Quality of life of 319 patients with bladder cancer undergoing
advertisement
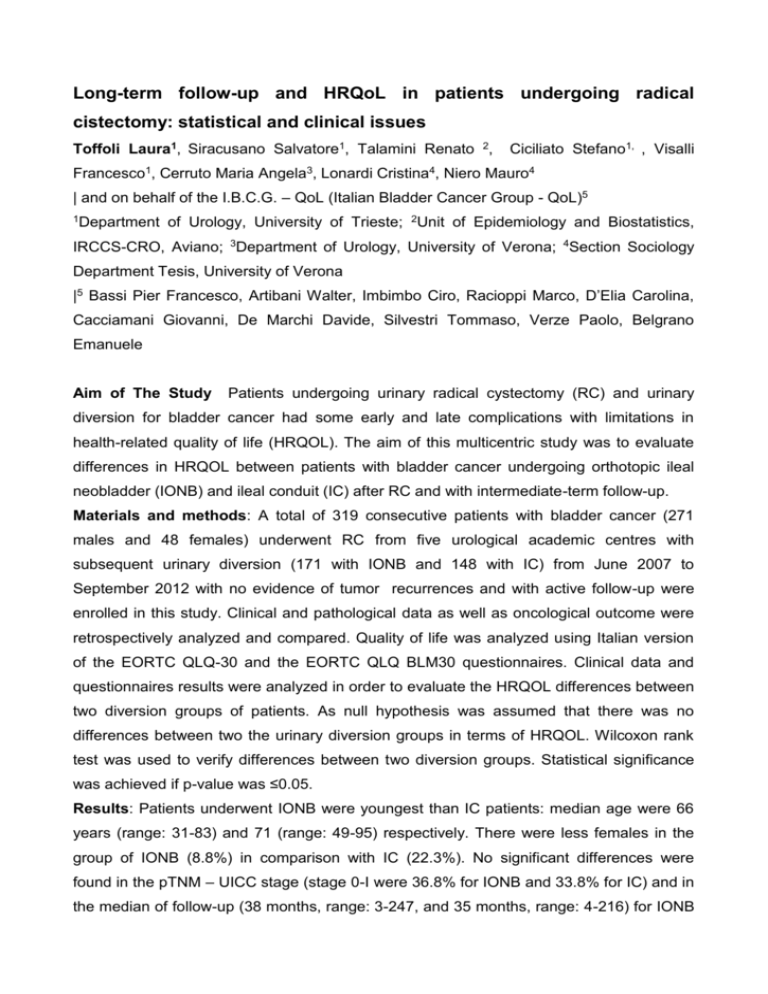
Long-term follow-up and HRQoL in patients undergoing radical cistectomy: statistical and clinical issues Toffoli Laura1, Siracusano Salvatore1, Talamini Renato 2, Ciciliato Stefano1, , Visalli Francesco1, Cerruto Maria Angela3, Lonardi Cristina4, Niero Mauro4 | and on behalf of the I.B.C.G. – QoL (Italian Bladder Cancer Group - QoL)5 1Department of Urology, University of Trieste; 2Unit of Epidemiology and Biostatistics, IRCCS-CRO, Aviano; 3Department of Urology, University of Verona; 4Section Sociology Department Tesis, University of Verona |5 Bassi Pier Francesco, Artibani Walter, Imbimbo Ciro, Racioppi Marco, D’Elia Carolina, Cacciamani Giovanni, De Marchi Davide, Silvestri Tommaso, Verze Paolo, Belgrano Emanuele Aim of The Study Patients undergoing urinary radical cystectomy (RC) and urinary diversion for bladder cancer had some early and late complications with limitations in health-related quality of life (HRQOL). The aim of this multicentric study was to evaluate differences in HRQOL between patients with bladder cancer undergoing orthotopic ileal neobladder (IONB) and ileal conduit (IC) after RC and with intermediate-term follow-up. Materials and methods: A total of 319 consecutive patients with bladder cancer (271 males and 48 females) underwent RC from five urological academic centres with subsequent urinary diversion (171 with IONB and 148 with IC) from June 2007 to September 2012 with no evidence of tumor recurrences and with active follow-up were enrolled in this study. Clinical and pathological data as well as oncological outcome were retrospectively analyzed and compared. Quality of life was analyzed using Italian version of the EORTC QLQ-30 and the EORTC QLQ BLM30 questionnaires. Clinical data and questionnaires results were analyzed in order to evaluate the HRQOL differences between two diversion groups of patients. As null hypothesis was assumed that there was no differences between two the urinary diversion groups in terms of HRQOL. Wilcoxon rank test was used to verify differences between two diversion groups. Statistical significance was achieved if p-value was ≤0.05. Results: Patients underwent IONB were youngest than IC patients: median age were 66 years (range: 31-83) and 71 (range: 49-95) respectively. There were less females in the group of IONB (8.8%) in comparison with IC (22.3%). No significant differences were found in the pTNM – UICC stage (stage 0-I were 36.8% for IONB and 33.8% for IC) and in the median of follow-up (38 months, range: 3-247, and 35 months, range: 4-216) for IONB and IC groups. Patients with IC showed a significant worse in physical functioning (means: 80.8±22.2 and 74.7±24.8 respectively; p=0.006), in emotional functioning (means: 84.9±20.9 and 78.7±24.7; p=0.02), in cognitive functioning (means: 93.1±12.6 and 85.4±21.2; p=0.0002) in comparison with IONB. Patients with IC had high level of troubles in fatigue (means: 19.5±21.4 and 29.6±27.0; p=0.0006), in dyspnea (means: 12.9±22.1 and 20.5±27.1; p=0.007), in appetite loss (means: 6.7±17.2 and 14.2±27.5; p=0.01), in constipation (means: 16.0±21.4 and 31.5±34.7; p<0.0001), and abdominal bloating flatulence (means: 11.8±19.9 and 25.5±26.5; p<0.0001) in comparison with IONB. Discussion Cystectomy with any type of diversion remains a complication-prone surgery, nevertheless our results showed that IC showed higher troubles than IONB. Conclusions: This results are in favor of IONB as a the urinary diversion of choice.