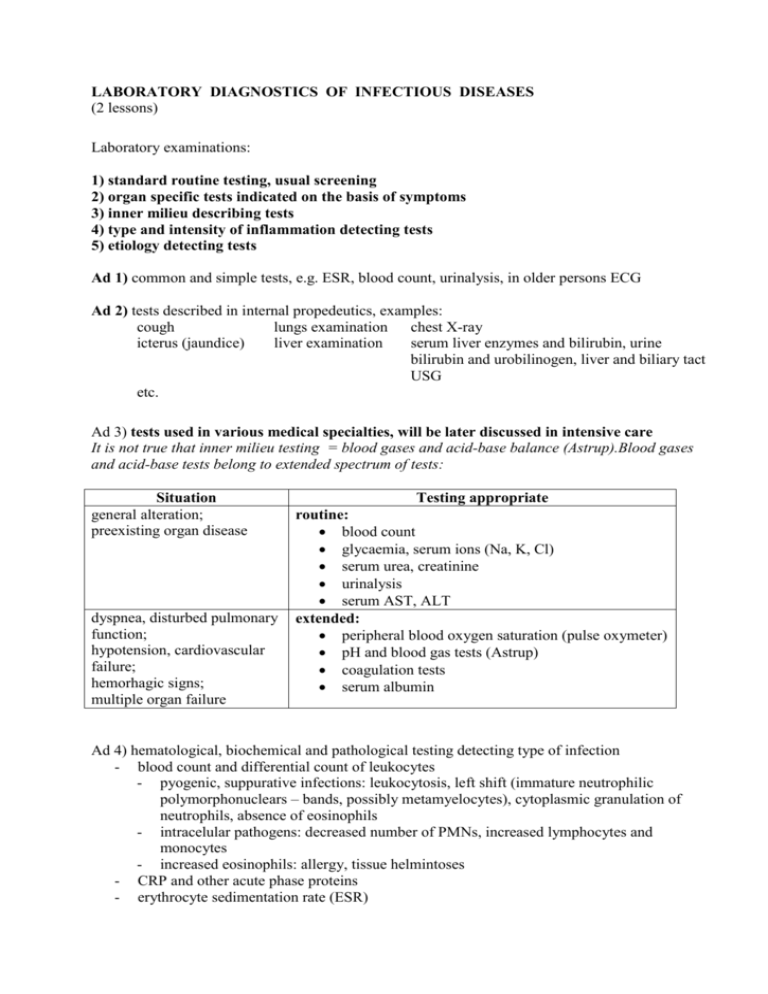
LABORATORY DIAGNOSTICS OF INFECTIOUS DISEASES (2 lessons) Laboratory examinations: 1) standard routine testing, usual screening 2) organ specific tests indicated on the basis of symptoms 3) inner milieu describing tests 4) type and intensity of inflammation detecting tests 5) etiology detecting tests Ad 1) common and simple tests, e.g. ESR, blood count, urinalysis, in older persons ECG Ad 2) tests described in internal propedeutics, examples: cough lungs examination chest X-ray icterus (jaundice) liver examination serum liver enzymes and bilirubin, urine bilirubin and urobilinogen, liver and biliary tact USG etc. Ad 3) tests used in various medical specialties, will be later discussed in intensive care It is not true that inner milieu testing = blood gases and acid-base balance (Astrup).Blood gases and acid-base tests belong to extended spectrum of tests: Situation general alteration; preexisting organ disease dyspnea, disturbed pulmonary function; hypotension, cardiovascular failure; hemorhagic signs; multiple organ failure Testing appropriate routine: blood count glycaemia, serum ions (Na, K, Cl) serum urea, creatinine urinalysis serum AST, ALT extended: peripheral blood oxygen saturation (pulse oxymeter) pH and blood gas tests (Astrup) coagulation tests serum albumin Ad 4) hematological, biochemical and pathological testing detecting type of infection - blood count and differential count of leukocytes - pyogenic, suppurative infections: leukocytosis, left shift (immature neutrophilic polymorphonuclears – bands, possibly metamyelocytes), cytoplasmic granulation of neutrophils, absence of eosinophils - intracelular pathogens: decreased number of PMNs, increased lymphocytes and monocytes - increased eosinophils: allergy, tissue helmintoses - CRP and other acute phase proteins - erythrocyte sedimentation rate (ESR) Dynamics of inflammatory parameters in the course of bacterial infection. Ad 5) microbiology diagnostics and clinical interpretation a) Direct methods of pathogen identification - microscopy: light, electron, ... - culture: aerobic vs. anaerobic, on selective media, ... - antigen detection: clearview, latexagglutination, .... - molecular genetic methods: PCR, genetic probes, ... Method microscopy culture antigen detection specific genome detection Contribution morphology and number of microbes in sample; microbes-leukocytes and microbes with each other interrelationship features of isolated agents; complete identification; sensitivity testing; storage for future testing detects presence of the searched agent detects presence of the searched agent Advantages quick, easy, cheap; low demands on equipment easy, cheap; low demands on equipment easy, cheap, quick; low demands on equipment quick; high sensitivity Disadvantages inappropriate in processing of high quantity of samples; good experience needed; only some microorganisms can be detected on the basis of morphology risk of selective identification of only some microbes; danger of laboratory infection; prolonged testing – some pathogens grow slowly low sensitivity; with some samples also low specificity expensive; expensive equipment needed; easy contamination b) Indirect methods of pathogen identification - serology: agglutination, hemagglutination, hemagglutination inhibition, complementfixation, enzyme-linked immunosorbent assay (ELISA), Western blot etc. - skin tests: tuberculin test (PPD test, Mantoux II) - detection of lymphocyte sensibilisation (TB diagnostics) Method specific antibodies detection skin tests Contribution detects antibody response detects specific cell-mediated immunity Advantages easy, cheap; appropriate for routine processing easy, very cheap specific cell- detects specific more precise, no risk Disadvantages inappropriate for identification of agents with high antigenic variability low reliability; risk of allergic reaction; may induce patient immunisation – not possible to repeat much more expensive than mediated immunity detection cell-mediated immunity of allergy or patient immunisation skin test Serological tests