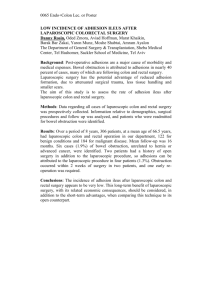
MIS rotation - Department of Obstetrics and Gynecology
advertisement

The Minimally Invasive Surgery Program The University of Michigan Department of Obstetrics and Gynecology Sawsan As-Sanie, MD, MPH Arleen Song, MD, MPH 1500 E. Medical Center Drive Women’s L4100, Box 0276 Ann Arbor, Michigan 48109-0276 PHONE: (734) 764-8429 FAX: (734) 647-9727 Educational Objectives for the Minimally Invasive Surgery (MIS) Rotation Submitted 9/8/08, updated 12/7/09. The overall objective of the MIS rotation is to provide the resident with a strong foundation in laparoscopic and hysteroscopic skills that would be necessary and expected of a generalist OBGYN after residency training. It is expected that the resident’s primary goal at the end of this rotation is to independently perform the wide range of laparoscopic procedures that should be offered by a general obgyn in either a community or academically-based clinical practice. In order to achieve these goals, the resident will participate in both the outpatient, intraoperative, and inpatient evaluation and management of MIS patients. The objectives of the outpatient portion of this rotation are to become competent in: (1) The evaluation and management of complex chronic pelvic pain patients, with a focus on the physical exam, differential diagnosis, and medical/surgical treatment options for women with chronic pelvic pain. (2) The preoperative evaluation of minimally invasive surgery candidates with a focus on how to determine best surgical approach (traditionally laparoscopy, Da Vinci-assisted laparoscopy, vaginal surgery vs. minilaparotomy). (3) The evaluation and management of postoperative complications seen in minimally invasive surgery. The objectives of the surgical portion of this rotation are listed below. Please note that this rotation will focus on a wide-range of advanced laparoscopic procedures, and will NOT be limited to Da Vinci-procedures only. 1. To provide the fundamental training in laparoscopic and hysteroscopic surgery. 2. To provide resident education in the basics of laparoscopy in areas such as correct patient positioning to prevent perioperative neuropathies, different ways of obtaining pneumoperitoneum, and correct port placement. 3. To expose the resident to advanced laparoscopy and operative hysteroscopy and have the resident assist in such procedures. Participation in advanced laparoscopic procedures is expected once the resident has demonstrated full understanding of the basic principles of laparoscopy and has demonstrated proficiency in basic laparoscopy. 4. To familiarize the resident with the daVinci system so that the resident will be able to select the appropriate patient for surgery, choose appropriate port placement, dock the da Vinci robotic system independently, and be proficient as the bedside-assistant in da Vinci cases. Proficiency as the bedside-assistant includes the appropriate manipulation of the uterine manipulator, as well as anticipating the needs of the primary surgeon with little direction or guidance. This will require thorough knowledge of the anatomy and steps of each type of surgical procedure. 5. Once the resident has shown proficiency in the above tasks, the goal would be familiarize the resident at the console. This will involve the following: a. Prior to the start of the MIS and GYN ONC rotation in the third year of residency, all GYN residents will receive didactic and dry lab training on the da Vinci Robotic Surgical System. All residents will first complete an online training program designed by Intuitive Surgical to familiarize surgeons with the da Vinci system. Following successful completion of the online training program, residents will participate in a one-on-one dry lab training session with an MIS and/or GYN ONC faculty. The dry lab training session will include modules to learn appropriate docking of the robotic device, manipulation of the robotic arms, dissection, transaction and suturing. An overview of the training modules is attached. These training modules are available at any time for any resident to practice on at their convenience once they have completed their formal dry-lab session. b. Once the resident has proven proficiency in the dry lab, the resident should be able to suture interrupted, figure-of-eight, and running sutures, as well as tie intracorporeal knots. These skills can be performed on a myomectomy case or closure of the vaginal cuff during a total laparoscopic hysterectomy. c. Once the resident has sufficiently exhibited proficiency in suturing and knot tying and has shown facility with basic maneuvering of the instruments, the resident will be able to spend more time at the console participating in lysis of adhesions and one side of a simple hysterectomy case. The goal will be for the fellow to perform one side of a hysterectomy, and the resident will complete the other side of a hysterectomy. 6. The OR time will be supplemented with the online tutorials and testing. 7. The resident will keep a case log. The case log should include a detailed description of the operative procedure and which portion of the case they participated in as primary surgeon, first assistant, vs. bed-side assistant. In order to achieve the objectives of the surgical and intraoperative portion of this rotation, residents may expect to achieve the following goals by the end of their residency training: **Please note that these are general guidelines. The level of involvement with each surgery will depend on the individual resident’s skill level, difficulty of case, and most importantly, the proficiency demonstrated by each individual resident as the rotation progresses. (1) To become proficient and truly independent in performing the following procedures: a. operative laparoscopy with lysis of mild to moderate adhesions b. excision and ablation of stage I, II, and some forms of stage III and IV endometriosis c. laparoscopic adnexal surgery including ovarian cystectomy, oophorectomy, and salpingectomy d. operative hysteroscopy with removal of endometrial polyps and submucosal fibroids e. minilaparotomy with TAH, myomectomy, adnexectomy f. total laparoscopic and laparoscopic supracervical hysterectomy of ≤12-14 week size uterus with minimal pelvic and bladder adhesions and/or endometriosis g. Da Vinci-assisted total laparoscopic and laparoscopic supracervical hysterectomy of ≤12-14 week size uterus with minimal pelvic and bladder adhesions and/or endometriosis (At the discretion of the attending physician, the resident will do one side and the MIS fellow will do the other side. The attending may intervene if difficulty is encountered.) (2) The resident will also be exposed to and participate in the following procedures. Based on the individual resident’s proficiency and progress in this rotation, he/she may have the opportunity to participate in all aspects of the following procedures over the course of the rotation. In doing so, he/she may become proficient and independent in performing the following procedures: a. Laparoscopic ureterolysis b. Laparoscopic excision or ablation of stage III or IV endometriosis (3) The resident will also be exposed to and participate in the following procedures according to their level of proficiency. However, due to the complexity of these cases, it is not expected that the resident be able to perform these procedures independently by the end of the rotation. These cases are considered fellow-level cases. a. Da Vinci-assisted total laparoscopic and supracervical hysterectomy of ≥16 week size uterus, any size uterus with severe pelvic or bladder adhesions and/or endometriosis b. Total laparoscopic and laparoscopic supracervical hysterectomy of ≥16 week size uterus, or any size uterus with severe pelvic or bladder adhesions and/or endometriosis c. (±Da Vinci-assisted) laparoscopic excision of ovarian remnant d. (±Da Vinci-assisted) laparoscopic trachelectomy e. Da Vinci-assisted laparoscopic myomectomy (the resident will participate in suturing the myoma bed. However, enucleation of the fibroid in most cases should be considered a fellow or attending-level portion of the procedure)