Isolated VI Nerve Palsy
advertisement

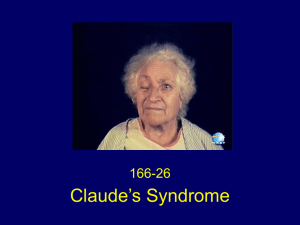
Isolated VI Nerve Palsy Examination (Examine patient’s eyes, CNs) Complete the eye examination Rule out MG, thyroid Rule out Cavernous Sinus syndrome, Superior orbital fissure syndrome Proceed to check cranial nerves V, VII and VIII for CPA tumor XI, X, XI, XII for any base of skull lesions Examine upper limbs Hemiplegia (long tract signs suggesting brainstem) Cerebellar signs (CPA lesion, Miller Fisher usually truncal and gait) Reflexes for areflexia (Miller Fisher) Examine the neck for LNs and mastoid for tenderness (Gradenigo’s syndrome) Request Fundoscopy (papilloedema from raised ICP, optic atrophy for MS) Field testing (bitemporal hemianopia) Acuity (reduced in orbital lesions) Corneal testing for reduced sensation form V1 involvement BP Urine dipstick Temperature chart for fever(meningitis) Ask for retrobulbar pain Presentation Sir, this patient has an isolated right sided VI nerve palsy as evidenced by Convergent strabismus at primary gaze Failure of abduction of the right eye With diplopia where the image is side by side and furthest apart on rightward gaze, with disappearance of the outer image on covering the right eye. This suggests a right lateral rectus muscle weakness and hence a right VI nerve palsy. There is no evidence of a III or IV or V1 palsy which may suggest cavernous sinus or superior orbital syndrome. There is also no involvement of the VII or VIII nerve palsy and no cerebellar signs to suggest A CPA lesion There are no associated CN lesions of IX to XII and no enlarged Cx LNs. There is no fatiguibilty to suggest MG and no thyroid eye signs. There are no enlarged LNs or tender mastoid. There is also no hemiparesis, no cerebellar signs and reflexes are present. I would like to complete my examination by: Fundoscopy (papilloedema from raised ICP, optic atrophy for MS, DM or hypt changes) Field testing (bitemporal hemianopia) Acuity (reduced in orbital lesions) Corneal testing for reduced sensation form V1 involvement BP Urine dipstick Temperature chart for fever(meningitis) Ask for retrobular pain In summary, this patient has an isolated right sided VI nerve palsy. The aetiology includes…. Questions What is the course of the VI nerve? Nucleus of CN VI located in the pons, sending motor neurons supplying the lateral rectus muscle of the ipsilateral eye; also internuclear neurons that project (via MLF) to medial rectus subdivision of contralateral oculomotor (CN III) nucleus (ie lesion of nucleus causes ipsilateral horizontal gaze palsy) nerve fascicles exit the pons anteriorly and course through subarachnoid space where it runs a vertical (upward) course, along ventral surface of pons (confined by adjacent AICA) pierces dura overlying clivus, entering into Dorello's canal, contacting tip of petrous pyramid (part of temporal bone; adjacent to mastoid air cells) enters the cavernous sinus after passing through the petroclinoid (Gruber's) ligament runs in body of sinus (rather than lateral wall where CN III, IV, V located) along foramen lacerum (near internal carotid artery) enters orbit via superior orbital fissure and shortly thereafter pierces lateral rectus muscle What are the causes of a unilateral VI nerve palsy? Brainstem (Pons)– infarct, haemorrhage, abscess, demyelinating (look for VI and VII palsies due to close proximity) Aneurysm (ectatic basilar artery) Meningitis Infective – TB, Fungal, HIV, Syphilis, Lyme Mitotic – leptomeningeal carcinaomatosis, secondaries(NPC), lymphoma, radiotherapy Sarcoidosis Trauma CPA lesions Petrous temporal bone (Gradenigo’s syndrome) Cavernous sinus syndrome Superior orbital syndrome Miller Fisher syndrome Mononeuritis multiplex DM, hypertension MG Raised ICP NB: - most common aetiology of isolated abducens lesion is post-viral in children and ischemia / infarction (eg diabetic) in adults What are the causes of bilateral VI nerve palsy? Leptomeningeal causes (see above) Miller Fisher syndrome Mononeuritis multiplex MG Raised ICP Wernicke’s encephalopathy (Ophthalmoplegia, confusion and ataxia a/w Korsakoff’s psychosis from thiamine deficiency) What are the syndromes associated with VI nerve palsy? Central Raymond’s syndrome – ipsilateral VI with contralateral hemiparesis Millard-Gubler syndrome – Ipsilateral VI and VII with contralateral hemiparesis Peripheral Gradenigo syndrome – inflammation of the tip of the petrous bone from mastoiditis; VI and V(gasserian ganglion therefore ipsilateral pain) and VII CPA Cavernous sinus Superior orbital Congenital Mobius syndrome (VI with facial diplegia) Duane’s syndrome (Congenital absence of VI nuclei with III nuclei innervating the lateral recti; orbit retraction on adduction and protrusion on abducting How do you evaluate diplopia? Evaluation of diplopia follows 3 rules o The double vision is maximal in the direction of gaze in the affected muscle o The false image is the outer image o The false image arises form the affected eye What is Cavernous sinus syndrome? Lesion in the cavernous sinus leading to Ophthalmoplegia, V1, Horner’s, proptosis, chemosis and pain Causes include carotid aneurysm, carotid-cavernous fistula, tumour and thrombosis, Tolosa Hunt syndrome What is superior orbital fissure syndrome? Lesions occurring at the superior orbital fissure leading to Ophthalmoplegia, V1, Horner’s, proptosis, chemosis, pain and Optic Nerve Causes includes meningiomas, hemangiomas and thyroid eye disease, Tolosa Hunt syndrome What is Miller Fisher syndrome? Triad of ophthalmoplegia, ataxia and areflexia Cs by present of anti GQ1B antibodies Variant of GBS What are the causes of mononeuritis multiplex? Endocrine – DM, hypt AI – Churg Strauss, Wegener’s, PAN, Sjogren’s, RA, SLE Infective – Lyme, leprosy Infiltrative – Amyloid, sarcoid How would you investigate? Blood tests fasting glucose, ESR, ANA, VDRL Imaging CT brain or MRI brain Vascular imaging if proptosis / chemosis looking for dural carotid-cavernous fistula or cavernous sinus thrombosis Examine CSF (also if systemic illness, immunocompr, bilateral, other CN deficits) 8-30% will remain cryptogenic after work-up How would you manage? Education on Px if ischaemic (see below) and Ix and avoid driving, climbing high places and operating heavy machinery Treat underlying cause Example control DM and BP Symptomatic treatment Patch Prism If chronic, chemodenervation with botox or strabismus surgery What is the prognosis? most either spontaneously improve or have underlying lesion found ischemic palsies almost always recover completely in 2-4 months while some recovery seen in half of traumatic cases (but take over one year) if no recovery over 3-6 months then suspect underlying lesion such as tumour few may have chronic isolated abducens palsy of unknown cause follow regularly looking for emergency of new localizing signs and ensure adequate neuroimaging and ENT evaluation