interpretation: acute infection: chronic infection: single sample testing (IgM vs. IgG) paired sera testing (fourfold elevation of specific antibody titres) dynamics of antibody titres in time antibodies avidity testing (the strength of Ab-Ag bind) Indirect detection methods are based on the detection of specific immune response to infection: general advantages: can differentiate infection and colonisation can detect infection that already passed general limitations: cannot be used in acute and quickly progressing infections (specific immunity occurs after 1-3 weeks) not reliable in local infections (e.g. on mucosal surface only) fail in immunocompromised persons UPPER RESPIRATORY TRACT INFECTIONS (1 lesson) Introduction, pathophysiology - antiinfective defense of the respiratory tract - respiratory tract as a continuum, involvement of its parts ranging from nose to trachea - closely related structures (conjunctiva, paranasal sinuses, middle ear) - inflammatory edema of respiratory tract mucosa and submucosal lymphatic tissue Etiology: - physiological bacterial colonization of the upper respiratory tract - respiratory viruses: rhinoviruses, coronaviruses, influenza and parainfluenzaviruses, RSV - pathogenic bacteria: nasal mucosa: Staphylococcus aureus nasopharynx: Streptococcus pyogenes, corynebacteria, anaerobes epiglottis and below: H. influenzae and other gramnegative nacteria sinuses (sinusitis, otitis): various agents – viruses, bacteria, fungi Syndromes and etiology: - acute rhinitis, coryza, common cold: viruses - acute pharyngitis and tonsillitis: viruses, bacteria - acute laryngitis: viruses - acute epiglottitis: H.influenzae - acute tracheitis: viruses Complications: - sinusitis - otitis media, mastoiditis - peritonsillar abscess Separatelly discussed diaseases: - influenza - infectious mononucleosis - diphtheria Diagnostics, differentiation of viral and bacterial disease: - inflammatory parameters - tests for etiology detection - bacterial infection, viral infection - complementary and syndrome-specific tests URINARY TRACT INFECTIONS (1 lesson) Pathogenesis of urinary tract infections - route of infection: ascending infection, hematogenous infection per continuitatem – very rare - predisposing factors: - anatomical factors (short uretra in females, congenital defects...) - mechanical obstruction from inside (lithiasis, tumours, scarring and postoperative strictures) and from outside (prostatic hypertrophy, tumours, pregnancy) - functional neuromuscular defects (paraplegia, sclerosis multiplex, spina bifida) - metabolic factors (diabetes mellitus) - microbial pathogenic factors: - adherence to uroepithelium, colonisation (hemolytic E.coli) - biofilm production (catheters, chronic infection) - tissue invasion Classification of UTI with regard to etiology and pathogenesis: - community-acquired UTI - cystitis, pyelonephritis – E.coli, Proteus mirabilis - urethritis, prostatitis – Mycoplasma, Chlamydia, Neisseria gonorhoae - chronic UTI in diabetic patients - besides Gramnegative bacilli frequently Enterococcus - hospital-acquired UTI - commonly associated with permanent catheterisation or endoscopy (cystoscopy) - etiology: multiresistant Gramnegative bacilli (Pseudomonas, Enterobacter, Klebsiella) Examination procedure - physical examination - laboratory testing: - inflammatory parameters (blood count + differential count of leukocytes, CRP) - biochemical testing of urine, urine culture - blood culture if pyelonephritis suspected - renal function testing (urea, creatinine in serum - imaging techniques: ultrasonography mostly sufficient Clinical classification of UTI Upper urinary tract infection (easy progression to sepsis) - acute pyelonephritis and chronic pyelonephritis - interstitial nephritis - renal absces, pararenal absces Lower urinary tract infection - cystitis - urethritis - prostatitis Treatment of UTI - symptomatic therapy, fluid intake - antibiotic therapy CENTRAL NERVOUS SYSTEM INFECTIONS (1 lesson) Classification of CNS infections, terminology: • structure most involved: meningitis, encephalitis, myelitis, radiculitis, neuritis