54 liposuction and body contouring
advertisement

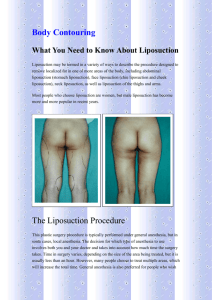
Body contouring Assessment of the body contouring patient History weight changes/ ideal weight eating disorders obstetric history and future babies previous abdo surgery general medical, smoking Examination fully undressed record height, weight circumference of pertinent body parts from behind- spinal curvature assymmetries, buttocks, fat rolls from sides and in front look for skin excess, skin laxity, fat distribution, abdominal scars pinch skin between fingers to determine fat amount and therefore suitability to liposuction NB the abdomen, hips, and subtrochanteric areas should have a pinch thickness of > 3 cm in order for the patient to benefit from liposuction. areas of normally little fat like ankles and calves, need at least 2cm of fat on pinch test to be of benefit -skin laxity test by lifting up the area of concern and seeing what happens to the wrinkles (the perceived fat excess may in fat just be skin laxity) FIG. 4A + B. Lifting skin and subcutaneous tissues over the hip area reduces trochanteric fullness, lifts the lower buttock, and eliminates surface irregularities by skin tightening. Ability to lift the skin 8–10 cm in this area and produce the illustrated visual changes indicates that the patient will benefit from an outer thigh lift. Procedures Liposuction is used to correct the majority of contour problems and surgery is seen as an adjunct. Surgery is indicated primarily for: 1. Skin laxity without significant fat deposits 2. Excessive skin laxity and cellulite, or buttock ptosis Surgical sequence consider postbariatric body-contouring surgery after at least 15 to 18 months or when their weight loss has plateaued for 3 to 6 months. 1. Central body lift and suction of flanks and thighs; 2. 3 to 6 months later: medial thigh lift and brachioplasty; 3. 3 to 6 months later: breast surgery (reduction/ mastopexy), with trunk liposuction if needed; and 4. 3 to 6 months later: facial rejuvenation. Thigh Lifts 2 groups of patients 1. those with classic lipodystrophy who have generous fat deposits on the trunk, thighs, and buttocks and who are disproportionately broader in the hips than in the rest of the body 2. those with generalized skin flaccidity in the medial and lateral thighs after massive weight loss. 2. According to Regnault, overweight patients showing a firm adiposity are not good candidates for surgery. The amount of tissue which can be removed safely is relatively small and the result is poor. . . . Firm adiposity may be accepted only in special cases, such as patients with trochanteric adiposity, where localized surgery is performed. 3. Grazer’s classification Type 1: medial thigh excess – SAL if good skin turgor, otherwise skin reduction Type 2: saddle bag trochanteric bulge (ecto and mesomorphs) – SAL Type 3: Saddle bag + additional bulge superiorly – SAL Type 4: Like type 3 with deepened midgluteal depression – SAL Type 5: Typical obesity pattern (endomorphs) – SAL or combined with reduction Type 6: traumatic or congenital – SAL surgery Type 7: Sagging and wrinkling due to aging – autologous fat to wrinkling and liposuction The pattern of deformity determines the specific technique to be used, whether semicircular, circular, longitudinal, or a combination of these. Many medial thigh lift techniques have been proposed over the years, but conventional (Pitanguy) techniques are prone to wide scars that migrate outside of swimsuit lines, vulvar distortion, and early relapse. The fascial anchoring technique(superficial fascial system) of Lockwood’s has reduced the frequency of these complications significantly. His modification consists of 1. suction lipectomy in the upper inner thigh 2. excision of a crescent of redundant skin 3. anchoring of the inferior thigh flap to the deep layer of the superficial perineal fascia (Colles’) without undermining or deepithelialization of the flaps. Lockwood Lower Body Lift 1 (1993) Preferred where patient has had previous abdominoplasty and a moderate to severe medial thigh problem. Operation -prep, drape, infiltrate, liposuck as req'd Preoperative marking for combined inner and outer thigh lift. Reference line (line of final closure) is thick black line. Thin black lines represent the expected upper and lower resection lines. Where the reference line and resection lines overlap, resection lines are white. Short vertical lines outline the bathing suit. Long vertical marks drawn at the anterior and posterior midlines and the left and right midaxillary lines to aid in symmetry of closure. A: Frontal view. The lower transverse pubic line is 5–7 cm from the anterior vulvar commissure when the skin is put on moderate upward stretch. The upper transverse line in the hypogastrium is the expected superior limit of resection. B: Note the Burow’s triangle excision at lower mid line to help reduce discrepancy between lengths of upper and lower lines. C: Most of skin resection will be below the reference line. D: Reference line and upper resection line are identical in the groin. The line of excision and the reference line end anterior to the buttocks fold so that subcutaneous fascia to, scar isfat notand visible fromdown behind. -incision is carried through the superficial layer of but not through, the deep subcutaneous layer of fat and fascia (Fig. 21). The deep subcutaneous layer is characterized by a darker, more orange fat and a looser, lamellar arrangement of fascial elements FIG. 21. Incising the superior limit of resection to the deep layer of superficial fascia over buttock and flank. The depth of the incision over the anterolateral abdomen is to the filmy innominate fascia just superficial to external oblique fascia. Although drawing shows medial thighs together, thighs should be held in