Russell_Langan_Whipple_80
advertisement
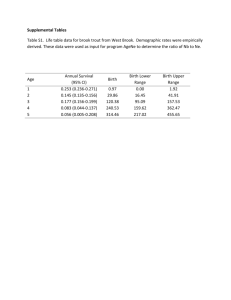
PANCREATICODUODENECTOMY IN THE OLDEST OF OLD: RESULTS BEYOND OPERATIVE MORTALITY Russell C. Langan, Weisheng Mao, Katherine Harris, Will Chapman, Charles Fehring, Peter R. Bucciarelli, Kesha Oza, Patrick G. Jackson, Thomas Fishbein, Reena Jha, Nadim Haddad, Firas Al-Kawas, John Carroll, Jane Hanna, Ann Parker, Waddah B. Al-Refaie, Lynt B. Johnson Department of Surgery, Radiology and Gastroenterology, Georgetown University Hospital, Washington, DC Introduction: The projected expansion of the elderly population may have significant implications on providers, hospital service lines and payers. Yet, there remains a paucity of data on the effect of the oldest old (≥ 80 years) on postpancreaticoduodenectomy (PD) outcomes beyond traditional operative mortality. We sought to assess potential differences in the index surgical hospitalization for patients over 80 years as compared to younger cohorts. Methods: We identified 99 patients who underwent PD between 2005 and 2013. Perioperative outcomes were compared across increasing age groups (I:≤ 70, II:71 – 79, III:≥ 80 years). Results: Median age was 66 years in cohort I, 74 years in the cohort II and 83 years in cohort III. Surgery was performed for malignancy in 75% of cohort I, 77% of cohort II and 90% of cohort III. Median tumor size, stage and estimated blood loss were equivalent across cohorts. There was no difference in the rate of pancreatic fistula, overall postoperative complications or 60-day readmission between cohorts. Length of stay (LOS) was significantly longer in cohort III as compared to cohort I (14.1 vs. 8.5 days; p = 0.0042) and trended toward significance in the cohort II vs. cohort I (13.7 vs. 8.5 days; p = 0.08). LOS was equivalent between the cohort II and cohort III. Increasing age was also significantly associated with discharge to a skilled facility (I: 6%, II: 13%, III: 27%; p = 0.02). Conclusions: Dogma states the oldest old will place significant strains on the existing healthcare system. However, we found perioperative outcomes and adverse events comparable between all age groups and no difference in LOS between septuagenarians and octogenarians. These results have future research and policy implications to overcome some of the challenges of this growing cohort of the US population. Larger studies should be performed on larger patient populations.