type of inflammation: purulent x nonpurulent, aseptic pathogen: bacterial, viral, fungal, parasitic extent of inflammation: difusse - meningitis, meningoencephalitis, encephalitis focal – necrotising encephalitis (HSV), cerebritis, abscess course of disease: acute x chronic Pathogenesis: - invasion of CNS - via blood (blood-brain, blood-cerebrospinal fluid barrier) - via direct spreading from adjacent structures - via peripheral nerves - response of CNS to bacterial and viral invasion - brain edema Clinical manifestations and etiology of CNS infections: - meningeal syndrome (headache, vomitus, meningeal signs), fever, coma - examination of meningeal signs - symptoms of encephalitis - purulent meningitis - clinical presentation - etiology (pneumococcus, meningococcus, listeria, other agents) - aseptic meningitis, meningoencephalitis - clinical presentation - etiology (tick-borne encephalitis, respiratory viruses, borrelia, leptospira) Diagnostics: - diagnosis of CNS inflammation and type of inflammation lumbar puncture, cerebrospinal fluid testing and findings - detection of etiology – dirrect and indirrect methods Basic principles of treatment: - causative therapy - symptomatic therapy (including brain edema therapy) - risk of delayed diagnosis (meningococcal invasive disease, purulent meningitis, necrotising encephalitis) IMPORTED INFECTIONS (1 lesson) Basic features of imported diseases - infections of cosmopolitan occurrence - infections limited to tropical and subtropical climate Danger: delayed diagnosis risk of spreading Diseases obligatory reported to WHO: variola, cholera, plague, haemorhagic fevers, SARS The most important syndromes in imported diseases: fever: malaria, typhoid fever, dengue fever, haemorrhagic fevers, amebiasis diarhea: food-poisoning bacterial etiology (except pathogens common in middle Europe): enterotoxigenic E. coli (ETEC), shigellae, V. cholerae parasitic etiology: Entamoeba histolytica, Giardia intestinalis, Trichuris trichuria, Ancylostoma duodenale icterus: viral hepatitis (A,E,B), yellow fever leptospirosis amebic liver abscess, echinococcosis, schistosomosis exanthema: disesases eliminated by vaccination in developed countries (measles, rubella) diseases limited to tropical and subtropical climate (dengue, rickettsiosis, haemorrhagic fevers, larva migrans cutanea) Examination of traveller: history including detailed travell history physical examination, „dominant symptom“ laboratory tests: basic screening + special tests with respect to the suspected diagnosis Malaria endemic area malaric plasmodia: Plasmodium vivax, ovale, malariae, falciparum life cycle of plasmodium, insect vector (Anopheles mosquito) clinical manifestation: attack of fever fever patterns – tertian, quartan, tropical (falciparum) malaria danger of falciparum malaria diagnostics: microscopy - thick smear, thin smear of blood treatment and prevention, increasing resistance to antimalarial drugs EXANTHEM OF INFECTIOUS ORIGIN (2 lessons, slide show) Introduction, terminology: exanthem (skin), enanthem (mucosal surfaces) infectious diseases with exanthem as an obligatory symptom and facultative symptom pathogenesis of exanthem Examination of patient with rash: morphological classification of the rash, distribution, pattern of progression, timing history: vaccination, travelling abroad, known allergy morphologic types of skin lesions: macula, papula, nodule, vesicle, bulla, pustula Morphologic classification of exanthems, representative diseases: 1. macular and/or papular exanthem: scarlet fever (scarlatina) measles (rubeola, morbilli) German measles (rubella, rubeola) Fifth disease (erythema infectiosum) Sixth disease (exanthema subitum, roseola infantum) dif. dg. allergic reaction 2. vesicular and pustular exanthem: generalized: chickenpox (varicella) smallpox (variola) localized: herpes zoster herpes simplex impetigo 3. petechial purpuric eruptions: rickettsiosis – purpuric fever infections associated with disseminated intravascular coagulopathy: meningococcal invasive disease viral hemorrhagic fevers severe sepsis Falciparum malaria