abduction in order to reduce lateral skin tension (see Fig. 22). -Once the level of dissection is established, a flap is undermined in a caudal direction extending over the buttocks area, the iliac area, and the groin and anterior thigh. Dissection proceeds at least as far as the planned line of inferior resection. Over the lateral thigh, undermining may extend beyond the area of the greater trochanter. -the deep layer is several centimeters thick in the posterolateral area, but is rudimentary in the anterolateral area, and, for practical purposes, is absent over the external oblique fascia. -The flap is pulled in a cephalic direction, and a decision is made regarding how much of the flap should be excised FIG. 22. Flap is pulled in a superior direction, divided into segments, and held in place with penetrating towel clips while skin and subcutaneous tissues are excised. Usually the entire amount of the premarked area is removed. Additional flap mobility can be obtained by dissecting over the lower buttock and upper thigh distal to the greater trochanter, but as the extent of flap undermining increases, so does the incidence of postoperative seroma formation. -closure in layers -patient should then be turned to the right lateral decubitus position and the left side is treated in an identical fashion.symmetrical resection, tension etc -next the medial thigh lift is done FIG. 23. Patient positioning for medial thigh lift and excision of pubic-hypogastric skin segment. The knees are shoulder-width apart, and the hips are flexed 30 degrees. -prep, drape, infusion - groin incision is begun along the groin crease marking (most cephalic portion of specimen to be excised) and is carried up to the symphysis pubis and then laterally to join the lateral excision. In the groin, the depth of incision is to the fascia lata in the region between the ischial tuberosity and the symphysis pubis. The depth of incision becomes more superficial through the fat over the femoral triangle in order to leave lymphatics intact. As the incision proceeds laterally, its depth is to the innominate fascia just superficial to the external oblique aponeurosis FIG. 24. Dissection of the medial thigh and groin flap. Note the exposure of the muscle fascia in the area between the ischial tuberosity and the symphysis pubis. The flap over femoral triangle is thinner, preserving lymphatics and the external pudendal vessels. -Undermining of the flap is carried out in a caudal direction at the previously described levels of dissection. With the thighs slightly abducted and the knees flexed at 30 degrees, the skin flap of the upper medial thigh and groin area is put under moderate tension and excised. -closure- superficial fascial systemClosure in the groin is accomplished by suturing the superficial fascial system of the flap to the Colles fascia along the pubic ramus between the ischium and pubis. FIG. 25. Deep sutures in the Colles fascia at the upper wound edge and in the superficial fascial system (SFS) at the lower wound edge. Sutures over the femoral triangle are in SFS at both the upper and the lower wound edges. All sutures are placed before tying. -The deep sutures take all tension off the skin closure and prevent downward migration of the scar and eversion or distortion of the labia majora. Lockwood Lower Body Lift 2(1995) Medial Thigh Lift (Lockwood) Skin design (Green = liposuction) Combined with anchoring to Colles fascia Aftercare - 2–3 nights in the hospital. They are maintained in a thighs-abducted position with pillows between the knees and gradually ambulated starting the morning after surgery. - Although the patient may be unable to sit comfortably for approximately one week, voiding and bowel movements can be performed in a semi-standing position. Return to sedentary work activities is usually not until two weeks after surgery and sports are prohibited for six weeks. Complications As for abdominoplasty but include specifically 1. wound complications – medial thigh lifts highest of all the body contouring procedures (30-35%) 2. seroma – going too deep with groin excision 3. scar migration out of swimsuit lines 4. vulval distortion 5. contour irregularities Brachioplasty Goal of brachioplasty is to eliminate tissue redundancy and reduce circumference of the arm. Lockwood believes upper arm flabbiness is the direct result of 1) loosening of the connections of the arm superficial fascial system to the axillary fascia 2) relaxation of the axillary fascia itself, with age, weight fluctuations, and gravitational pull resulting in significant ptosis of the posteromedial arm. He proposes reanchoring of the posteromedial arm soft tissues to axillary fascia Teimourian(1998) classifies upper arm deformities into four groups: 1) Minimal to moderate fat and minimal skin laxity – treat with liposuction. 2) Generalized fat with moderate skin laxity - liposuction but may require excisional techniques. 3) Generalized obesity with extensive skin laxity - These patients benefit from a combination of circumferential liposuction and skin resection. 4) Minimal subcutaneous fat and extensive skin laxity - These patients are best treated with excisional techniques. To hide the scars, most recommend direct elliptical excision of the redundant tissue and place the incision medially along a line 2cm distal to the axillary crease(with or without z-plasties) to the medial epicondyle. Lockwood incision Line A=Line B+Line C Complications 1. highly visible scars 2. persistent vascular congestion, 3. edema and lymphedema from excessive skin 4. resection 5. wound necrosis -tension on closure, 6. cutaneousnerve injury from a dissection that strayed below 7. the superficial fascia. References A "bicycle-handlebar" type of incision for primary and secondary abdominoplasty. Aesthetic Plast Surg 1995 Jul-Aug;19(4):307-20 Baroudi R The authors register a revision of the literature regarding the types of low transversal pubic incisions used in abdominoplasty. Since 1987, the traditional open W-type incision changed to a new type called the bicycle handlebar. In this procedure, the pubic segment remains in a lower line at the level of the pubic hair, while the lateral limbs are in a high position. The anterior superior iliac spine is used as reference. Different types of procedures where the umbilical skin hole reaches the pubic incision are described and illustrated. This procedure is also used in secondary abdominoplasty. In all cases, the incision's new position should remain hidden under a bathing suit. Tumescent technique for regional anesthesia permits lidocaine doses of 35 mg/kg for liposuction. J Dermatol Surg Oncol 1990 Mar;16(3):248-63 Klein JA The tumescent technique for local anesthesia permits regional local anesthesia of the skin and subcutaneous tissues by direct infiltration. The tumescent technique uses large volumes of a dilute anesthetic solution to produce swelling and firmness of targeted areas. This investigation examines the absorption pharmacokinetics of dilute solutions of lidocaine (0.1% or 0.05%) and epinephrine (1:1,000,000) in physiologic saline following infiltration into subcutaneous fat of liposuction surgery patients. Plasma lidocaine concentrations were measured repeatedly over more than 24 hours following the infiltration. Peak plasma lidocaine levels occurred 12-14 hours after beginning the infiltration. Clinical local anesthesia is apparent for up to 18 hours, obviating the need for postoperative analgesia. Dilution of lidocaine diminishes and delays the peak plasma lidocaine concentrations, thereby reducing potential toxicity. Liposuction reduces the total amount of lidocaine absorbed systemically, but does not dramatically reduce peak plasma lidocaine levels. A safe upper limit for lidocaine dosage using the tumescent technique is estimated to be 35 mg/kg. Infiltrating a large volume of dilute epinephrine assures diffusion throughout the entire targeted area while avoiding tachycardia and hypertension. The associated vasoconstriction is so complete that there is virtually no blood loss with liposuction. The tumescent technique can be used with general anesthesia or IV sedation. However, with appropriate instrumentation and surgical method, the tumescent technique permits liposuction of large volumes of fat totally by local anesthesia, without IV sedation or narcotic analgesia. High-lateral-tension abdominoplasty with superficial fascial system suspension [see comments] Plast Reconstr Surg 1995 Sep;96(3):603-15 Lockwood T Modern abdominoplasty techniques were developed in the 1960s. The advent of liposuction has reduced the need for classic abdominoplasty and allowed more aesthetic sculpting of the entire trunk. However, the combination of significant truncal liposuction and classic abdominoplasty is not recommended due to the increased risk of complications. Although the surgical principles of classic abdominoplasty certainly have stood the test of time, they are based on two theoretical assumptions that may be proved to be inaccurate. The first assumption is that wide direct undermining to costal margins is essential for abdominal flap advancement. In fact, discontinuous undermining allows effective loosening of the abdominal flap while preserving vascular perforators. The second inaccurate assumption is that with aging and weight fluctuations (including pregnancy), abdominal skin relaxation occurs primarily in the vertical direction from the xiphoid to the pubis. This is true in the lower abdomen, but in most patients a strong superficial fascial system adherence to the linea alba in the epigastrium limits vertical descent. Epigastric laxity frequently results from a progressive horizontal loosening due to relaxation of the tissue along the lateral trunk. Experience with the lower-body lift procedure has shown that significant lateral truncal skin resection results in epigastric tightening. In these patients, the ideal abdominoplasty pattern would resect as much or more laterally than centrally, leading to more natural abdominal contours. Fifty patients who underwent high-lateral-tension abdominoplasty with and without significant truncal liposuction and other aesthetic procedures were followed for 4 to 16 months. The primary indication for surgery was moderate to severe laxity of abdominal skin and muscle with or without truncal fat deposits. Complication rates were equal to or less than those of historical controls and did not increase with significant adjunctive liposuction. The key technical elements of this procedure include direct undermining limited to the paramedian area, discontinuous undermining to costal margins and flanks as needed, skin resection pattern with significant lateral resection and highest-tension wound closure placed laterally, superficial fascial system repair with permanent sutures along the entire incision, and liberal use of adjunctive liposuction in the upper abdomen and the lateral and posterior trunk. Tumescent liposuction. A surgeon's perspective. Clin Plast Surg 1996 Oct;23(4):633-41; discussion 642-5 Pitman GH The tumescent technique consists of injection of large amounts of dilute lidocaine and epinephrine into the subcutaneous fat prior to performing liposuction. This preinjection provides local anesthesia and reduction in postoperative pain. Blood loss, bruising, and swelling are significantly reduced. The large volume of injectate is a complete fluid replacement, eliminating the need for intravenous fluid support. In the authors' experience, patients are most comfortable when the tumescent technique is combined with monitored intravenous sedation.